Cdc Report on Tb in Prisons - 2006
Download original document:
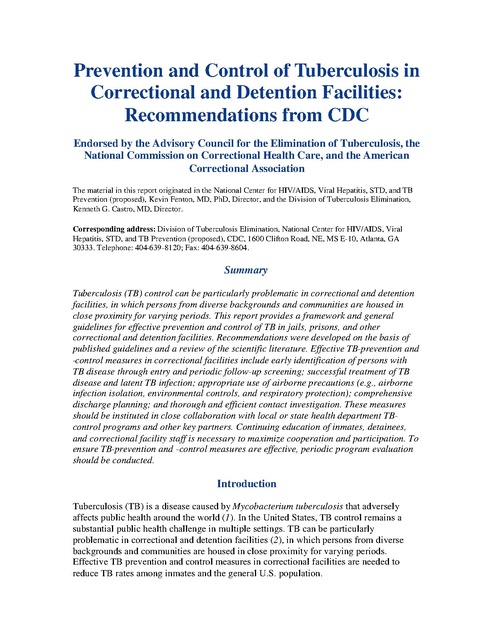
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
Prevention and Control of Tuberculosis in Correctional and Detention Facilities: Recommendations from CDC Endorsed by the Advisory Council for the Elimination of Tuberculosis, the National Commission on Correctional Health Care, and the American Correctional Association The material in this report originated in the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (proposed), Kevin Fenton, MD, PhD, Director, and the Division of Tuberculosis Elimination, Kenneth G. Castro, MD, Director. Corresponding address: Division of Tuberculosis Elimination, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (proposed), CDC, 1600 Clifton Road, NE, MS E-10, Atlanta, GA 30333. Telephone: 404-639-8120; Fax: 404-639-8604. Summary Tuberculosis (TB) control can be particularly problematic in correctional and detention facilities, in which persons from diverse backgrounds and communities are housed in close proximity for varying periods. This report provides a framework and general guidelines for effective prevention and control of TB in jails, prisons, and other correctional and detention facilities. Recommendations were developed on the basis of published guidelines and a review of the scientific literature. Effective TB-prevention and -control measures in correctional facilities include early identification of persons with TB disease through entry and periodic follow-up screening; successful treatment of TB disease and latent TB infection; appropriate use of airborne precautions (e.g., airborne infection isolation, environmental controls, and respiratory protection); comprehensive discharge planning; and thorough and efficient contact investigation. These measures should be instituted in close collaboration with local or state health department TBcontrol programs and other key partners. Continuing education of inmates, detainees, and correctional facility staff is necessary to maximize cooperation and participation. To ensure TB-prevention and -control measures are effective, periodic program evaluation should be conducted. Introduction Tuberculosis (TB) is a disease caused by Mycobacterium tuberculosis that adversely affects public health around the world (1). In the United States, TB control remains a substantial public health challenge in multiple settings. TB can be particularly problematic in correctional and detention facilities (2), in which persons from diverse backgrounds and communities are housed in close proximity for varying periods. Effective TB prevention and control measures in correctional facilities are needed to reduce TB rates among inmates and the general U.S. population. The recommendations provided in this report for the control of TB in correctional facilities expand on, update, and supersede recommendations issued by the Advisory Council for the Elimination of TB (ACET) in 1996 (3). This report provides a framework and general guidelines for effective prevention and control of TB in jails, prisons, and other correctional and detention facilities. In addition, on the basis of existing scientific knowledge and applied experience of correctional and public health officials, this report defines the essential activities necessary for preventing transmission of M. tuberculosis in correctional facilities. These fundamental activities can be categorized as 1) screening (finding persons with TB disease and latent TB infection [LTBI]); 2) containment (preventing transmission of TB and treating patients with TB disease and LTBI); 3) assessment (monitoring and evaluating screening and containment efforts); and 4) collaboration between correctional facilities and public health departments in TB control. These overarching activities are best achieved when correctional facility and public health department staff are provided with clear roles of shared responsibility. The recommendations in this report can assist officials of federal, state, and local correctional facilities in preventing transmission of TB and controlling TB among inmates and facility employees. The target audience for this report includes public health department personnel, correctional medical directors and administrators, private correctional health vendors, staff in federal and state agencies, staff in professional organizations, and health-care professionals. The report is intended to assist policymakers in reaching informed decisions regarding the prevention and control of TB in correctional facilities. Methods To update the existing guidelines, with assistance from ACET, CDC organized and convened the Tuberculosis in Corrections Working Group, an ad hoc group of persons with expertise in public health and health care in correctional facilities. Organizations represented in the Working Group included ACET, the National Commission on Correctional Health Care, the American Correctional Association, the American Jail Association, and the Society of Correctional Physicians. The Working Group reviewed published guidelines and recommendations, published and unpublished policies and protocols, and peer-reviewed studies discussing overall TB prevention and control and aspects of TB prevention and control specific to correctional and detention facilities. These guidelines, recommendations, policies, protocols, and studies form the basis for the Working Group's recommendations. Because controlled trials are lacking for TB prevention and control activities and interventions specific to correctional and detention facilities, the recommendations have not been rated on the quality and quantity of the evidence. The recommendations reflect the expert opinion of the Working Group members with regard to best practices, based on their experience and their review of the literature. Summary of Changes from Previous Recommendations These guidelines are intended for short- and long-term confinement facilities (e.g., prisons, jails, and juvenile detention centers), which are typically referred to as correctional facilities throughout this report. These recommendations differ as follows from those made in 1996: The target audience has been broadened to include persons working in jails and other detention facilities. The need for correctional and detention facilities to base screening procedures for inmates and detainees on assessment of their risk for TB is emphasized. A description of how TB risk should be assessed is included. The need for institutions to conduct a review of symptoms of TB for all inmates and detainees at entry is discussed. The need for all inmates and detainees with suspected TB to be placed in airborne infection isolation (AII) immediately is emphasized. Testing recommendations have been updated to reflect the development of the QuantiFERON®-TB Gold test (QFT-G), a new version of the QuantiFERON®-TB (QFT) diagnostic test for M. tuberculosis infection. The section on environmental controls has been expanded to cover local exhaust ventilation, general ventilation, air cleaning, and implementation of an environmental control program. Ventilation recommendations for selected areas in new or renovated correctional facilities have been included. A section on respiratory protection has been added, including information on implementing respiratory protection programs. Treatment recommendations for TB and LTBI have been updated on the basis of the most recent treatment statements published by CDC, the American Thoracic Society (ATS), and the Infectious Diseases Society of America. Emphasis is placed on case management of inmates with TB disease and LTBI. The need for early discharge planning coordinated with local public health staff is emphasized. A section has been included on U.S. Immigration and Customs Enforcement detainees. The importance of collaboration between correctional facility and public health staff is emphasized, particularly with respect to discharge planning and contact investigation. The need for corrections staff to work closely with public health staff to tailor an appropriately comprehensive training program to achieve and sustain TB control in a correctional facility is emphasized. The need for public health workers to receive education regarding the correctional environment is emphasized. Program evaluation is emphasized. Recommended areas of evaluation include assessment of TB risk in the facility, performance measurement for quality improvement, collaboration, information infrastructure, and using evaluation information to improve the TB-control program. Background During 1980--2003, the number of incarcerated persons in the United States increased fourfold, from approximately 500,000 in 1980 to approximately 2 million in 2003 (4,5). A disproportionately high percentage of TB cases occur among persons incarcerated in U.S. correctional facilities. In 2003 at midyear, although 0.7% of the total US population was confined in prisons and jails, 3.2% of all TB cases nationwide occurred among residents of correctional facilities (6). Although overall incidence of new TB cases among the U.S. population has remained at <10 cases per 100,000 persons since 1993 (6), substantially higher case rates have been reported in correctional populations (2). For example, the incidence of TB among inmates in New Jersey during 1994 was 91.2 cases per 100,000 inmates, compared with 11.0 cases per 100,000 persons among all New Jersey residents (3). In 1991, a TB case rate for inmates of a California prison was 184 cases per 100,000 persons, which was 10 times greater than the statewide rate (7). In addition, in 1993, the TB rate for inmates in the New York State correctional system was 139.3 cases per 100,000 persons, an increase from the rate of 15.4 during 1976--1978 (3,8). In California, the TB case rate reported from an urban jail in a high-prevalence area was 72.1 cases per 100,000 inmates in 1998, representing 10% of the county's cases in that year (9). Studies have demonstrated the prevalence of LTBI among inmates to be as high as 25% (10--14). Other studies have demonstrated a correlation between length of incarceration and positive tuberculin skin test (TST) response, indicating that transmission might have occurred in these facilities (15,16). At least three factors contribute to the high rate of TB in correctional and detention facilities. First, disparate numbers of incarcerated persons are at high risk for TB (e.g., users of illicit substances [e.g., injection drugs], persons of low socioeconomic status, and persons with human immunodeficiency virus [HIV] infection). These persons often have not received standard public health interventions or nonemergency medical care before incarceration. Second, the physical structure of the facilities contributes to disease transmission, as facilities often provide close living quarters, might have inadequate ventilation, and can be overcrowded (9,17--19). Third, movement of inmates into and out of overcrowded and inadequately ventilated facilities, coupled with existing TB-related risk factors of the inmates, combine to make correctional and detention facilities a highrisk environment for the transmission of M. tuberculosis and make implementation of TB-control measures particularly difficult (19). Despite recent efforts to improve TBcontrol measures in correctional and detention facilities, outbreaks of TB continue to occur in these settings, and TB disease has been transmitted to persons living in nearby communities (20--22). Consequently, correctional and detention facilities are critical settings in which to provide interventions for detecting and treating TB among a vulnerable population. Addressing the Challenges of TB Control in Correctional Facilities Published recommendations for elimination of TB in the United States include testing and treating inmates in correctional facilities for LTBI to prevent the development and transmission of TB (23). The basis for this recommendation is that LTBI and coinfection with HIV are more common in these underserved populations than in the general population (24--26). However, treating correctional inmates for LTBI can be challenging. Before being incarcerated, inmates might have faced barriers to accessing community health services necessary for the detection and treatment of TB disease and LTBI (27). In addition, inmates released from correctional facilities often do not attend clinic visits or adhere to treatment regimens. One study of inmates released before completion of TB therapy indicated that only 43% made at least one visit to the clinic after release (28). In another jail setting, using an educational intervention increased the rate of clinic visits after release from 3% to only 23% (29). In the United States, TB is concentrated increasingly among the most disadvantaged populations, particularly immigrants (30). Detained immigrants are arriving largely from countries with a high prevalence of TB (e.g., Mexico, the Philippines, and Vietnam) and therefore present unique challenges in the elimination of TB in the United States* (31). Social and legal barriers often make standard testing and treatment interventions inadequate among undocumented immigrants (31). In certain instances, these patients have become resistant to first-line anti-TB drugs because of the interrupted treatment received in their countries of origin (32). However, undocumented immigrants placed in detention and correctional facilities have an opportunity to receive TB screening and begin treatment for TB disease (33). Rationale for Updating and Strengthening TB Control and Prevention Guidelines Transmission of M. tuberculosis continues to be documented within correctional facilities, primarily as a result of undiagnosed TB. Inmates with undiagnosed TB disease place other inmates and correctional staff at risk for TB, and when released, these persons also can infect persons living in surrounding communities (16,17,20,21,22,34,35). Despite the continued transmission of TB in correctional settings, few comprehensive evaluations of the implementation of TB-detection and -control procedures in correctional facilities have been performed (36--38). Nevertheless, correctional facilities are increasingly basing their TB prevention and control procedures on studies and data that support judicious interventions, including screening, case finding, case management, outbreak and contact investigations, and treatment for LTBI (7,9,14,21,28,33,34,39--46). Improving TB prevention and control practices within these settings is necessary to reduce rates of disease and eventually eliminate TB. TB prevention and control practices within correctional facilities should be strengthened for multiple reasons: M. tuberculosis is spread through the air. One highly infectious person can infect inmates, correctional staff, and visitors who share the same air space. Immediate isolation of infectious patients can interrupt transmission of M. tuberculosis in the facility. † Prompt initiation of an adequate regimen of directly observed therapy (DOT) helps ensure adherence to treatment because a health-care professional, a specially trained correctional officer, or a health department employee observes the patient swallowing each dose of medication. This method of treatment can diminish infectiousness, reduce the risk for relapse, and help prevent the development of drug-resistant strains of M. tuberculosis. Inmates of correctional facilities have been reported to have relatively high rates of HIV infection; persons who are coinfected with HIV and M. tuberculosis are at high risk for progressing from LTBI to TB disease. A completed regimen of treatment for LTBI can prevent the development of TB disease in persons who are infected with M. tuberculosis. Correctional facility officials have an opportunity to treat inmates who have TB disease or LTBI before such inmates are released into the community. Because a substantial proportion of inmates do not have any other access to the health-care system, the correctional setting can be a primary source of health information, intervention, and maintenance. Screening Early identification and successful treatment of persons with TB disease remains the most effective means of preventing disease transmission (47). Therefore, inmates who are likely to have infectious TB should be identified and begin treatment before they are integrated into the general correctional facility population (i.e., at the time of admission into the correctional system). When possible, newly arrived inmates should not be housed with other inmates until they have been appropriately screened for TB disease. Screening programs in the correctional setting also allow for the detection of substantial numbers of persons with LTBI who are at high risk for progressing to TB disease and would likely benefit from a course of treatment. This secondary benefit of screening programs is often limited by inability to initiate and ensure completion of LTBI treatment, particularly in short-term correctional facilities. In addition to screening at intake, routine (i.e., at least annual) screening of long-term inmates and correctional facility staff (e.g., custody and medical) should be incorporated into the TB-control program (48,49). How screening activities should be implemented depends on multiple factors, including 1) the type of facility, 2) the prevalence of TB infection and disease in the facility, 3) the prevalence of TB in the inmates' communities, 4) the prevalence of other risk factors for TB (e.g., HIV) in the inmate population, and 5) the average length of stay of inmates in the facility. The type of screening recommended for a particular facility is determined by an assessment of the risk for TB transmission within that facility. The risk assessment should be performed at least annually and should be made in collaboration with the local or state health department. A facility's TB risk can be defined as being minimal or nonminimal. A facility has minimal TB risk if no cases of infectious TB have occurred in the facility in the last year, the facility does not house substantial numbers of inmates with risk factors for TB (e.g., HIV infection and injection-drug use), the facility does not house substantial numbers of new immigrants (i.e., persons arriving in the United States within the previous 5 years) from areas of the world with high rates of TB, and employees of the facility are not otherwise at risk for TB. Any facility that does not meet these criteria should be categorized as a nonminimal TB risk facility. Screening Methods Symptom Screening Whenever possible, health-care professionals should perform the initial screening. However, correctional officers in jails (particularly those housing minimal numbers of inmates) frequently administer health intake questionnaires. If custody staff members conduct the intake screening, they should receive adequate periodic training in taking a medical history, making necessary observations, and determining the appropriate disposition of inmates with signs or symptoms of possible medical problems. Staff conducting medical intake should receive appropriate counseling and education regarding medical confidentiality. During their initial medical screening, inmates should be asked if they have a history of TB disease or if they have been treated for LTBI or TB disease previously. Documentation of any such history should be obtained from medical records, if possible. Inmates should be observed for the presence of a cough or evidence of significant weight loss. All incoming inmates in any size jail, prison, or other detention facility (e.g., immigration enforcement) should be immediately screened for symptoms of pulmonary TB by being asked if they have had a prolonged cough (i.e., one lasting >3 weeks), hemoptysis (i.e., bloody sputum), or chest pain. The index of suspicion should be high when pulmonary symptoms are accompanied by general, systemic symptoms of TB (e.g., fever, chills, night sweats, easy fatigability, loss of appetite, and weight loss). Inmates should be interviewed systematically (i.e., using a standardized questionnaire) to determine whether they have experienced symptoms in recent weeks. Inmates who have symptoms suggestive of TB disease should immediately receive a thorough medical evaluation, including a TST or QFT-G, a chest radiograph, and, if indicated, sputum examinations. Persons with symptoms suggestive of TB disease or with a history of inadequate treatment for TB disease should be immediately placed in an AII room§ until they have undergone a thorough medical evaluation. If deemed infectious, such persons should remain in isolation until treatment has rendered them noninfectious. Facilities without an on-site AII room should have a written plan for referring patients with suspected or confirmed TB to a facility that is equipped to isolate, evaluate, and treat TB patients. Symptom screening alone is an unsatisfactory screening mechanism for TB, except in facilities with a minimal risk for TB transmission. The use of symptom screening alone often will fail to detect pulmonary TB in inmates. Chest-Radiograph Screening Screening with chest radiographs can be an effective means of detecting new cases of unsuspected TB disease at intake to a correctional facility. In addition, radiographic screening requires fewer subsequent visits than a TST (i.e., only those inmates with suspicious radiographs or TB symptoms require follow-up). However, such screening will not identify inmates with LTBI. One study demonstrated that screening inmates with a chest radiograph doubled the TB case-finding rate and reduced the time from intake into the correctional facility to isolation substantially compared with TST testing (2.3 days and 7.5 days, respectively), thereby reducing the risk for TB exposure for other inmates and staff (50). Digital radiographs (miniature or full-size) provide enhanced imaging and improved storage and readability. A miniature radiograph can be performed in <1 minute and exposes the patient to approximately one tenth the radiation dose of a conventional radiograph. One cost-effectiveness analysis of miniature chest radiography for TB screening on admission to jail indicated that more cases were detected with this method than either TST or symptom screening, and the cost of radiograph screening was less per case detected (51). The extent to which radiologic screening is used in a given institution should be dictated by multiple factors, including 1) local epidemiologic characteristics of TB disease; 2) inmate length of stay; 3) the ability of the health-care professionals within the facility to conduct careful histories, tuberculin skin or QFT-G testing, and cross-matches with state TB registries; and 4) timeliness of the radiographic study and its reading. Screening with chest radiographs might be appropriate in certain jails and detention facilities that house substantial numbers of inmates for short periods and serve populations at high risk for TB (e.g., those with high prevalence of HIV infection or history of injection-drug use and foreign-born persons from countries in which TB prevalence is high). Inmates who are infected with HIV might be anergic and consequently might have falsenegative TST results. However, routine anergy panel testing is not recommended because it has not been demonstrated to assist in diagnosing or excluding LTBI (52). In facilities that do not perform routine radiographic screening for all inmates, a chest radiograph should be part of the initial screening of HIV-infected patients and those who are at risk for HIV infection but whose status is unknown. In facilities with on-site radiographic screening, the chest radiograph should be performed as part of intake screening and read promptly by a physician, preferably within 24 hours. Persons who have radiographs suggestive of TB should be isolated immediately and evaluated further. Sputum-smear and culture examinations should be performed for inmates whose chest radiographs are consistent with TB disease and might be indicated for at least certain persons who are symptomatic, regardless of their TST, QFT-G, or chest radiograph results because persons with HIV and TB disease might have "negative" chest radiographs in addition to false-negative TST or QFT-G results. Mantoux TST Screening Tuberculin skin testing using 0.1 mL of 5 tuberculin units (TU) of purified protein derivative (PPD) is the most common method of testing for TB infection. Multiplepuncture tests (e.g., the tine test) should not be used to determine whether a person is infected. Persons who have a documented history of a positive TST result (with a millimeter [mm] reading), a documented history of TB disease, or a reported history of a severe necrotic reaction to tuberculin should be exempt from a routine TST. For persons with a history of severe necrotic reactions and without a documented positive result with a millimeter reading, a QFT-G may be substituted for the TST. Otherwise, such persons should be screened for symptoms of TB and receive a chest radiograph unless they have had one recently (i.e., within 6 months) and are not symptomatic. Pregnancy, lactation, or previous vaccination with Bacillus Calmette-Guerin (BCG) vaccine are not contraindications for tuberculin skin testing. The TST is not completely sensitive for TB disease; its sensitivity ranges from 75%--90% (53,54). Despite this limitation, skin testing, along with use of a symptom review, frequently constitutes the most practical approach to screening for TB disease. A trained health-care professional should place the TST and interpret the reaction 48--72 hours after the injection by measuring the area of induration (i.e., the palpable swelling) at the injection site. The diameter of the indurated area should be measured across the width of the forearm. Erythema (i.e., the redness of the skin) should not be measured. All reactions, even those classified as negative, should be recorded in millimeters of induration. In the majority of cases, a TST reaction of >10 mm induration is considered a positive result in inmates and correctional facility employees. However, an induration of >5 mm is considered a positive result in the following persons: persons infected with HIV, persons who are recent contacts of patients with TB disease, persons with fibrotic changes on chest radiograph consistent with previous TB disease, organ transplant recipients and patients with other immunocompromising conditions (e.g., persons receiving >15 mg/day of prednisone for >1 month), and persons suspected of having TB disease. Persons who have a positive TST result and no symptoms suggestive of TB disease should be evaluated with a chest radiograph within 72 hours after the skin test is interpreted. Persons who have symptoms suggestive of TB disease should be evaluated immediately and placed in an AII room until TB is ruled out (see Symptom Screening). The use of two-step testing can reduce the number of positive TSTs that would otherwise be misclassified as recent skin-test conversions during future periodic screenings. Certain persons who were infected with M. tuberculosis years earlier exhibit waning delayed-type hypersensitivity to tuberculin. When they are skin tested years after infection, they might have a false-negative TST result (even though they are truly infected). However, this first skin test years after the infection might stimulate the ability to react to subsequent tests, resulting in a "booster" reaction. When the test is repeated, the reaction might be misinterpreted as a new infection (recent conversion) rather than a boosted reaction. For two-step testing, persons whose baseline TSTs yield a negative result are retested 1--3 weeks after the initial test. If the second test result is negative, they are considered not infected. If the second test result is positive, they are classified as having had previous TB infection. Two-step testing should be considered for the baseline testing of persons who report no history of a recent TST and who will receive repeated TSTs as part of an institutional periodic skin-testing program. In the majority of cases, a two-step TST is not practical in jails because of the short average length of stay of inmates. In the past, a panel of other common antigens was often applied with the TST to obtain information regarding the competence of the patient's cellular immune system and to identify anergy. More recently, however, anergy testing has been demonstrated to be of limited usefulness because of problems with standardization and reproducibility, the low risk for TB associated with a diagnosis of anergy, and the lack of apparent benefit of preventive therapy for groups of anergic HIV-infected persons. Therefore, the use of anergy testing in conjunction with a TST is no longer recommended routinely for screening programs for M. tuberculosis infection in the United States (52). Intracutaneous inoculation with BCG is currently used worldwide as a vaccine against TB. BCG is a live attenuated Mycobacterium bovis strain that stimulates the immune system to protect against TB. No reliable method has been developed to distinguish TST reactions caused by vaccination with BCG from those caused by natural mycobacterial infections, although reactions of >20 mm of induration are not likely caused by BCG (55). TST is not contraindicated for persons who have been vaccinated with BCG, and the TST results of such persons are used to support or exclude the diagnosis of M. tuberculosis infection. A diagnosis of M. tuberculosis infection and treatment for LTBI should be considered for any BCG-vaccinated person who has a positive TST reaction. The same criteria for interpretation of TST results are used for both BCG-vaccinated and nonvaccinated persons (56). QuantiFERON®-TB Gold Test In May 2005, the U.S. Food and Drug Administration (FDA) licensed QFT-G. This invitro diagnostic test measures the amount of interferon-gamma produced by cells in whole blood that have been stimulated by mycobacterial peptides. The peptides used in the test mimic proteins known as ESAT-6 and CFP-10, which are present in M. tuberculosis but absent from all BCG strains and from the majority of commonly encountered non-TB mycobacteria. The test is intended for use as a diagnostic tool for M. tuberculosis infection, including both TB disease and LTBI. As with a TST, QFT-G cannot distinguish between LTBI and TB disease and should be used in conjunction with risk assessment, radiography, and other diagnostic evaluations. The advantages of QFT-G compared with TST are that 1) results can be obtained after a single patient visit, 2) the variability associated with skin-test reading can be reduced because "reading" is performed in a qualified laboratory, and 3) QFT-G is not affected by previous BCG vaccination and eliminates the unnecessary treatment of persons with false-positive results. QFT-G does not affect the result of future QFT-G tests (i.e., no "boosting" occurs). Limitations of the test include the need for phlebotomy, the need to process blood specimens within 12 hours of collection for the most recent version of the test, the limited number of laboratories that process the test, and a lack of clinical experience in interpreting test results. The elimination of the second visit for reading the TST, however, is likely to render the QFT-G competitive in cost-benefit considerations. Although the performance of QFT-G has not been evaluated sufficiently in select populations of interest (e.g., HIV-infected persons), available data indicate that QFT-G is as sensitive as TST for detection of TB disease and more specific than TST for detection of LTBI (57,58). CDC guidelines for QFT-G recommend that QFT-G can be used in place of TST in all circumstances in which TST is currently used (58). This includes initial and periodic TB screening for correctional facility inmates and employees and testing of exposed persons in contact investigations. Because data are insufficient regarding performance of QFT-G in certain clinical situations, as with a negative TST result, a negative QFT-G result alone might not be sufficient to exclude M. tuberculosis infection in these situations. Examples of such clinical scenarios include those involving patients with severe immunosuppression who have had recent exposure to a patient with TB and patients being treated or about to undergo treatment with potent tumor necrosis factor alpha (TNF-a) antagonists. Use of Local Health Department TB Registry Correctional facilities and local health departments should collaborate to ensure effective TB screening in the correctional setting. Inmates might provide inaccurate information on admission for multiple reasons, ranging from forgetfulness and confusion to deliberate misrepresentation. Health departments should perform cross-matches with the local TB registry and search for matches on known aliases, birth dates, maiden names, and other personal information for inmates suspected of having TB infection. A readily accessible record of previous TB history, drug-susceptibility patterns, treatment, and compliance can be useful in determining the disposition of a given patient with suspected TB. Initial Screening The following procedures should be used for the initial screening of inmates and detainees (depending on their length of stay in the facility and the type of facility) and for all correctional facility employees, regardless of the type of facility. Inmates in Minimal TB Risk Facilities Inmates in all minimal TB risk correctional and detention facilities should be evaluated on entry for symptoms of TB. Persons with symptoms of TB should be evaluated immediately to rule out the presence of infectious disease and kept in an AII room until they are evaluated. If the facility does not have an AII room, the inmate should be transported to a facility that has one. In addition, all newly arrived inmates should be evaluated for clinical conditions and other factors that increase the risk for infection or the risk for progressing to TB disease, including the following: HIV infection, recent immigration, history of TB, recent close contact with a person with TB disease, injection-drug use, diabetes mellitus, immunosuppressive therapy, hematologic malignancy or lymphoma, chronic renal failure, medical conditions associated with substantial weight loss or malnutrition, or history of gastrectomy or jejunoileal bypass. Persons with any of these conditions require further screening with a TST, a QFT-G, or a chest radiograph within 7 days of arrival. Regardless of the TST or QFT-G result, inmates known to have HIV infection or other severe immunosuppression, and those who are at risk for HIV infection but whose HIV status is unknown, should have a chest radiograph taken as part of the initial screening. Persons who have an abnormal chest radiograph should be further evaluated to rule out TB disease; if TB disease is excluded as a diagnosis, LTBI therapy should be considered if the TST or QFT-G result is positive. Inmates in Nonminimal TB Risk Prisons Immediately on arrival, all new inmates should be screened for symptoms, and any inmate with symptoms suggestive of TB should be placed in an AII room and evaluated promptly for TB disease. If the facility does not have an AII room, the inmate should be transported to a facility that has one. Inmates who have no symptoms require further screening with a TST, a QFT-G, or a chest radiograph within 7 days of arrival. Regardless of their TST or QFT-G status, inmates known to have HIV infection or other severe immunosuppression, and those who are at risk for HIV infection but whose HIV status is unknown, should have a chest radiograph taken as part of the initial screening. Persons who have an abnormal chest radiograph should be further evaluated to rule out TB disease; if TB disease is excluded as a diagnosis, LTBI therapy should be considered if the TST or QFT-G result is positive. As the rate of TB disease in the United States has decreased, identification and treatment of persons with LTBI who are at high risk for TB disease have become essential components of the TB elimination strategy promoted by ACET (59). Targeted testing using the TST or QFT-G identifies persons at high risk for TB disease who would benefit from treatment for LTBI. Prisons offer an excellent public health opportunity for identifying persons at high risk for TB who can be screened for TB infection and placed on LTBI therapy, if indicated. If the TST is used, a two-step testing procedure should be strongly considered when obtaining a baseline reading. A single step QFT-G is an adequate baseline. Inmates with a positive test should be evaluated for LTBI therapy after TB disease is excluded. Inmates in Nonminimal TB Risk Jails and Other Short-Term Detention Facilities As in prisons, all new detainees in nonminimal TB risk jails should be screened on entry for symptoms, and any detainee who has symptoms suggestive of TB should be placed immediately in an AII room and evaluated promptly for TB disease. If the facility does not have an AII room, the inmate should be transported promptly to a facility that does have one. Detainees without symptoms require further screening with a TST, a QFT-G, or a chest radiograph within 7 days of arrival. Regardless of the TST or QFT-G result, detainees known to have HIV infection, and those who are at risk for HIV infection but whose HIV status is unknown, should have a chest radiograph taken as part of the initial screening. Persons who have a positive result should be further evaluated to rule out TB disease. The primary purpose of screening in correctional settings is to detect TB disease. TST or QFT-G screening in jails to initiate LTBI therapy often is not practical because of the high rate of turnover and short lengths of stay. Although not all jail detainees have short lengths of stay, determining which detainees will be in the jail for a long term is difficult. Nationwide, approximately half of persons detained in local jails are released within 48 hours of admission. Thus, even if all detainees can be tested at intake, a large proportion will be unavailable to have their TSTs read or to be evaluated when QFT-G test results are available. Of those still in custody, a substantial percentage will be released before the radiographic and medical evaluation is completed. In a 1996 study, 43% of detainees at a county jail in Illinois who had a positive TST result were released or transferred before their evaluation could be completed (3). A substantial proportion of detainees who are incarcerated long enough to begin LTBI therapy will be released before completion of treatment. A San Francisco study indicated that approximately 62% of detainees who were started on LTBI treatment were released before completion (40). These data illustrate the challenges of implementing a testing and treatment program for LTBI in jails with highly dynamic detainee populations. Certain jails have adopted a targeted approach of performing TSTs only on new detainees who are at high risk for TB disease (e.g., detainees with known HIV infection). Screening for TB and treating LTBI are most effective within the jail setting if resources dedicated to discharge planning and reliable access to community-based treatment are available. Modest interventions (e.g., education and incentives [see Glossary]) in the jail setting can lead to improvements in linking released detainees to postrelease medical care and increase the likelihood that therapy will be completed (60,61). Persons in Holding or Booking Facilities City, county, and other law enforcement authorities frequently have facilities that hold arrestees and detainees for short periods of time, ranging from hours to multiple days. TB symptom screening is recommended for all persons at the time of entry into these facilities. Any detainee who has symptoms suggestive of TB should be immediately isolated and transferred to a facility or hospital in which the detainee can be placed in an AII room and evaluated promptly for TB disease. Employees in All Correctional and Detention Facilities A medical history relating to TB should be obtained from and recorded for all new employees at the time of hiring, and a physical examination for TB disease should be required. The results of the screening and examination should be kept confidential; access should be granted to public health and infection control medical professionals only when necessary. In addition, a TST or QFT-G should be mandatory for all employees who do not have a documented history of a positive result. To improve the accuracy of the baseline result, a two-step TST or a single-step QFT-G should be used for the initial screening of employees who have not been tested during the preceding 12 months. Persons who have a positive TST or QFT-G result should have a chest radiograph taken and interpreted and should be required to have a thorough medical evaluation; if TB disease is excluded as a diagnosis, such persons should be considered for LTBI therapy. All employees should be informed that they should seek appropriate follow-up and testing for TB if they are immunosuppressed for any reason (e.g., have HIV infection). Any employee who has symptoms suggestive of TB should not return to the workplace until a clinician has excluded a diagnosis of infectious TB disease. Other Persons Who Might Need to be Screened Certain persons who are neither inmates nor employees but who visit high-risk facilities on a regular basis also should be considered for screening. These persons might include contractors (e.g., food handlers and service workers), volunteers, and those providing religious ministries. Screening of these persons should follow the same procedures as those outlined for employees. Periodic Screening Long-term inmates and all employees who have a negative TST or QFT-G result should have follow-up testing at least annually. Persons who have a history of a positive test result should be screened for symptoms of TB disease. Annual chest radiographs are unnecessary for the follow-up evaluation of infected persons. Test results should be recorded in medical records and in a retrievable aggregate database of all TST or QFT-G results. Personal identifying information should be kept confidential. Correctional facilities can use multiple strategies to ensure annual screening of long-term inmates for newly acquired TB infection. Certain institutions schedule annual screening on the inmate's date of birth or on the anniversary of the inmate's most recent test. Other institutions and systems suspend inmate movement and screen the entire population on the same day every year. Methods of screening a subset of the inmate population (e.g., on a monthly basis) are beneficial because they provide an ongoing assessment of M. tuberculosis transmission within the facility. Results from TST or QFT-G testing should be analyzed periodically to estimate the risk for acquiring new infection in a correctional facility; however, this analysis should be completed by using only the test results of facility employees and inmates who have remained in the facility continually during the interval between testing. The conversion rate equals the number of employees or inmates whose test results have converted from negative to positive (i.e., the numerator) during a specific interval divided by the total number of previously negative employees or inmates who were tested during the same interval (i.e., the denominator). In certain facilities, conducting an analysis of test results for specific areas or groups within the facility might be appropriate. More frequent screening is needed when a conversion rate is substantially higher than previous rates or when other evidence of ongoing transmission is detected. A cluster (i.e., either two or more patients with TB disease that are linked by epidemiologic or genotyping data or two or more TST or QFT-G conversions occurring in the correctional facility among inmates who are epidemiologically linked) or other evidence of person-toperson transmission also warrants additional epidemiologic investigation and possibly a revision of the facility's TB prevention and control protocol. Facilities in which the risk for infection with M. tuberculosis is minimal might not need to maintain a periodic screening program. However, requiring baseline TST or QFT-G testing of employees would enable medical staff to distinguish between a TST or QFT-G conversion and a positive TST or QFT-G result caused by a previous exposure to M. tuberculosis. A decision to discontinue periodic employee screening should be made in consultation with the local or state health department. HIV Counseling, Testing, and Referral HIV counseling, testing, and referral (CTR) should be routinely recommended for all persons in settings in which the population is at increased behavioral or clinical risk for acquiring or transmitting HIV infection, regardless of setting prevalence (62). Because correctional facilities are considered settings in which the population is at increased risk for acquiring or transmitting HIV, routine HIV CTR is recommended for inmates. Furthermore, HIV infection is the greatest risk factor for progression from LTBI to TB disease (63,64). Therefore, HIV CTR should be routinely offered to all inmates and correctional facility staff with LTBI or TB disease if their HIV infection status is unknown at the time of their LTBI or TB disease diagnosis (64,65). Correctional facilities should be particularly aware of the need for preventing transmission of M. tuberculosis in settings in which persons infected with HIV might be housed or might work (66). Use of Data to Refine Policies and Procedures Correctional and detention facilities are strongly encouraged to collect and analyze data on the effectiveness of their TB screening policies and procedures. Working in conjunction with their state or local TB-control program, correctional and detention facilities should refine their screening policies and procedures as indicated by such data. In the absence of local data that justify revision, correctional and detention facilities should adhere to the screening recommendations detailed above. Case Reporting All states require designated health-care professionals to report suspected and confirmed cases of TB to their local or state health department; this reporting is mandatory for all correctional facilities, whether private, federal, state, or local. Correctional facility medical staff should report any suspected or confirmed TB cases among inmates or employees to the appropriate health agency in accordance with state and local laws and regulations, even if the inmate or detainee has already been released or transferred from the facility. Reporting cases to health departments benefits the correctional facility by allowing it to obtain health department resources for case management and contact investigation in both the facility and the community. For each suspected case of TB, the diagnosis or the exclusion of a diagnosis of TB should be entered immediately into 1) the person's medical record, 2) the retrievable aggregate TB-control database at the facility, and 3) the database at a centralized office if the system has multiple facilities. In addition, drug-susceptibility results should be sent to the state or local health department for use in monitoring the rates of drug resistance in the health department's jurisdiction. Drugsusceptibility reports also should be sent to all health departments managing the infectious person's contacts because the choice of medication for LTBI treatment is based on these drug-susceptibility test results (64). Reports to local or state health departments should identify the agency that has custodial responsibility for the inmate (e.g., county corrections agency, state corrections agency, ICE, Federal Bureau of Prisons [FBOP], and U.S. Marshals Service [USMS]) and the corresponding identification number for that agency (e.g., U.S. alien number, FBOP number, or USMS number). Federal law enforcement agencies frequently contract for bed space with local or private detention facilities. Therefore, custodial authority and corresponding custody identification numbers should be verified with the facility's custody staff; detention facility medical staff might not have this information available. Isolation in an Airborne Infection Isolation Room Initiation TB airborne precautions should be initiated for any patient who has signs or symptoms of TB disease or who has documented TB disease and has not completed treatment or not been determined previously to be noninfectious. Discontinuation For patients placed in an AII room because of suspected infectious TB disease of the lungs, airways, or larynx, airborne precautions can be discontinued when infectious TB disease is considered unlikely and either 1) another diagnosis is made that explains the clinical syndrome or 2) the patient has three negative acid-fast bacilli (AFB) sputumsmear results (67,68). The three sputum specimens should be collected 8--24 hours apart (69), and at least one should be an early morning specimen (because respiratory secretions pool overnight). Typically, this will allow patients with negative sputum-smear results to be released from an AII room in 2 days. Incarcerated patients for whom the suspicion of TB disease remains after the collection of three negative AFB sputum-smear results should not be released from airborne precautions until they are on standard multidrug anti-TB treatment and are clinically improving. Because patients with TB disease who have negative AFB sputum-smear results can still be infectious (70), patients with suspected disease who meet the above criteria for release from airborne precautions should not be released to an area in which other patients with immunocompromising conditions are housed. A patient who has drug-susceptible TB of the lung, airways, or larynx, is on standard multidrug anti-TB treatment, and has had a significant clinical and bacteriologic response to therapy (i.e., reduction in cough, resolution of fever, and progressively decreasing quantity of AFB on smear result) is probably no longer infectious. However, because culture and drug-susceptibility results are not typically known when the decision to discontinue airborne precautions is made, all patients with confirmed TB disease should remain in an AII room while incarcerated until they have had three consecutive negative AFB sputum-smear results collected 8--24 hours apart, with at least one being an early morning specimen, have received standard multidrug anti-TB treatment, and have demonstrated clinical improvement. Because the consequences of transmission of MDR TB (i.e., TB that is resistant to isoniazid and rifampin) are severe, infection-control practitioners might choose to keep persons with suspected or confirmed MDR TB disease in an AII room until negative sputum-culture results have been documented in addition to negative AFB sputum-smear results. Environmental Controls Overview Guidelines for preventing transmission of M. tuberculosis in health-care settings and for environmental infection control in health-care facilities have been published previously (71,72). These guidelines and this report can be used to educate correctional facility staff regarding use of environmental controls in TB infection-control programs. Environmental controls should be implemented when the risk for TB transmission persists despite efforts to screen and treat infected inmates. Environmental controls are used to remove or inactivate M. tuberculosis in areas in which the organism could be transmitted. Primary environmental controls consist of controlling the source of infection by using local exhaust ventilation (e.g., hoods, tents, or booths) and diluting and removing contaminated air by using general ventilation. These controls help prevent the spread and reduce the concentration of airborne infectious droplet nuclei (see Glossary). Environmental controls work in conjunction with administrative controls such as isolation of inmates with suspected TB disease detected through screening (see Glossary). Secondary environmental controls consist of controlling the airflow to prevent contamination of air in areas adjacent to the source (AII rooms) and cleaning the air (using a HEPA filter or ultraviolet germicidal irradiation [UVGI]) to increase the number of equivalent ACH.¶ The efficiency of different primary or secondary environmental controls varies; details concerning the application of these controls to prevent transmission of M. tuberculosis in health-care settings have been published previously (71). To be effective, secondary environmental controls should be used and maintained properly, and their strengths and limitations should be recognized. The engineering design and operational efficacy parameters for UVGI as a secondary control measure (i.e., portable UVGI units, upper-room air UVGI, and in-duct UVGI) continue to evolve and require special attention in their design, selection, and maintenance. Exposure to M. tuberculosis within correctional facilities can be reduced through the effective use of environmental controls at the source of exposure (e.g., an infectious inmate) or in general areas. Source-control techniques can prevent or reduce the spread of infectious droplet nuclei into the air in situations in which the source has been identified and the generation of the contaminant is localized by collecting infectious particles as they are released. Use of these techniques is particularly prudent during procedures that are likely to generate infectious aerosols (e.g., bronchoscopy and sputum induction) and when inmates with infectious TB disease are coughing or sneezing. Unsuspected and undiagnosed cases of infectious TB disease contribute substantially to disease transmission within correctional facilities (73). When attempting to control this type of transmission, source control is not a feasible option. Instead, general ventilation and air cleaning should be relied on for environmental control. General ventilation can be used to dilute the air and remove air contaminants and to control airflow patterns in AII rooms or other correctional facility settings. Air-cleaning technologies include mechanical air filtration to reduce the concentration of M. tuberculosis droplet nuclei and UVGI to kill or inactivate microorganisms so they no longer pose a risk for infection. Ventilation systems for correctional facility settings should be designed, and modified when necessary, by ventilation engineers in collaboration with infection-control practitioners and occupational health staff. Recommendations for designing and operating ventilation systems in correctional facilities have been published (48,49,74--76). The multiple types of and conditions for use of ventilation systems in correctional-facility settings and the individual needs of these settings preclude provision of extensive guidance in this report. Incremental improvements in environmental controls (e.g., increasing the removal efficiency of an existing filtration system in any area) are likely to lessen the potential for TB transmission from persons with unsuspected or undiagnosed TB. This information should not be used in place of consultation with experts who can advise on ventilation system and air handling design, selection, installation, and maintenance. Because environmental controls will fail if they are not properly operated and maintained, routine training and education of infection-control and maintenance staff are key components to a successful TB infection-control program. Airborne Infection Isolation Rooms Inmates known or suspected of having TB disease should be placed in an AII room or AII cell that meets the design and operational criteria for airborne infection isolation described previously (71). Inmates deemed infectious should remain in isolation until treatment or further evaluation has ensured that they are noninfectious. Facilities without an on-site AII room should have a written plan for referring patients with suspected or confirmed TB to a facility that is equipped to isolate, evaluate, and treat TB patients. New or renovated facilities should ensure that a sufficient number of AII rooms are available consistent with the facility risk assessment. Under rare circumstances, if an AII room is not available and the immediate transfer of the inmate with suspected infectious TB is not possible, the inmate should be housed temporarily in a room that has been modified to prevent the escape of infectious aerosols outside the TB holding area. The heating, ventilating, and air-conditioning (HVAC) system in this temporary TB holding area might have to be manipulated or augmented with auxiliary exhaust fans to create an inward flow of air that reduces the potential escape of infectious aerosols. If possible, air from these areas should be exhausted directly to the outdoors. If this is not feasible, the highest filtration efficiency compatible with the installed HVAC system should be used. Because TB droplet nuclei are approximately 1--5 micrometers in size, filtration efficiency should be evaluated for particles in that size range. Filter selection based on the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) Standard 52.2 Minimum Efficiency Reporting Value (MERV)--rating efficiency tables can help in this evaluation (77). Secondary air cleaning techniques (portable air cleaners and UVGI) also can be used in these areas to increase effective air cleaning. Local Exhaust Ventilation Aerosol-producing procedures should be performed in an area with a type of local exhaust ventilation that captures and removes airborne contaminants at or near their source without exposing persons in the area to infectious agents. Local exhaust devices typically use hoods. Two types of hoods are used: enclosing devices, in which the hood either partially or fully encloses the infectious source, and exterior devices, in which the infectious source is near but outside the hood. Fully enclosed hoods, booths, or tents are always preferable to exterior devices because of their superior ability to prevent contaminants from escaping. Enclosing devices should have sufficient airflow to remove >99% of airborne particles during the interval between the departure of one patient and the arrival of the next. The time required to remove a given percentage of airborne particles from an enclosed space depends on 1) the ACH number, 2) the location of the ventilation inlet and outlet, and 3) the physical configuration of the room or booth. The time interval required to ensure the proper level of airborne contaminant removal from enclosing devices varies according to ACH (Table 1). For example, if an enclosing device operates at six ACH, and the air inlet and exhaust locations allow for good air mixing, approximately 46 minutes would be required to remove 99% of the contaminated air after the aerosol-producing procedure has ended. Similarly, an additional 23 minutes (total time: 69 minutes) would be required to increase the removal efficiency to 99.9%. Doubling the ventilation rate decreases the waiting time by half. General Ventilation General ventilation is used to 1) dilute and remove contaminated air, 2) control the direction of airflow in a correctional facility setting, and 3) control airflow patterns in rooms. Recommended ventilation rates for correctional facility settings are typically expressed in ACH. Ventilation recommendations for selected areas in new or renovated correctional facility settings should be followed (Table 2). The feasibility of achieving a specific ventilation rate depends on the construction and operational requirements of the ventilation system and might differ for retrofitted and newly constructed facilities. The expense and effort of achieving a high ventilation rate might be reasonable for new construction but not be as feasible when retrofitting an existing setting. Ventilation design guidance for correctional facilities and related areas has been published (78). This design guidance includes specific ventilation recommendations regarding total ventilation, filtration efficiency, and environmental design parameters. For minimum outdoor air supply recommendations, the guidance refers to ASHRAE Standard 62, Ventilation for Acceptable Indoor Air Quality. In 2004, ASHRAE revised and renumbered this standard to ANSI/ASHRAE Standard 62.1 (74). For areas within correctional facilities that are not intended to contain persons with infectious TB, the recommended minimum outdoor air supply rates should meet or exceed those recommended in ANSI/ASHRAE Standard 62.1-2004 (74). When risk analysis reveals an enhanced potential for undiagnosed cases of infectious TB, facility designers and owners may consider using higher supply rates of outdoor air (e.g., those recommended for areas within health-care facilities anticipated to contain infectious patients). Minimum outdoor air supply recommendations for health-care facilities have been published (71,79). Because correctional areas frequently will not have an exact equivalent area within the health-care environment, the designer or owner should identify an analogous health-care area from which to choose the outdoor air supply recommendation. This selection should be made on the basis of occupant risk factors for TB, occupant activities, and occupant density within the area. For example, the intake, holding, and processing area of a higher risk correctional facility might be considered analogous to the emergency waiting room area in a health-care facility. In that case, the recommended outdoor air supply would be at least two ACH. The direction of air movement relative to adjacent areas is necessary for the containment of contaminated air. Air within a correctional facility should flow to minimize exposure of others within the building (Table 2). For example, air inside an AII room or cell should flow from the corridor and air-supply grille across the worker, then across that patient, and finally out of the room. To ensure that air is flowing from the corridor into an AII room or cell, smoke testing should be performed daily, even if the AII room or cell is equipped with a pressure-sensing device. Air flow (supply air and exhaust air) should be measured at least annually and compared with the designed air flow rates to ensure that optimal directional air flow and air exchange rates are being maintained (Table 2). Air Cleaning Methods Detailed information has been published regarding the selection, design, maintenance, and safety considerations associated with air cleaning methods (i.e., filtration and UVGI) (71). Designers and end users should consult this information. Air removed from areas likely to contain infectious aerosols (e.g., AII cells, sputum collection and other procedure rooms, and intake areas) should be exhausted directly to the outdoors to ensure that it cannot immediately reenter the building or pose a hazard to persons outside, in accordance with applicable federal, state, and local regulations. If discharging air to the outside is not feasible, HEPA filters should be used to clean the air before returning to the general ventilation system. Such recirculation is acceptable only if the air is recirculated back into the same general area from which it originated. For general population areas in which infectious aerosols are not anticipated but might be present (from persons with undiagnosed TB disease), total exhaust ventilation should be considered where and when the outdoor environmental conditions (temperature and humidity) are compatible with a single-pass system without undue energy or equipment costs. When recirculating air from these areas, the minimum ASHRAE-recommended level of filtration is a MERV-8 filter (78). However, CDC encourages selection and use of filters with higher MERV ratings to provide an incremental improvement in the protection afforded by this mechanism. The filtration system should be designed to prevent filter by-pass and to allow filter leakage testing and safe filter changes. A combination of air cleaning methods (e.g., MERV-rated filters and supplemental UVGI) may be used to increase effective air cleaning. When used, UVGI should be applied in-duct (i.e., inside the ductwork of existing HVAC systems) or in the upper room of the area to be treated to ensure that organisms are inactivated. Upper-air systems should be designed, installed, and monitored to ensure both sufficient irradiation in the upper room to inactivate M. tuberculosis and safe levels of UVGI in the occupied space. Environmental Control Maintenance To be most effective, environmental controls should be installed, operated, and maintained correctly. Ongoing maintenance should be part of any written TB infectioncontrol plan. The plan should outline the responsibility and authority for maintenance and address staff training needs. Failure to maintain environmental control systems properly has adversely impacted TB control and prevention efforts at facilities throughout the United States. At one hospital, improperly functioning ventilation controls were believed to be a factor in the transmission of MDR TB disease to four persons (three patients and a correctional officer), three of whom died (80). In three other multihospital studies evaluating the performance of AII rooms, failure to routinely monitor air-pressure differentials (whether manually or through use of continuous monitoring devices) resulted in a substantial percentage of the rooms being under positive pressure (81--84). Correctional facilities should schedule routine preventive maintenance that covers all components of the ventilation systems (e.g., fans, filters, ducts, supply diffusers, and exhaust grilles) and any air-cleaning devices in use. Performance monitoring should be conducted to verify that environmental controls are operating as designed. Performance monitoring should include 1) directional airflow assessments using smoke tubes and use of pressure monitoring devices sensitive to pressures at 0.001 inch of water gauge and 2) measurement of supply and exhaust airflows to compare with recommended air change rates for the respective areas of the facility. Records should be kept to document all preventive maintenance and repairs. Standard procedures should be established to ensure that 1) maintenance staff notify infection-control personnel before performing maintenance on ventilation systems servicing inmate-care areas and 2) infection-control staff request assistance from maintenance personnel in checking the operational status of AII cells and local exhaust devices (e.g., booths, hoods, and tents) before use. A protocol that is well written and followed will help to prevent unnecessary exposures of correctional facility staff and inmates to infectious aerosols. Proper labeling of ventilation system components (e.g., ducts, fans, and filters) will help identify air-flow paths. Clearly labeling which fan services a given area will help prevent accidental shutdowns (85). In addition, provisions should be made for emergency power to avoid interruptions in the performance of essential environmental controls during a power failure. Respiratory Protection Considerations for Selection of Respirators Respiratory protection is used when administrative (i.e., identification and isolation of infectious TB patients) and environmental controls alone have not reduced the risk for infection with M. tuberculosis to an acceptable level. The use of respiratory protection is most appropriate in specific settings and situations within correctional facilities. For example, protection is warranted for inmates and facility staff when they enter AII rooms, transport infectious inmates, and participate in cough-inducing procedures. Respirators should be selected from those approved by CDC/National Institute for Occupational Safety and Health (NIOSH) under the provisions of Title 42, Part 84 of the Code of Federal Regulations (86). Decisions regarding which respirator is appropriate for a particular situation and setting should be made on the basis of a risk assessment of the likelihood for TB transmission.** For correctional facilities, a CDC/NIOSH-approved N95 air-purifying respirator will provide adequate respiratory protection in the majority of situations that require the use of respirators. If a higher level of respiratory protection is warranted, additional information on other classes of air-purifying respirators and powered air-purifying respirators (PAPRs) is available (71). The overall effectiveness of respiratory protection is affected by 1) the level of respiratory protection selected (i.e., the assigned protection factor), 2) the fitting characteristics of the respirator model, 3) the care taken in donning the respirator, and 4) the effectiveness of the respiratory protection program, including fit testing and worker training. Implementing a Respiratory Protection Program All facilities should develop, implement, and maintain a respiratory-protection program for health-care workers or other staff who use respiratory protection. Respiratoryprotection programs are required for facilities covered by the U.S. Occupational Safety and Health Administration (OSHA) (71,87--89). The key elements of a respiratory protection program include 1) assignment of responsibility, 2) training, and 3) fit testing (71,87,90,91). All correctional facility staff who use respirators for protection against infection with M. tuberculosis must participate in the facility's respiratory protection program (e.g., understand their responsibilities, receive training, receive medical clearance, and engage in fit testing) (71). In addition to staff members, visitors to inmates with TB disease should be offered respirators to wear while in AII rooms and instructed on proper use. Certain regular visitors (e.g., law enforcement officials, social workers, ministers and other religious representatives, and attorneys and other legal staff) might be there in an occupational capacity. Each facility, regardless of TB risk classification (i.e., minimal or nonminimal), should develop a policy on the use of respirators by visitors of patients. Precautions for Transporting Patients Between Correctional or Detention Facilities Recommended precautions to take when transporting patients between facilities have been published (71). Patients with suspected or confirmed infectious TB disease should be transported in an ambulance whenever possible. The ambulance ventilation system should be operated in the nonrecirculating mode and the maximum amount of outdoor air be provided to facilitate dilution. If the vehicle has a rear exhaust fan, it should be used during transport. If the vehicle is equipped with a supplemental recirculating ventilation unit that passes air through HEPA filters before returning it to the vehicle, this unit should be used to increase the number of ACH. Airflow should be from the cab (i.e., front of vehicle) over the patient and out the rear exhaust fan. If an ambulance is not used, the ventilation system for the vehicle should bring in as much outdoor air as possible, and the system should be set to nonrecirculating. If possible, the cab should be physically isolated from the rest of the vehicle, and the patient should be placed in the rear seat. Drivers or other persons who are transporting patients with suspected or confirmed infectious TB disease in an enclosed vehicle should wear at least an N95 disposable respirator. If the patient has signs or symptoms of infectious TB disease (i.e., positive AFB sputum-smear result), consideration might be given to having the patient wear a surgical or procedure mask, if possible, during transport, in waiting areas, or when others are present. Diagnosis and Treatment of Latent Tuberculosis Infection and Tuberculosis Disease The principles of diagnosis and treatment of LTBI and TB disease discussed in this section are guidelines and not meant to substitute for clinical experience and judgment. Medical providers not familiar with the management of LTBI and TB disease should consult a person with expertise. All facilities' local operations procedures should include plans for consultation with and referral to persons with expertise in TB and should include criteria delineating when consultation and referral are indicated. Although the index of suspicion for TB disease varies by individual risk factors and prevalence of TB in the population served by the correctional facility, correctional facilities typically are considered higher-risk settings (see Screening). A diagnosis of TB disease should be considered for any patient who has a persistent cough (i.e., one lasting >3 weeks) or other signs or symptoms compatible with TB disease (e.g., hemoptysis, night sweats, weight loss, anorexia, and fever). Diagnostic tests for TB include the TST, QFT-G, chest radiography, and laboratory examination of sputum samples or other body tissues and fluids. Persons exposed to inmates with TB disease might become latently infected with M. tuberculosis depending on host immunity and the degree and duration of exposure. Therefore, the treatment of persons with TB disease plays a key role in TB control by stopping transmission and preventing potentially infectious cases from occurring (92). LTBI is an asymptomatic condition that can be diagnosed by the TST or QFT-G. Interpreting TST Results A baseline screening TST result of >10 mm induration is considered positive for the majority of correctional facility staff and inmates, and these persons should be referred for medical and diagnostic evaluation. However, for correctional facility staff and inmates who have had a known exposure in a correctional facility (i.e., close contact with an inmate or staff member with infectious TB disease) after having a previous (baseline) TST value of 0 mm, TST results of >5 mm should be considered positive and interpreted as a new infection. Correctional facility staff and inmates with a screening baseline TST result of >1 mm, but <10 mm, who are subsequently exposed to TB disease, should be considered newly infected if they have TST values increase by >10 mm on retest (Table 3). For example, a baseline TST result with 8 mm induration and a repeat TST result 1 year later with 18 mm induration would indicate a new infection. However, a repeat TST result with 12 mm induration would not indicate a new infection. When decisions are made for the diagnosis and treatment of LTBI and choosing the cutoff value for a positive reaction, certain risk factors (e.g., immunocompromising conditions and known contact with a TB patient) should be assessed. Correctional facility staff and inmates who have TST indurations of 5--9 mm should be advised that their results might be an indication for treatment under certain conditions. Special Considerations in Interpreting the TST Interpretation of the TST might be complicated by previous vaccination with BCG, anergy, and the "boosting" effect. Detailed recommendations describing how the TST should be interpreted in relation to these possible confounders have been published (64,93). Correctional Staff and Inmates who Refuse Testing for M. tuberculosis Infection A correctional facility staff member or inmate who refuses testing for M. tuberculosis infection should first be educated regarding the importance of routine screening of correctional facility staff and inmates. If the person continues to refuse to have a TST, the option may be offered for the person to be tested using the QFT-G test (and vice versa). The decision to offer an alternative test depends on the reason for refusal and should be consistent with the patient's underlying wishes (e.g., offering QFT-G in place of TST is acceptable if the patient objects to having injection of a substance but agrees to having blood drawn). Interpreting the QuantiFERON®-TB Gold Test Data Interpretation of QFT-G data is initially performed electronically; an approved interpretation method is automatically performed by the software supplied by the manufacturer (Table 4) (58). A complete description of the test's interpretation is included in the product insert. Persons who have a positive QFT-G result should be referred for a medical and diagnostic evaluation. On serial testing, a person with QFT-G results changing from negative to positive should be referred for medical and diagnostic evaluation and considered to be a QFT-G converter. Risk factors (e.g., the facility's prevalence of TB disease and personal risk factors) should be assessed when making decisions about the diagnosis and treatment of LTBI. Interpreting Chest Radiographs Persons with Suspected Pulmonary TB Multiple types of abnormalities demonstrated on chest radiographs are strongly suggestive of pulmonary TB disease, including upper-lobe infiltration, cavitation, and pleural effusion. Infiltrates can be patchy or nodular and observed in the apical or subapical posterior upper lobes or superior segment of the lower lobes. If radiographic or clinical findings are consistent with TB disease, further studies (e.g., medical evaluation, mycobacteriologic examinations of sputa or tissue, and comparison of current and prior chest radiographs) should be performed (65). Persons with TB pleural effusions might have concurrent unsuspected pulmonary or laryngeal TB disease (94). These patients should be considered infectious until pulmonary and laryngeal TB disease is excluded. Patients with suspected extrapulmonary TB disease also should be suspected of having pulmonary TB until concomitant pulmonary disease is excluded. The radiographic presentation of pulmonary TB in HIV-infected persons might be atypical. Apical cavitary disease is less common among such patients than HIV-negative patients. More common findings among HIV-infected persons are infiltrates in any lung zone, mediastinal or hilar adenopathy, or, in rare cases, a normal chest radiograph (65,95-97). Persons with LTBI To exclude pulmonary TB disease, a chest radiograph is indicated for all persons in whom LTBI is diagnosed. If chest radiographs do not indicate pulmonary TB, and no symptoms consistent with TB disease are present, persons with positive test results for TB infection should be considered for treatment for LTBI. Persons with LTBI typically have normal chest radiographs, although they might have abnormalities suggestive of previous TB disease or other pulmonary conditions. In certain patients with TB symptoms, pulmonary infiltrates might be apparent on chest computed tomography scan or magnetic resonance imaging study but not on chest radiograph. Previous, healed TB disease typically produces radiographic findings that differ from those associated with current TB disease. These findings include nodules, fibrotic scars, calcified granulomas, and apical pleural thickening. Nevertheless, a chest radiograph by itself cannot be used to distinguish between current and healed TB. Nodules and fibrotic scars might contain slowly multiplying tubercle bacilli and pose substantial risk for progression to TB disease. Calcified nodular lesions (i.e., calcified granulomas) and apical pleural thickening indicate lower risk for progression to TB disease (65). Pregnant Women Because TB disease is dangerous to both the mother and the fetus, a pregnant woman who has a positive TST or QFT-G result or who is suspected of having TB disease should receive a chest radiograph (with shielding consistent with safety guidelines) as soon as feasible. If symptoms or other high-risk conditions (e.g., HIV infection) are identified, a chest radiograph might have to be performed during the first trimester of pregnancy (64,65,98). Evaluation of Sputum Samples Sputum examination is a key diagnostic procedure for pulmonary TB disease (93) and is indicated for the following inmates and correctional facility staff: persons suspected of having pulmonary TB disease because of a chest radiograph consistent with TB disease, particularly those with any respiratory symptoms suggestive of TB disease; persons with chest radiographic findings suggestive of previous, healed TB disease; HIV-infected persons with any pulmonary symptoms (regardless of chest radiograph findings); or persons suspected of having pulmonary TB disease for which bronchoscopy is planned (all sputum specimens should be collected and final results of staining for AFB should have been reviewed before proceeding with bronchoscopy [67]). Specimen Collection Persons requiring smear- and culture-sputum examination should submit at least three sputum specimens (collected 8--24 hours apart, with at least one specimen collected in the early morning) (71,99). Specimens should be collected in a sputum induction booth or in an AII room. In resource-limited settings without environmental containment, collection is safer when performed outdoors. Patients should be instructed how to produce an adequate sputum specimen, and a health-care professional should supervise and observe the collection of sputum, if possible (93). For patients who are unable to produce an adequate sputum specimen, expectoration might be induced by inhalation of an aerosol of warm, hypertonic saline (71). Laboratory Examination Detection of AFB in stained smears by microscopy can provide the first mycobacteriologic indication of TB disease. A positive result for AFB in a sputum smear is predictive of increased infectiousness; however, negative AFB sputum-smear results do not exclude a diagnosis of TB disease if clinical suspicion is high. In 2002, only 63% of U.S. patients with reported positive sputum cultures had positive AFB sputum smears (100). Although smears allow for the detection of mycobacteria, definitive identification, strain typing, and drug-susceptibility testing of M. tuberculosis can be performed only via culture (93). A culture of sputum or other clinical specimen that contains M. tuberculosis provides a definitive diagnosis of TB disease. In the majority of cases, identification of M. tuberculosis and drug-susceptibility results are available within 28 days using recommended rapid methods (e.g., liquid culture and DNA probes). A negative culture result is obtained in approximately 14% of patients with confirmed pulmonary TB disease (100) . Testing sputum with certain techniques (e.g., nucleic acid amplification [NAA]) facilitates the rapid detection and identification of M. tuberculosis, but should not replace culture and drug-susceptibility testing in patients with suspected TB disease (88,101,102). Recommendations for use and interpretation of NAA tests in the diagnosis of TB disease have been published previously (101,102). Laboratories should report positive smear results within 24 hours of collection and positive cultures within 24 hours of the notation of the positive culture. Drugsusceptibility tests should be performed on initial isolates from all patients to assist in the identification of an effective anti-TB regimen. Drug-susceptibility tests should be repeated if 1) sputum specimens continue to be culture-positive 3 months after initiation of treatment or if 2) persons whose cultures had converted to negative subsequently revert to positive (65,93). Treatment for LTBI Treatment for LTBI is essential to controlling and eliminating TB disease in the United States because it substantially reduces the risk that TB infection will progress to TB disease (23). Certain persons are at high risk for developing TB disease once infected, and every effort should be made to begin these persons on a standard LTBI treatment regimen and to ensure that they complete the entire course of treatment for LTBI . Before treatment for LTBI is started, TB disease should be ruled out by history, medical examination, chest radiography, and when indicated, mycobacteriologic studies. Candidates for Treatment of LTBI Correctional facility staff and inmates in the following high-risk groups should be given treatment for LTBI if their reaction to the TST is >5 mm, regardless of age (64,65): HIV-infected persons, recent contacts of a TB patient, persons with fibrotic changes on chest radiograph consistent with previous TB disease, and patients with organ transplants and other immunocompromising conditions who receive the equivalent of >15 mg/day of prednisone for >1 month. All other correctional facility staff and inmates should be considered for treatment of LTBI if their TST results are >10 mm induration. If QFT-G is used, any correctional facility staff member or inmate with a positive QFT-G result should be considered for LTBI treatment. Decisions regarding initiation of LTBI treatment should include consideration of the likelihood of the patient continuing and completing LTBI treatment under supervision if released from the facility before the treatment regimen is completed. Persons with previously positive TST results who have previously completed treatment for LTBI (i.e., >6 months of isoniazid, 4 months of rifampin, or another regimen) do not need to be treated again unless concern exists that reinfection has occurred. Other persons who might be poor candidates for treatment of LTBI include those with a previous history of liver injury or a history of excessive alcohol consumption; active hepatitis and end-stage liver disease are relative contraindications to the use of isoniazid or pyrazinamide for treatment of LTBI (64,103). If the decision is made to treat such patients, baseline and follow-up monitoring of serum aminotransaminases are recommended. Treatment Regimens for LTBI Standard regimens have been developed for the treatment of LTBI (Table 5). The preferred treatment for LTBI is 9 months of daily isoniazid or biweekly dosing administered by DOT. Although regimens are broadly applicable, modifications should be considered for certain populations (e.g., patients with HIV infection) and when drug resistance is suspected. Reports of severe liver injury and death associated with the combination of rifampin and pyrazinamide for treatment of LTBI prompted ATS and CDC to revise previous recommendations. These recommendations now state that this regimen typically should not be offered for the treatment of LTBI (64,103--107). If the potential benefits substantially outweigh the demonstrated risk for severe liver injury and death associated with this regimen and the patient has no contraindications this regimen may be considered; a physician with experience treating LTBI and TB disease should be consulted before use of this regimen (103). Clinicians should continue the appropriate use of rifampin and pyrazinamide in standard multidrug anti-TB regimens for the treatment of TB disease (65). For all LTBI treatment regimens, nonadherence to intermittent dosing results in a larger proportion of total doses missed than daily dosing; therefore, all patients on intermittent treatment should receive DOT. In addition, DOT should be used with daily dosing of LTBI treatment whenever feasible. Patients with the highest priority for DOT are those at the highest risk for progression from LTBI to TB disease, including persons with HIV infection and persons who are recent contacts of infectious patients with pulmonary TB. Contacts of Patients with Drug-Susceptible TB Disease Contacts of patients with drug-susceptible TB disease who once tested negative but subsequently have a positive TST result (i.e., >5 mm) should be evaluated for treatment of LTBI. The majority of persons who are infected will have a positive TST result within 6 weeks of exposure; therefore, contacts of patients with drug-susceptible TB disease who have initial negative TSTs should be retested 8--10 weeks after the end of exposure to a patient with suspected or confirmed TB disease (108). Persons with TB infection should be advised that they can be re-infected with M. tuberculosis if re-exposed (109-111). If they have not been treated previously, HIV-infected persons (regardless of TST result or previous LTBI treatment history), persons receiving immunosuppressive therapy (regardless of TST result or previous LTBI treatment history), and persons with a known previous (to current exposure) positive TST also should be considered for LTBI treatment. Treatment of LTBI should not be started until a diagnosis of TB disease has been excluded. If the presence of TB disease is uncertain because of an equivocal chest radiograph, a standard multidrug anti-TB therapy might be started and adjusted as necessary, depending on the results of sputum cultures, drug-susceptibility tests, and clinical response (65). If cultures are obtained without initiating therapy for TB disease, treatment for LTBI should not be initiated until all cultures are reported as negative, which might take 6--8 weeks. Contacts of Patients with Drug-Resistant TB Disease Treatment for LTBI caused by drug-resistant M. tuberculosis organisms is complex and should be conducted in consultation with the local health department's TB control program and persons with expertise in the medical management of drug-resistant TB. Often this will require waiting for results of susceptibility testing of the isolate from the presumed source patient. Treatment should be guided by in vitro susceptibility test results from the isolate to which the patient was exposed (65,112,113). Pretreatment Evaluation and Monitoring of Treatment Routine laboratory monitoring during treatment of LTBI is indicated only for patients with abnormal baseline tests and for persons at risk for hepatic disease. Baseline laboratory testing is indicated only for persons infected with HIV, pregnant women, women in the immediate postpartum period (typically within 3 months of delivery), persons with a history of liver disease, persons who use alcohol regularly, and persons who have or who are at risk for chronic liver disease (64). All patients should undergo clinical monitoring at least monthly. This monitoring should include 1) a brief clinical assessment regarding the signs of hepatitis (i.e., nausea, vomiting, abdominal pain, jaundice, and yellow or brown urine) and 2) education about the adverse effects of the drug(s) and the need for prompt cessation of treatment and clinical evaluation should adverse effects occur. All aspects of the clinical encounter should be conducted in private and in the patient's primary language. Severe adverse events associated with the administration of tuberculin antigen or treatment of LTBI or TB disease (e.g., those resulting in hospitalization or death) should be reported to MedWatch, FDA's Safety Information and Adverse Event Reporting Program at telephone 800-FDA-1088, by facsimile at 800-FDA-0178, or via the Internet by sending Report Form 3500 (available at http://www.fda.gov/medwatch/safety/3500.pdf). Instructions regarding the types of adverse events that should be reported are included on MedWatch report forms. In addition, severe adverse effects associated with LTBI treatment should be reported to CDC's Division of Tuberculosis Elimination at telephone 404-639-8118. Treatment for TB Disease A decision to initiate treatment (i.e., combination anti-TB chemotherapy) should be made on the basis of epidemiologic information; clinical, pathological, and radiographic findings; and the results of microscopic examination of AFB-stained sputum smears and cultures for mycobacteria. A positive AFB-smear result provides strong inferential evidence for the diagnosis of TB, and combination chemotherapy should be initiated promptly unless other strong evidence against the diagnosis of TB disease is present (e.g., a negative NAA test). If the diagnosis is confirmed by isolation of M. tuberculosis or a positive NAA test, treatment should be continued until a standard course of therapy is completed. Because as few as 50% of patients with positive sputum culture results for M. tuberculosis will have negative sputum AFB-smear results (93), when initial AFB-smear results are negative, empiric therapy for TB is indicated if the clinical suspicion for TB disease is high. Regardless of the decision to begin anti-TB treatment, diagnoses other than TB should be considered and appropriate evaluations undertaken in patients with negative AFB-smear results. A diagnosis of culture-negative pulmonary TB can be made if sputum cultures are negative, the TST result is positive (in this circumstance, a reaction of >5 mm induration is considered positive), a clinical or radiographic response is observed 2 months after the initiation of therapy, and no other diagnosis has been established. An adequate regimen for culture-negative pulmonary TB includes an additional 2 months of isoniazid and rifampin to complete 4 months of treatment (65). If no clinical or radiographic response is observed by 2 months, treatment can be stopped, and other diagnoses (including inactive TB) should be considered. If AFB-smear results are negative, and suspicion for TB disease is low, treatment can be deferred until the results of mycobacterial cultures are known and a comparison chest radiograph is available (typically at 2 months). Among persons who have not begun treatment and in whom suspicion of TB is low, treatment of LTBI should be considered if 1) cultures are negative, 2) the TST result is positive (>5 mm induration), and 3) the chest radiograph is unchanged after 2 months. A person with TB expertise should be consulted for unusual or complex situations. Individualized case management should be provided for all patients with TB disease (114--116). In addition, patient management should be coordinated with officials of the local or state health department; suspected or confirmed TB cases should be reported to the local or state health department in accordance with laws and regulations. Regimens for treating TB disease should contain multiple drugs to which the organisms are susceptible. For persons with TB disease, treatment with a single drug can lead to the development of mycobacterial resistance to that drug. Similarly, adding a single drug to a failing anti-TB regimen is not recommended because it can lead to resistance to the added drug (65). For the majority of patients, the preferred regimen for treating TB disease consists of an initial 2-month phase of isoniazid, rifampin, pyrazinamide, and ethambutol, followed by a continuation phase of isoniazid and rifampin lasting >4 months, for a minimum total treatment period of 6 months (Tables 6 and 7). The decision to stop therapy should be made on the basis of the number of doses taken within a maximum period (not simply a 6-month period) (65). Persons with cavitary pulmonary TB disease and positive cultures of sputum specimens at the completion of 2 months of therapy should receive a longer, 7month continuation phase of therapy (total duration: 9 months) because of the substantially higher rate of relapse among persons with this type of TB disease (65). If interruptions in TB therapy occur, the decision should be made whether to restart a complete course of treatment or continue the regimen as originally intended. In the majority of instances, the earlier the break in therapy and the longer its duration, the more serious the effect and the greater the need to restart the treatment from the beginning. Continuous treatment is more important in the initial phase of therapy, when the bacillary burden is highest and the chance of developing drug resistance is greatest. Although no evidence on which to base detailed recommendations exists, examples of practical algorithms for managing interruptions in therapy have been described previously (65). For HIV-infected persons who are receiving antiretroviral therapy, TB treatment regimens might need to be altered. Whenever possible, the care of persons with concomitant TB and HIV should be provided by or in consultation with persons with expertise in the management of both TB and HIV-related disease (65). To prevent the emergence of rifampin resistance, persons with TB, HIV, and CD4+ T-lymphocyte cell counts <100 cells/mm3 should not be treated with highly intermittent (i.e., once- or twiceweekly) regimens. These patients should instead receive daily therapy during the intensive phase (i.e., first 2 months) and receive daily dosing or 3 doses per week by DOT during the continuation phase (117). Antiretroviral therapy should not be withheld because the patient is being treated for TB if it is otherwise indicated. Nevertheless, beginning both antiretroviral therapy and combination chemotherapy for TB at nearly the same time is not advisable. Although data on which to base recommendations are limited, experience in the fields of HIV and TB suggests that treatment for TB should be initiated first. Delaying the initiation of antiretroviral therapy until 4--8 weeks after starting antiTB therapy is advantageous because it 1) better enables providers to ascribe a specific cause to a drug side effect, 2) decreases the severity of paradoxical reactions, and 3) decreases adherence challenges for the patient. Until controlled studies have been conducted that evaluate the optimal time for starting antiretroviral therapy in patients with HIV infection and TB, this decision should be individualized on the basis of 1) the patient's initial response to treatment for TB, 2) the occurrence of side effects, and 3) the availability of multidrug antiretroviral therapy. Because drug-drug interactions might be less frequent with use of rifabutin, substitution of rifabutin for rifampin might be indicated with certain antiretroviral medications. Detailed information on TB treatment in HIV-infected persons has been published (65,107). Updates are posted on the Internet as new findings become available (at http://www.dhfs.state.wi.us/aidshiv/resources/overviews/aids_hiv.htm, http://www.hiv-druginteractions.org, and http://www.cdc.gov/nchstp/tb/tb_hiv_drugs/toc.htm). Drug-susceptibility testing should be performed on all initial isolates from patients with TB disease. When results from drug-susceptibility tests become available, the treatment regimen should be adjusted accordingly (65,113,114,118,119) (Tables 6 and 7). Medical providers treating patients with drug-resistant TB disease should seek expert consultation and collaborate with the local health department for treatment decisions (65). The primary determinant of treatment outcome is patient adherence to the drug regimen. Thus, careful attention should be paid to measures designed to enable and foster adherence (65,119,120). DOT is the preferred treatment strategy for all persons with TB disease and high-risk (e.g., HIV infected) persons with LTBI. DOT should be used throughout the entire course of therapy whenever feasible. Practitioners providing treatment to inmates should coordinate DOT with the local health department on an inmate's release. The local health department also may be involved in monitoring therapy for correctional facility staff (65). Challenges to Treatment Completion Achieving completion of treatment for LTBI or TB disease often is difficult, particularly in correctional facilities. Movement of inmates both within and outside of correctional systems interferes with continuity of care and might lead to treatment default (121). Comprehensive case management that includes discharge planning and coordination with other correctional facilities and health departments is needed to ensure completion of therapy for patients with TB disease and LTBI (42). Multiple studies have demonstrated that inmates have relatively low LTBI treatment completion rates, particularly those in jails who are likely to be released before their therapy has been completed (14,28,40,122). For a substantial proportion of inmates, referrals for follow-up after release are not made; of inmates whose appointments are scheduled, 40%--60% will not attend their first clinic visit (36,40). Multiple interventions have been attempted to improve LTBI treatment completion in this population, including patient education while in jail, use of incentives, and use of DOT (61,122,123). None of these strategies has had substantial success, although patient education and use of DOT have increased completion rates modestly in certain situations (61,122). Active case management, as recommended for TB disease, should be considered as a next step in improving the completion rates for LTBI treatment (14,42). Discharge Planning Correctional facilities should plan for the discharge of inmates and other detainees who have confirmed or suspected TB disease and those with LTBI who are at high risk for TB disease. Such planning is crucial to effective local TB control efforts within the community to which released inmates return. Facilities should ensure that their discharge plan is comprehensive and effective; the process should include 1) collaborating with public health and other community health-care professionals, 2) ensuring continuity of case-management, and 3) evaluating discharge-planning procedures and modifying procedures as needed to improve outcomes. Collaboration Between Correction Facilities and Public Health Officials Postconfinement follow-up is a necessary component of TB-control efforts (35,124). Effective discharge planning requires collaboration between corrections and medical staff (both intra- and inter-facility), and with public health and community-based service organizations (37). Correctional facilities and public health departments should overcome multiple obstacles associated with postdetention follow-up (125), including short length of stay in a facility; unscheduled release or transfer; poorly defined or implemented channels of communication between correctional and public health authorities; limited resources (i.e., staff, equipment, and medications) available to provide recommended TB prevention, screening, treatment, and discharge-planning services; limited resources of the patient to make or keep appointments; high prevalence of mental illness and substance abuse among correctional patients; mistrust among inmates, which might result in the provision of aliases or incorrect contact or locating information; and reincarceration with disruption in treatment or termination of public benefits. Collaboration is essential to ensure that TB-control efforts are undertaken in the most cost-effective manner. Coordination between the correctional facility and the public health department maximizes the effectiveness of any efforts begun in a correctional facility (126), and linking released detainees to the public health-care system might improve post-release adherence (35) and reduce recidivism (127,128). The types of relationships forged will depend on the assessment of the TB risk in the facility and the community. Comprehensive Discharge Planning Comprehensive discharge planning is an important component of case management and is essential for ensuring the continuity of TB management and therapy among persons with TB disease and LTBI. Following release, former inmates face housing, employment, and other crises concerning basic needs that often take priority over their health. Multiple reports from the United States and other countries support the use of comprehensive discharge planning in TB control efforts (42,129,130). Comprehensive discharge planning should be implemented for inmates with confirmed TB disease, suspected TB disease, and LTBI who also are at high risk for TB disease. Discharge planning for persons with LTBI who are considered at high risk for developing TB disease is critical if treatment is begun in the correctional facility. Starting all inmates at high risk on LTBI therapy might not be feasible while they are in the correctional facility, and the policy determining which risk groups to start on treatment should be made in collaboration with public health personnel. Collaboration ensures appropriate communication and adequate resources for treatment after transfer to another facility or after release to the community. At minimum, all inmates who have begun therapy for LTBI in a correctional facility should be given community contact information for follow-up and continuity of care. Ideally, all inmates demonstrated to be infected with TB should be considered for therapy, and discharge planning to facilitate therapy should be comprehensive (124). Because of high recidivism rates, discharge-planning efforts should begin in the detention phase and continue in the post-detention phase to ensure continuity of care as inmates move among different facilities and between correctional facilities and the community. Components of Discharge Planning Initiate Discharge Planning Early To ensure uninterrupted treatment, discharge planning for inmates who receive a diagnosis of TB disease should begin as soon as possible after diagnosis (131). Corrections or health services administrators (or their designees) should assign staff to notify the public health department of inmates receiving treatment for TB disease or LTBI. Inmates with TB disease should be interviewed while still incarcerated (ideally by public health staff) to enable facility administrators to assess and plan for the appropriate support and referrals that will be needed after discharge (131). Such personnel also should communicate with other facilities in the event of transfers of inmates. Provide Case Management To ensure continuity of care, all correctional facilities should assign personnel (preferably health-care professionals) to serve as case managers. These managers should be responsible for conducting discharge planning in the facility, which entails coordinating follow-up and communicating treatment histories with public health department and other health-care counterparts within the community (42). In addition, case managers should employ strategies (e.g., mental-illness triage and referral, substance-abuse assessment and treatment, and prerelease appointments for medical care) to help former inmates meet basic survival needs on release. The role of case manager should be assigned to a facility staff member who is capable of establishing good rapport with inmates; an effective case manager might be capable of persuading TB patients who are being released into the community to supply accurate information needed to ensure follow-up care. The following factors should be considered when planning community discharge of an inmate receiving treatment for TB (132): Where will the ex-inmate reside after discharge (e.g., a permanent residence, a halfway house, or a shelter)? Will family or other support be available? Are cultural or language barriers present? What kind of assistance will be needed (e.g., housing, social services, substance abuse services, mental health services, medical services, and HIV/AIDS services)? Does the inmate understand the importance of follow-up and know how to access health-care services? Obtain Detailed Contact Information To facilitate the process of locating former inmates, detailed information should be collected from all inmates with TB disease or LTBI for whom release is anticipated, including 1) names, addresses, and telephone numbers of friends, relatives, and landlords; 2) anticipated place of residence; and 3) areas typically frequented (e.g., restaurants, gyms, parks, and community centers) (61,133). Inmates also should complete a release form authorizing health department personnel to contact worksites, family members, corrections staff (parole officers), and public and private treatment centers. Inmates might give aliases or incorrect contact information because of fear of incrimination or deportation. The use of an alias can be a barrier to continuity of care on reentry to a correctional facility. Assess and Plan for Substance Abuse and Mental Health Treatment and for Other Social Services Substance abuse and other comorbid mental health conditions should be considered when developing a comprehensive discharge plan. Addiction affects health care, medication adherence, housing opportunities, social relationships, and employment and might be the greatest barrier to continuity of care for TB (134). Mental illness can be a barrier when community service providers have not been trained to interact with mentally ill patients. Persons who are mentally ill might have difficulties keeping medical appointments. Collaboration between corrections and health department personnel can facilitate the placement of former inmates in substance abuse or mental-health treatment programs to improve the likelihood of social stabilization and continuity of care (134,135). Other social issues present barriers to released inmates. Loss of health insurance benefits while incarcerated is common, and former inmates might be required to wait 30--365 days after release to become re-eligible for benefits (136,137). Certain correctional facilities have agreements with local Social Security Administration field offices to facilitate swift reactivation of these benefits (138); creation of and training in the use of such agreements are encouraged. Ideally, on entry into the correctional system, public benefits would be suspended, rather than terminated, and reactivated on release to eliminate gaps in coverage. Application for public benefits and insurance should be incorporated into the discharge planning phase whenever possible. If the inmate is likely to have limited access to care because of inability to pay for services on release, documentation should be made and another treatment mechanism identified (139). Make Arrangements for Postrelease Follow-Up Before release, the inmate should be introduced (preferably face to face) to the employee from the community treatment agency who is responsible for community-based treatment and care (139). When release dates are known, setting post-release appointments has been demonstrated to improve compliance (128,134,140). Patients with TB disease should be given a supply of medication at discharge adequate to last until their next medical appointment. Discharge planners can work with advocacy groups or private or government-funded programs to facilitate a safe, supported transition into the community (61). Make Provisions for Unplanned Release and Unplanned Transfers Administrative procedures should be in place for unscheduled discharge of inmates who are being managed or treated for TB (36,141). Reporting requirements for inmates with TB disease who are released or transferred to another facility vary among states and jurisdictions. Despite mandatory notification policies, notification of public health officials varies from 87%--92% for inmates with TB disease (37,126) to only 17% for inmates with LTBI (36,37). Correctional facility staff responsible for health department notification should relay information about all scheduled and unscheduled releases as it becomes available. All TB information concerning persons who are being transferred to other correctional settings should be provided to the receiving facility. In addition, inmates should be given a written summary or discharge card outlining their treatment plan to ensure continuity of care in case of unplanned and unanticipated release (131,142). Inmates with TB disease who are eligible for release or transfer to another medical or correctional facility but continue to be infectious should remain in airborne precautions during and after transfer until noninfectious (132). Provide Education and Counseling Patient education and documentation of education in the correctional facility is critical; multiple misconceptions persist among inmates and facility staff regarding means of transmission, differences between infection and disease, and methods of prevention and treatment for TB (143). Persons receiving treatment should be counseled about the importance of adhering to the treatment plan (131) as a measure to improve postrelease follow-up (61). Education should be delivered in the inmate's first preferred language and should be culturally sensitive with respect to ethnicity, sex, and age (135,144--147). The inmate should be actively involved in all education sessions to encourage communication regarding previous transition experiences (e.g., the inmate's treatment motivations and any positive or negative experiences with specific providers) (141). Inmates with LTBI who have not been started on therapy should be counseled on their risk factors, encouraged to visit the public health department, and provided with information about access to care after release. DOT DOT for TB disease or LTBI in the correctional setting provides an opportunity for educating and counseling inmates and for establishing a routine of medication administration. The effect, if any, of DOT on postrelease behavior has not been evaluated formally, but this practice might enhance adherence (122). Community-Based Case Management after Release Case-management strategies begun in the correctional facility should be continued after release for former inmates with confirmed or suspected TB disease and those with LTBI who are at high risk for progression to TB disease. Incentives and enablers (see Glossary) have improved adherence in incarcerated (35,60,61) and nonincarcerated (148,149) populations, and incentives combined with education and counseling optimize both shortand long-term adherence (40,60,61,150). Case management that takes into account cultural differences and addresses not only TB-control matters but patient-defined needs (particularly among foreign-born persons) results in improved completion rates for LTBI therapy (145). Case management by health department personnel after release is critical for continuity of care in the event of reincarceration. The provision of follow-up information from local health departments and community-based organizations back to corrections staff is helpful in determining whether discharge planning is effective. Discharge Planning for Immigration and Customs Enforcement Detainees Background Persons with TB disease detained by ICE officers are a potential public health threat because they typically are highly mobile, likely to leave and reenter the United States before completion of TB therapy, and at high risk for interrupting treatment (151). Therefore, ensuring treatment of such detainees is important to the national strategy to eliminate TB in the United States (32,152). In March 2003, the detention and removal functions of the former Immigration and Naturalization Service (INS) were transferred from the U.S. Department of Justice (DOJ) to the U.S. Department of Homeland Security (DHS). ICE is a division of DHS and detains approximately 200,000 persons annually while enforcing immigration law. ICE detainees are screened for TB disease at service processing centers, staging facilities, contract detention facilities, and local jails. Frequent transfers of ICE detainees between detention facilities are common. ICE detention provides an opportunity to identify persons with confirmed and suspected TB disease and initiate treatment, if appropriate. ICE detainees with confirmed or suspected TB disease receive treatment while they are in custody. Presently, ICE does not deport detainees with known infectious TB, but such persons might be deported when noncontagious, even if treatment has not been completed or the final culture and susceptibility results are pending. Discharge Planning for ICE Detainees In May 2004, ICE approved a policy to implement a short-term medical hold of persons with suspected or confirmed TB disease until continuity of care is arranged, which affords the ICE health services program the time needed to facilitate continuity of TB therapy arrangements before the patient's release or removal. The ICE health services program seeks to enroll all persons with confirmed or suspected TB disease in programs that facilitate the continuity of TB therapy between countries. These programs (e.g., CureTB, TB Net, and the U.S.-Mexico Binational Tuberculosis Referral and Case Management Project) facilitate TB referrals and follow-up for patients who move between the United States and other countries. ICE field office directors may consider a stay of removal for persons with MDR TB or other complicated cases, so they can receive and complete treatment in the United States before removal. In detention settings in which ICE detainees are held, facility staff who are responsible for TB communication should notify the ICE health services program of persons with confirmed or suspected TB disease. Collaboration with detention facilities and local and state health departments will facilitate enrollment in the appropriate continuity of care program before transfer, release, or repatriation. Correctional facility staff should identify these patients as ICE detainees when reporting TB cases to local and state health departments. Evaluation of Discharge Planning Effectiveness Evaluation of a discharge planning program is critical and should begin with an assessment of existing programs and activities. Program evaluation should be incorporated into the overall correctional quality improvement/assurance program (153). Data from program evaluation studies should be documented and published to ensure that correctional facility and public health department staff are informed regarding effective measures and the effective translation of research findings into practice (123). Evaluation of discharge planning should include measurements of adherence to therapy, cost savings (from unduplicated testing for persons with LTBI and completion of care without re-starts and extensions), recidivism, and the effectiveness of the collaboration between medical and corrections staff (both within and among facilities) and between correctional facilities and the public health department and other community agencies. Contact Investigation Overview Multiple outbreaks of TB, including those involving MDR TB, have been reported in prisons and jails, particularly among HIV-infected inmates (17,22,45,154). The identification of a potentially infectious case of TB in a correctional facility should always provoke a rapid response because of the potential for widespread TB transmission. A prompt public health response in a confined setting can prevent a TB outbreak or contain one that has already begun (16,21,155). The overall goal of a TB contact investigation is to interrupt transmission of M. tuberculosis. Ongoing transmission is prevented by 1) identifying, isolating, and treating persons with TB disease (source and secondary-case patients) and 2) identifying infected contacts of the source patient and secondary patients and providing them with a complete course of treatment for LTBI. The contact investigation can serve to educate corrections staff and inmates about the risk, treatment, and prevention of TB in correctional facilities; inform staff and inmates regarding the importance of engaging in recommended TBcontrol practices and procedures within the correctional system; and emphasize the importance of completion of therapy for persons with TB disease and LTBI. Because decisions involved in planning and prioritizing contact investigations in correctional facilities are seldom simple, a multidisciplinary team is preferable. Health departments often can help correctional facilities in planning, implementing, and evaluating a TB contact investigation. Data collection and management is an essential component of a successful investigation (21,36). It requires a systematic approach to collecting, organizing, and analyzing TBassociated data. As part of the contact investigation, all staff and investigation personnel should adopt a uniform approach. Investigators should have a clear understanding of how a contact is defined and what constitutes an exposure (156--158). Two correctional information systems are critical to the efficient conduct of a contact investigation: 1) an inmate medical record system containing TST results and other relevant information and 2) an inmate tracking system. The lack of either system can lead to the unnecessary use of costly personnel time and medical evaluation resources (e.g., TSTs and chest radiographs). Without these information systems, facilities also might be forced to implement costly lockdowns and mass screenings. TB Transmission Factors TB transmission is determined by the characteristics of the source patient and exposed contacts; the circumstances surrounding the exposure itself also determine whether ongoing transmission will occur. The following variables should be accounted for when planning each contact investigation. Characteristics of the Source Patient Source patients who have either cavitation on chest radiograph or AFB smear-positive respiratory specimens are substantially more likely to transmit TB than persons who have neither characteristic (159--163) Delays in TB diagnosis in source patients have also been associated with an increased likelihood of transmission (164). Nonetheless, substantial variability exists among the infectiousness of a given TB source patient. Although AFB smear status, cavitary disease, and delayed diagnosis increase the likelihood of transmission, certain persons with these characteristics infect few persons, whereas others with none of these characteristics might infect multiple persons. The best measure of the infectiousness of source patients is the documented infection rate among their contacts. Characteristics of Persons Who Have Been Identified as Contacts Immunosuppression. HIV infection is the greatest single risk factor for progression to TB disease. Therefore, HIV-infected contacts should receive the highest priority for evaluation of TB infection, even if these persons had shorter duration of exposure than other contacts. Persons receiving prolonged therapy with corticosteroids, chemotherapy for cancer, or other immunosuppressive agents (e.g., TNF-a antagonists) also should be considered high priority for investigation. In addition, persons with end-stage renal disease and diabetes mellitus should be promptly evaluated, because these conditions are associated with compromised immune function. Age. Young children (i.e., those aged <4 years) are at high risk for rapid development of TB disease, particularly TB meningitis. If an inmate with TB identifies a young child as a community contact, a health department referral should be made immediately. Exposure Characteristics Air volume. The volume of air shared between an infectious TB patient and susceptible contacts is a major determinant of the likelihood of transmission. Infectious particles become more widely distributed as air space increases, rendering them less likely to be inhaled. Ventilation. Ventilation is another key factor in the risk for airborne transmission of disease. Airborne infectious particles disburse throughout an entire enclosed space; thus, if air is allowed to circulate from the room occupied by an infectious patient into other rooms or central corridors, their occupants also will be exposed. Areas that have 1) confined air systems with little or no ventilation or 2) recirculated air without HEPA filtration have been associated with increased TB transmission. Duration of exposure. Although transmission of TB has occurred after brief exposure, the likelihood of infection after exposure to an infectious patient is associated with the frequency and duration of exposure. However, defining what constitutes a substantial duration of exposure for any given contact is difficult. When conducting a contact investigation, priority should be given first to inmates and employees who were most exposed to the source patient (21,154,162). Decision to Initiate a Contact Investigation The decision to initiate a contact investigation for an inmate or detainee with possible TB is made on a case-by-case basis. Each potential source patient's clinical presentation and opportunities for exposure should be evaluated. Contact investigations should be conducted in the following circumstances: Suspected or confirmed pulmonary, laryngeal, or pleural TB with cavitary disease on chest radiograph or positive AFB smears (sputum or other respiratory specimens). If the sputum smear is positive and the NAA is negative, TB is unlikely, and a contact investigation typically can be deferred. A negative NAA on an AFB-smear-negative specimen, however, should not influence decisions about the contact investigation (102). Suspected or confirmed pulmonary (noncavitary) or pleural TB with negative AFB smears (sputum or other respiratory specimens) and a decision has been made to initiate TB treatment. A more limited initial investigation may be conducted for smear-negative cases. Contact investigations typically are not indicated for extrapulmonary TB cases (except for laryngeal and pleural TB), unless pulmonary involvement is also diagnosed. The decision as to whether the facility should conduct a contact investigation should be guided by the probability that an inmate or employee has pulmonary TB. Sputum results for AFB serve as a major determinant (165). However, in certain patients with pulmonary TB, collecting sputum samples is not feasible. In this circumstance, other types of respiratory specimens (e.g., those from bronchoscopy) may be collected for AFB smear and mycobacterial culture. Principles for Conducting the Contact Investigation No simple formula has been devised for deciding which contacts to screen in a correctional facility contact investigation. However, the investigation should be guided by the following basic principles: Identified contacts should be stratified by their duration and intensity of exposure to the source patient. HIV-infected contacts should be classified as the highest priority group for screening and initiation of LTBI therapy, regardless of duration and intensity of exposure. Identified groups of contacts with the greatest degree of exposure should be screened immediately, followed by repeat testing at 8--10 weeks if the initial TST or QFT-G is negative. The infection rate should be calculated to assess the level of TB transmission. Decisions to expand the contact investigation to groups with less exposure should be made on the basis of the calculated infection rate. If no evidence of transmission is observed, the investigation should not be expanded. If transmission is occurring, the investigation should be expanded incrementally to groups with less exposure. When the group screened shows minimal or no evidence of transmission, the contact investigation should not be expanded further. Corrections and medical staff should be included in the contact investigation depending on their exposure risks. Ideally, decisions about structuring the contact investigation should be made collaboratively with the contact investigation team that includes input from the state or local health department. For certain investigations, screening a convenience sample before expanding the investigation is prudent. For example, in jail investigations, multiple contacts might already have been released, rendering those who remain incarcerated the only available group for screening. If a substantial number of high priority contacts cannot be evaluated fully, a wider contact investigation should be considered. The investigation should focus on identifying the contacts at highest risk for transmission, screening them completely, and providing a full course of LTBI treatment for persons demonstrated to be infected. In general, because wide-scale investigations divert attention away from the high priority activities necessary to interrupt transmission in the facility, mass screening of all persons who had any contact with the source patient should be avoided (166). Rarely is a person so infectious that wide-scale expansion of the contact investigation is necessary or beneficial. Medical Evaluation of Contacts Appropriate medical evaluation depends on both the immunologic status (e.g., HIV infection) of the contact and previous TST or QFT-G results. Adequate knowledge of these data is possible only through use of a medical record system that is complete, up-todate, and reliable with regard to TST or QFT-G status, testing date, and documentation of the reading in millimeters (for TST). Without an adequate medical record system (and therefore definitive information regarding prior TST or QFT-G results), the true infection and transmission rates cannot be determined. The lack of such information is likely to lead to unnecessary expansion of the contact investigation. All Contacts All contacts should be interviewed for symptoms of TB disease using a standard symptom questionnaire. Symptomatic contacts should receive a chest radiograph and a complete medical evaluation by a physician, regardless of TST or QFT-G status; they also should be isolated appropriately (i.e., inmates should be placed in an AII room if infectious TB is suspected by chest radiograph or clinical findings; staff should not be permitted to work).†† HIV testing should be considered for all contacts whose HIV status is unknown. Inmates with Documented Previous Positive TST or QFT-G results Inmates who are asymptomatic, HIV-negative, and have previous positive TST or QFT-G results need no further follow-up, other than consideration for "routine" treatment of LTBI, if not completed in the past. However, if such an inmate has any signs or symptoms suggestive of TB, further evaluation should be conducted (e.g., a chest radiograph for persons with respiratory symptoms). HIV-Infected Inmates HIV-infected contacts should be interviewed for symptoms, have a TST or QFT-G and chest radiograph performed, and initiate a complete course of treatment for LTBI (once TB disease has been ruled out), regardless of the TST or QFT-G result. Treatment should be initiated even for persons with a history of previous treatment for LTBI or TB disease because of the possibility of re-infection. Those with a history of a negative TST or QFTG should have a TST or QFT-G placed at baseline and again in 8--10 weeks. The results of the TST or QFT-G will not affect treatment decisions, but they will provide important information for the contact investigation. Anergy testing is not recommended (52). Previous TST-Negative or QFT-G--Negative Inmates (HIV Negative) Mandatory tuberculin skin or QFT-G testing of all previously TST- or QFT-G--negative inmate contacts should be conducted at baseline (unless previously tested within 1--3 months of exposure). Testing should be repeated 8--10 weeks from the most recent contact with the source patient (58,167). TST and QFT-G Converters Persons whose TSTs or QFT-Gs convert or those with newly documented, positive TST or QFT-G results should be offered treatment for LTBI unless medically contraindicated. If inmate contacts refuse medically indicated treatment for LTBI, they should be monitored regularly for symptoms. Certain facilities have chosen to monitor HIVinfected contacts with follow-up chest radiographs. Contact Investigation Stepwise Procedures The following steps are involved in conducting a contact investigation and might overlap in time. As soon as a person is confirmed or suspected of having TB disease, the case should be reported to the appropriate local health authorities and contacts promptly evaluated. Notify correctional management officials. Identification of TB in an inmate or facility staff member can be alarming for other inmates, corrections staff, and the community. The administrator should be notified through appropriate chain of command that a case of TB has been identified in the institution so that appropriate briefing and educational efforts can be initiated. Conduct a source patient chart review. The following data (with specific dates) should be collected: 1) history of previous exposure to TB, 2) history of TB symptoms (e.g., cough, fever, and night sweats), 3) weight history (particularly unexplained weight loss), 4) chest radiograph reports, 5) previous TST or QFT-G results, 6) mycobacteriology results (e.g., AFB smears, cultures, and susceptibilities), 7) NAA test results, 8) HIV status, and 9) other medical risk factors. Interview the source patient. A chart review and case interview should be accomplished within 1 working day for persons with AFB smear-positive respiratory specimens or cavitation on chest radiograph and within 3 days for all other persons (165). Source patients should be asked concerning TB symptom history, with a particular focus on duration of cough. Source patients also should be asked about where they conduct their daily activities. Persons with confirmed or suspected TB who were detained during the course of the infectious period should be interviewed regarding potential community contacts, particularly HIVinfected persons and young children; information regarding the location of community contacts also should be obtained. Source patients should be questioned regarding contacts during a second interview conducted 7--14 days after the first. Define the infectious period. Defining the infectious period for a source patient helps investigators determine how far back to go when investigating potential contacts. The infectious period is typically defined as 12 weeks before TB diagnosis or onset of cough (whichever is longer). If a patient has no TB symptoms, is AFB smear negative, and has a noncavitary chest radiograph, the presumed infectious period can be reduced to 4 weeks before the date of first positive finding consistent with TB. If the contact investigation reveals that TB transmission occurred throughout the identified infectious period, the period for contact investigation might need to be expanded beyond 12 weeks. Convene the contact investigation team. After TB is diagnosed, a team of professionals (e.g., infection-control, medical, nursing, custody, and local public health personnel) should be convened and charged with planning the contact investigation. A team leader should be identified and the roles and responsibilities of each team member defined, and a schedule of regular meetings (documented formally with written minutes) should be established. In addition, a communications plan and a plan for handling contact investigation data should be developed. Update correctional management officials. Administrative personnel should be kept apprised of the strategy, process, and action steps involved in conducting the contact investigation. Obtain source case inmate traffic history. The dates and locations of the source patient's housing during the infectious period and information regarding employment and education should be obtained. Groups of contacts should be prioritized according to duration of exposure and immune status. Tour exposure sites. A tour should be conducted of each place the source patient lived, worked, or went to school during the infectious period. In addition, information should be obtained regarding any correctional facility that has housed the source patient during the infectious period, including 1) the number of inmates who are housed together at one time, 2) the housing arrangement (e.g., cells versus dorms), 3) the general size of the air space, 4) the basics of the ventilation system (e.g., whether air is recirculated), 5) the pattern of daily inmate movement (e.g., when eating, working, and recreating), and 6) the availability of data on other inmates housed at the same time as the source patient. The assistance of a facility engineer often is necessary to help characterize the ventilation system and airflow direction within a correctional facility. Prioritize contacts. Contacts should be grouped according to duration and intensity of exposure. Persons with the most exposure and HIV-infected or other immunosuppressed contacts (regardless of duration of exposure) are considered highest priority. Because progression from exposure to death can be rapid among HIV-infected persons in a facility in which HIV-infected persons are housed or congregated separately, the entire group should be given high priority (45). Develop contact lists. Rosters of inmate and employee contacts from each location should be obtained and their current location investigated. Lists of exposed contacts should be generated and grouped according to current location (e.g., still incarcerated, released, and transferred). Conduct a medical record review on each high-priority contact. TST or QFTG status, chest radiograph history, history of treatment for LTBI, HIV status, and other high-risk medical conditions should be recorded. Particular attention should be given to weight history and previous visits to facility health-care professionals for respiratory symptoms. Dates should be carefully recorded. Evaluate HIV-infected contacts for TB disease and LTBI promptly. LTBI therapy should be initiated promptly among these persons once TB disease has been excluded. Place and read initial TSTs or perform QFT-Gs on eligible contacts. Tuberculin skin or QFT-G testing of all previously TST- or QFT-G--negative inmate contacts should be conducted at baseline (unless previously tested within 1--3 months of exposure). Referrals should be made for persons who have been released or transferred before receiving their initial TST or QFT-G. Make referrals for contact evaluation. Referrals should be made to the local health department for inmate contacts of the source case who have been released or transferred to another facility. Additionally, family members or frequent visitors of the source patient should be investigated by the health department; follow-up TST or QFT-G results for a substantial percentage of contacts of released inmates have been obtained on re-arrest by matching the list of exposed contacts with the jail intake TST or QFT-G registry (21). Calculate the infection rate and determine the need to expand the investigation. To calculate the infection rate, the total number of inmates whose TST or QFT-G has converted from negative to positive should be divided by the total number with a TST placed and read or QFT-G performed. Persons with a history of a prior positive TST or QFT-G should be excluded. The infection rate should be calculated by exposure site. In addition, if using tuberculin skin testing, separately calculating the rate for U.S.- versus foreign-born inmates might provide useful data (33); foreign-born contacts often have a history of BCG vaccination, and a TST "conversion" among these contacts might represent a vaccination-associated "booster" TST response (168). The contact investigation team should analyze the infection rate(s) and decide whether to expand the investigation. Place and read follow-up TSTs or perform follow-up QFT-Gs. Follow-up TSTs or QFT-Gs for contacts who had a negative TST or QFT-G result on initial testing should be placed 8--10 weeks after exposure to the source patient has ended. Referrals should be made for persons who have been released or transferred and need a follow-up TST or QFT-G. Determine the infection/transmission rate. The infection rate from the second round of testing should be calculated. In addition, the need to expand the investigation should be determined. Write a summary report. The summary report should briefly describe the circumstances of the investigation, how it was conducted, the results of the investigation (e.g., the number of secondary cases identified and the infection and transmission rates), and any special interventions required (including follow-up plans). The report should be distributed to corrections administrators and the local health department. Tuberculosis Training and Education of Correctional Workers and Inmates TB training and education of correctional workers and other persons associated with any correctional facility (e.g., volunteers and inmates) can help lower the risk for TB transmission and disease. To ensure the effectiveness of such training and education, multiple factors should be considered. First, correctional facilities and local or state health departments should collaborate when providing TB training and education to correctional workers; specifically, facilities should routinely work with health department staff to provide them with corrections-specific training. Second, routine TB education should be provided for all persons who spend significant time in the facility, and additional training should be given to any employee who will interact with persons at risk for TB. The ideal amount of training time and information varies by the local risk for TB transmission and by the job descriptions and characteristics of those needing training. Finally, TB training and education efforts and other TB-related events should be documented to ensure that these programs can be evaluated and updated. Training and Education in Correctional Facilities Correctional workers, volunteers, inmates, and other persons spending significant time in correctional facilities should receive training and education regarding M. tuberculosis as part of in-facility, preservice training or orientation. Training should be provided at least annually thereafter. In-facility training and education efforts can build on existing sources of TB-related preservice education and training. Regional and national professional associations frequently provide ongoing education regarding TB and infection control, and national correctional health-care conferences and courses for medical professionals working in correctional facilities regularly include TB in their curricula. TB-associated training should be designed to meet the needs of correctional workers with diverse job descriptions. In multiple facilities and for multiple categories of correctional workers, appropriate TB training might be accomplished through incorporation of the topic into other annual employee trainings (e.g., bloodborne pathogen training); more extensive or topic-specific training should be developed for persons who are specifically involved in TB control. Facilities that use inmates to provide peer-to-peer TB-education programs should provide similarly tailored training to any participating inmates. Facilities located in areas with a high TB prevalence or whose inmates have lived in such areas might need to increase the time and resources dedicated to TB training. The correctional facility health services director or designee (i.e., the staff member responsible for a facility's TB control program) should collaborate with the local public health department to establish TB education and training activities. In addition, these staff members routinely should evaluate and update the facility's TB training and education program in collaboration with the public health sector. External changes in the prevalence of TB in the community, changes in state or local public health policies, or changes in national TB control guidelines might necessitate the conduct of regular educational updates for staff. Each facility should maintain training records to monitor correctional worker training and education. Records of TB-related adverse events (e.g., documented in-facility transmission) also should be monitored as a means of evaluating training and education outcomes. The circumstances of adverse events should be investigated, and the possibility of enhanced or altered training should be considered as an appropriate intervention. Initial Training and Education for all Correctional Workers Although the level and detail of any employee's initial TB training and education session will vary according to staff members' job responsibilities, the following components should be included for all correctional workers, regardless of job function: communication regarding the basic concepts of M. tuberculosis transmission, signs, symptoms, diagnosis (including the difference between LTBI and TB disease), and prevention; provision of basic information regarding the importance of following up on inmates or correctional workers demonstrating signs or symptoms of TB disease; need for initiation of airborne precautions of inmates with suspected or confirmed TB disease; review of the policies and indications for discontinuing AII precautions; discussion of basic principles of treatment for TB disease and LTBI; and discussion regarding TB disease in immunocompromised persons.§§ Required Training for Correctional Workers in Facilities with AII Rooms Correctional workers in facilities equipped with AII rooms also should be provided clear guidelines regarding the identification and containment of persons with TB disease. Education efforts for these staff members should include 1) discussion of the use of administrative and engineering controls and personal protective equipment and 2) a respiratory protection program (including annual training) as mandated by OSHA (Standard 29 CFR OSHA/DOL [87]). Enhanced Training and Education for Correctional Workers in High-Risk Facilities Correctional workers in facilities with a high risk for TB transmission should receive enhanced and more frequent training and education concerning the signs and symptoms of TB disease, transmission of TB disease, and TB infection-control policies (including instruction on and location of the facility's written infection-control policies and procedures, exposure control plan, and respiratory protection program). If a contact investigation is being conducted because of suspected or confirmed infectious TB, the health department or designated health provider should educate facility correctional workers in all aspects of the investigation. Education should include information concerning contact investigation guidelines (165), TB transmission, the method used to determine a contact's risk for infection and prioritization for evaluation and treatment, the noninfectiousness of inmates and correctional workers with LTBI, the noninfectiousness of persons with TB disease who have responded to therapy and have submitted three AFB negative sputum-smear results, and patient confidentiality issues. Facility staff members who are responsible for TB-control activities should stay informed regarding current TB trends and treatment options. Conference attendance, participation in professional programs, and other off-site training are effective supplemental training strategies for correctional worker trainers and facility medical and infection-control staff. Training and Education of Public Health Department Staff State and local health department staff providing consultation or direct services to a correctional facility (including those who act as liaisons) should receive training and education regarding the unique aspects of health care and TB control in the correctional facility setting. Correctional facility administrators, contracted correctional facility health-care professionals, and health department staff should collaborate to develop an appropriate training program. The use of self-study and other educational materials should be encouraged as a supplement to training. Certain TB training resources also can be accessed on the Internet (Appendix A). Education and training of health department staff should cover (but not be limited to) the following topics: TB-related roles of correctional facility and health department staff; methods of effectively collaborating with correctional facilities; differences between and among jails, prisons, and other forms of detention facilities; correctional culture and the importance of respecting the mission and purpose (i.e., custody) of correctional facilities and correctional workers; the health department's role in the discharge of inmates (see Discharge Planning); and the effect of the custody and movement of foreign detainees on local facilities. Training and Education of Inmates Inmates should receive education from facility health-care professionals or other appropriately trained workers managing the screening or treatment process. Education and training should be appropriate in terms of the education level and language of the trainees. The following components should be incorporated into inmate training and education programs: general TB information (provided either at the time of admission or when being screened for TB); the meaning of a positive TST or QFT-G result and treatment options for LTBI; comprehensive TB education, including the infectiousness of and treatment for inmates being confined with suspected or confirmed TB disease; and the importance of completing treatment for inmates with LTBI or TB disease. Program Evaluation Six steps should be followed to ensure successful monitoring and evaluation of a TBprevention and -control program: identifying collaborators, describing the TB-control program, focusing the evaluation to assess TB risk and performance, collecting and organizing data, analyzing data and forming conclusions, and using the information to improve the TB program (169). The purpose of program evaluation is to improve accountability, enable ongoing learning and problem-solving, and identify opportunities for improvement. The evaluation process should be designed to provide information relevant to the stakeholders. Measures should be simple and the communication of results meaningful. Identifying Collaborators TB control requires the collaboration of correctional systems, health departments, and other community agencies; effective program evaluation also involves teamwork. Early engagement of program staff and internal and external collaborators (including custody staff) helps ensure that the evaluation will yield the information that is most useful to stakeholders. Such engagement also promotes mutual cooperation for constructive change. Although multiple parties might be involved, each TB program should have a single person designated to be responsible for data quality and program evaluation. Designating staff for these activities helps ensure that continuity and accountability are maintained. Describing the Program Underlying a useful evaluation is an understanding of how the TB program currently operates within the context of the facility. Evaluators should be knowledgeable about program goals and objectives, strategies, expected program-associated results, and the way in which the program fits into the larger organization and community. This information can typically be obtained by reviewing a facility's existing TB-control plan. In addition, all stakeholders should agree on program goals before the evaluation is undertaken (169). Focusing the Evaluation to Assess TB Risk and Performance Risk Assessment Each facility should assess its level of TB risk at least annually (71). The TB risk assessment (see Screening) determines the types and levels of administrative and environmental controls needed. Assessment of a facility's risk level includes analysis of disease burden and facility transmission, which can be conducted by examining the following indicators: Burden of disease --- community rates of TB disease (including other communities from which substantial numbers of inmates come; these data are available from local health departments), --- the number of cases of TB disease in the facility during the preceding year, and --- the number and percentage of inmates and staff with LTBI; and Facility transmission --- the number and percentage of staff and inmates whose tests for TB infection converted and the reasons for the conversion, --- the number of TB exposure incidents (see Contact Investigation), and --- evidence of person-to-person transmission. Conversion rates (as determined by annual testing) for staff and inmates should be determined and tracked over time to monitor for unsuspected transmission in the facility. In larger facilities, conversion rates for staff assigned to areas that might place them at higher risk for TB (e.g., booking and holding areas, day rooms, libraries, enclosed recreation areas, medical and dental areas, and transport vehicles) should be calculated and tracked. Staff should analyze contributing factors to TB exposure and transmission and plan for corrective intervention, as appropriate. The following performance measures should be considered when determining risk within all correctional facilities, including those that function as a contract facility within a larger correctional system: the timeliness with which patients with suspected TB disease are detected, isolated, and evaluated (see Performance Measurement for Improving Quality); and other factors (e.g., the total number of patients with TB housed in the facility and the number of persons housed in the facility who are risk for TB) that will help determine the controls needed (71). Performance Measurement for Improving Quality The risk-assessment process enables the monitoring of risk for TB transmission (the key program indicator) and helps guide the focus and intensity of ongoing performance measurement and monitoring. Facilities at higher risk (e.g., those with cases of TB disease) benefit more from broader investigation of performance than facilities at lower risk. Risk-assessment findings should help guide the development of simple process performance measures for each pertinent area of TB prevention and control. These performance measures can then be used to monitor program implementation and intermediate outcomes. Treatment completion and continuity of care are key performance indicators. Each facility should have goals against which to measure performance in these areas (e.g., 100% of patients with TB disease will have documented treatment completion or, in the case of release or transfer, continuity of treatment on release). For LTBI, goals might be that 100% of patients released during treatment will have a documented referral for continuity of care in the community and that 90% of these patients will follow-up on their referral. The following are examples of possible performance measures that can be useful as part of a TB program evaluation, depending on the level of risk: Timeliness of screening and isolation --- time from inmate admission to testing for TB infection, --- time from TB testing to obtaining test results, --- time from positive TB infection test results to obtaining a chest radiograph, --- time from identification of a suspect TB patient (either through symptoms or abnormal chest radiograph) to placement in an AII room, --- time from sputum collection to receipt of results, and --- time from suspicious result (either via radiograph, smear-positive result, or smear-negative/culture-positive result) to initiation of contact investigation; Treatment --- the number and percentage of patients with LTBI who initiated treatment and the percentage of persons who completed the prescribed treatment for LTBI (excluding those released from or transferred out of the facility), --- the number and percentage of persons in whom TB disease was diagnosed who completed the prescribed treatment regimen (excluding those released from or transferred out of the facility), and --- the reasons for treatment interruption among persons who stop therapy; and ¶¶ Continuity of care --- the number and percentage of patients released before completing treatment for TB disease or LTBI who had documented community appointments (or referrals) for continuity of care, and --- the number and percentage of patients with confirmed and suspected TB disease who kept their first medical appointment in the community. Other pertinent performance measures for correctional facilities might include the adherence rates among inmates and staff who should undergo TB testing, the percentage of staff receiving TB education and training annually, and the percentage of inmates receiving TB education. Assessment of Collaboration On an annual basis, each program also should evaluate its success in working collaboratively with local and state public health departments in each area of TB control (e.g., screening, containment, and assessment). Correctional systems should meet with their respective public health departments each year to assess risk, update TB policies and procedures, and assess compliance regarding environmental control and respiratory protection recommendations (see Environmental Controls and Respiratory Protection). Correctional systems also should assess collaboration with other agencies to which the inmates are released. Collecting and Organizing Data Data Sources As part of quality assessment, all facilities that house persons with confirmed or suspected TB disease should conduct periodic reviews of medical records for these patients and for a sample of patients with LTBI. In collaboration with the public health department, the review should be conducted at least annually in facilities with any confirmed or suspected cases of TB (including low-risk facilities) and quarterly in higherrisk facilities with numerous cases. The record review should compare actual performance against time standards, protocols, and goals for TB activities and outcomes (see Performance Measures for Improving Quality). Multiple tools are available for data collection (Appendix B) (131). Medical records should contain information regarding TB history and risk factors, treatment, and all other interventions and dates to enable performance to be monitored. Other sources of data include log books, interviews with staff, and observations. Quality controls for TST placement and reading should be checked at least annually. The quality of the data used for calculating performance also should be verified. Information Infrastructure Effective program monitoring and evaluation is made possible through the reliable collection of valid data and through analysis of these data. Health-care professionals responsible for the prevention and control of TB within a correctional facility should have access to complete medical records and a database of essential TB-related activity and measurements. A retrievable aggregate record system is essential for tracking all inmates and for assessing the status of persons who have TB disease and LTBI, particularly in large jail and prison systems in which inmates are transferred frequently from one facility or unit to another. This record system should maintain at minimum current information about the location, screening results, treatment status, and degree of infectiousness of these persons. In addition to facilitating case management, such a record system provides facilities with the information necessary for conducting annual TB risk assessments, monitoring TB trends, measuring performance, and assessing the effectiveness of overall TB control efforts. Information contained in health records should always be kept confidential; all staff members involved in program evaluation should receive training to maintain the confidentiality of patient information. Although medical databases can be maintained manually, electronic databases provide additional benefits by enabling a facility to 1) better track inmates for testing and case management, 2) access information regarding tests for TB infection, 3) share medical information regarding transferred inmates with other facilities, 4) link with the local health department, and 5) measure the effectiveness of TB-control efforts. Analyzing Data and Drawing Conclusions In a multifacility correctional system, evaluation data should be compiled for each facility separately and in aggregate. Data should be analyzed against standards, which can be defined externally (e.g., by national organizations or CDC-defined standards) or internally as established by the program collaborators (170). Once analyzed, conclusions should be drawn from the data and recommendations for program improvement developed. The evaluation and recommendations should be shared with program staff, administrators, and partners, including the local public health department. Using Information to Improve the TB Program The final step in the evaluation process is to implement the recommendations to improve the TB program. Program staff should use data to identify and remove barriers to improving performance, and administrators should make necessary revisions to policies or procedures. Because the evaluation process is cyclical, assessing whether recommendations have been implemented and whether outcomes are improved is crucial. Existing data can be used to clearly demonstrate the effects of implemented interventions. Collaboration and Responsibilities The management of TB from the time an inmate is suspected of having the disease until treatment is complete presents multiple opportunities for collaboration between correctional facilities and the public health department. For example, public health agencies can partner with correctional facilities in TB screening and treatment activities. In a study of 20 urban jail systems and their respective public health departments, only 35% reported having collaborated effectively when conducting TB-prevention and control activities (38). Formal organizational mechanisms (e.g., designated liaisons, regular meetings, health department TB program staff providing on-site services, and written agreements) are associated with more effective collaboration between correctional facilities and health departments (37). Correctional facilities and health departments should each designate liaisons for TBassociated efforts. Liaisons should serve as a familiar and accessible communication link between collaborating entities. The duty of liaison at the correctional facility should be assigned to the person responsible for TB control or to another staff member familiar with TB control and patient management at the facility. Regular meetings between correctional facilities and health departments are important to establish communication and collaboration on TB-related issues (37,171). Jurisdictions with regularly scheduled meetings between jails and public health staff are 13 times more likely to report having highly effective collaboration than jurisdictions that have not established such meetings (37). For example, in Florida, the state TB-control program and corrections health officials hold quarterly coordination meetings on TB issues and regularly scheduled collaborative TB case-review conferences (171), activities that have encouraged communication between facilities and local health departments. The presence of health department staff in correctional facilities can help promote more effective collaboration (37,171). Functions provided by such personnel within the correctional facility setting include screening, surveillance, education and training, contact investigation, and follow-up after release (171). For example, New York City Department of Health and Mental Hygiene personnel assigned to the Rikers Island jail interview inmates, monitor their care, suggest interventions or changes, and work with the jail to determine discharge planning needs for continuity of care in the community. Data access links are available on site that enable health department personnel to promptly inform corrections staff regarding previous completed therapy, incomplete work-up or therapy, sputum-smear results, culture and drug-susceptibility data, and ongoing treatment for TB cases and suspects. These on-site access links diminish the time spent in AII rooms and decrease the time required for patient work-up by providing confirmatory historical documentation. Correctional facilities and health departments should work together to agree on and delineate their respective roles and responsibilities. Establishing clear roles and responsibilities helps avoid duplication, confusion, the potential for breaching patient confidentiality, excess expenditures, and missed opportunities. Roles and responsibilities should be clearly defined for all TB-control activities that might require collaboration between correctional facilities and health departments, including screening and treatment of inmates for LTBI and TB disease, reporting of TB disease, follow-up of inmates with symptoms or abnormal chest radiographs, medical consultation regarding persons with confirmed and suspected TB disease, contact investigations for reported TB cases, continuity of treatment and discharge planning for persons with TB disease and LTBI, training and education of correctional facility staff, evaluation of screening and case management, and facility risk assessment. Agreements about roles and responsibilities may be formal or informal, but they should be recorded in writing. Formal agreements include memoranda of understanding and written policies or plans. Informal agreements may be as simple as an e-mail summary of a verbal discussion or meeting. The format for recording and communicating agreements (e.g., checklists, flow charts, algorithms, and lists of steps) may vary depending on the need. Once agreements are made, they should be reassessed periodically (see Program Evaluation). Correctional facilities and health departments should work together to formulate agreements that specify the information to be shared in a particular time frame, who will have access to specific information or databases, and how patient confidentiality will be protected. Information systems provide the framework for recording and accessing pertinent information (see Program Evaluation). Health departments should provide correctional facilities with pertinent TB surveillance information (e.g., local rates of drug resistance, the number of TB cases occurring in correctional facilities relative to the community, and the number of TB cases identified in the community among recently incarcerated persons), which can bolster support for TB-screening activities within these facilities. Legislation or policy statements can effectively encourage or mandate collaboration on issues (e.g., disease reporting, contact investigation, and discharge planning) when institutional barriers (e.g., time and resources) inhibit collaboration. For example, California has improved discharge planning by prohibiting the release or transfer of inmates with confirmed or suspected TB unless a written treatment plan has been received and accepted by the local health officer (172). Arizona's state administrative code places responsibility for contact investigations of TB exposures in correctional facilities on the correctional facility but requires consultation with (and reporting to) the local health department. ICE also has developed a policy memorandum requesting that ICE field office directors grant a short-term hold on the deportation of patients with TB disease to allow time for the ICE health services program to facilitate continuity of care. Summary of Recommendations Screening Early identification and successful treatment of persons with TB disease remains the most effective means of preventing disease transmission. Inmates who are likely to have infectious TB should be identified and begin treatment before they are released into the general population. Screening programs in the correctional setting also allow for the detection of substantial numbers of persons with LTBI who are at high risk for TB disease and would likely benefit from a course of treatment. The type of screening recommended for a particular correctional facility is determined by an assessment of the risk for TB transmission within that facility. The risk assessment should be performed annually and should be conducted in collaboration with the local or state health department. A facility's TB risk level can be defined as minimal or nonminimal. A facility should be classified as having minimal TB risk on the basis of four criteria: No cases of infectious TB have occurred in the facility in the last year. The facility does not house substantial numbers of inmates with risk factors for TB (e.g., HIV infection and injection-drug use). The facility does not house substantial numbers of new immigrants (i.e., persons arriving in the United States within the previous 5 years) from areas of the world with high rates of TB. Employees of the facility are not otherwise at risk for TB. Any facility that does not meet all of these criteria should be categorized as being a nonminimal TB risk facility. Inmates in all minimal TB risk correctional and detention facilities require an evaluation at entry for symptoms of TB. Persons with symptoms of TB require an immediate evaluation to rule out the presence of infectious disease and must be kept in an AII room until they are evaluated. All newly arrived inmates should be evaluated for clinical conditions and other factors that increase the risk for TB disease. Persons who have any of these conditions require further screening with a TST, a QFT-G, or a chest radiograph within 7 days of arrival. Regardless of TST or QFT-G result, inmates known to have HIV infection or other severe immunosuppression, as well as inmates who are at risk for HIV infection but whose HIV status is unknown, should have a chest radiograph taken as part of the initial screening. Persons who have an abnormal chest radiograph should be evaluated further to rule out TB disease; if TB disease is excluded as a diagnosis, LTBI therapy should be considered if the TST or QFT-G is positive. In nonminimal TB risk prisons, symptom screening assessment should be performed immediately for all new inmates. Any inmate who has symptoms suggestive of TB should be placed in an AII room and evaluated promptly for TB disease. Inmates who have no symptoms require further screening with a TST, a QFT-G, or a chest radiograph within 7 days of arrival. Regardless of their TST or QFT-G status, inmates known to have HIV infection or other severe immunosuppression, and inmates who are at risk for HIV infection but whose HIV status is unknown, should have a chest radiograph taken as part of the initial screening. Persons who have an abnormal chest radiograph should be evaluated further to rule out TB disease; if TB disease is excluded as a diagnosis, LTBI therapy should be considered if the TST or QFT-G result is positive. Symptom screening should be performed immediately on entry for all new detainees in nonminimal TB risk jails. Any detainee who has symptoms suggestive of TB should be placed in an AII room and promptly evaluated for TB disease. Detainees who are without symptoms require further screening with a TST, a QFT-G, or a chest radiograph within 7 days of arrival. Regardless of TST or QFT-G result, detainees known to have HIV infection, and detainees who are at risk for HIV infection but whose HIV status is unknown, should have a chest radiograph taken as part of the initial screening. Persons who have a positive result should be further evaluated to rule out TB disease. Screening in jails with the TST or QFT-G for purposes of initiating LTBI therapy often is not practical because of the high rate of turnover and short lengths of stay. A medical history relating to TB should be obtained from and recorded for all new employees at the time of hiring, and a physical examination for TB disease should be required. In addition, TST or QFT-G screening should be mandatory for all employees who do not have a documented positive result. Persons who have a positive TST or QFTG result should have a chest radiograph taken and interpreted and should be required to have a thorough medical evaluation; if TB disease is excluded as a diagnosis, such persons should be considered for LTBI therapy. All employees should be informed and instructed to seek appropriate follow-up and screening for TB if they are immunosuppressed for any reason (e.g., HIV infection, organ transplant recipient receiving immunosuppressive therapy, and treatment with TNF-a antagonist). Any employee who has symptoms suggestive of TB should not return to the workplace until a clinician has excluded a diagnosis of contagious TB disease. In general, long-term inmates and all employees who have a negative baseline TST or QFT-G result should have follow-up testing at least annually. Persons who have a history of a positive test result should be screened annually for symptoms of TB disease. Annual chest radiographs are unnecessary for the follow-up evaluation of infected persons. Test results should be recorded in medical records and in a retrievable aggregate database of all TST or QFT-G results. Case Reporting Correctional facility medical staff must report any suspected or confirmed TB cases among inmates or employees to the appropriate health agency in accordance with state and local laws and regulations, even if the inmate or detainee has already been released or transferred from the facility. Reporting cases to health departments benefits the correctional facility by allowing it to obtain health department resources for case management and contact investigation in both the facility and the community. In addition, drug-susceptibility results should be used to inform optimal therapy and sent to the state or local health department for use in monitoring the rates of drug resistance. The drug-susceptibility reports also should be sent to all health departments managing contacts of the TB case because the choice of medication for LTBI treatment is based on drug-susceptibility test results of the source case. Reports to local or state health departments should identify the agency that has custodial responsibility for the inmate. Airborne Infection Isolation TB airborne precautions should be initiated for any patient who 1) has signs or symptoms of TB disease or 2) has documented TB disease and has not completed treatment or not previously been determined to be non-infectious. For patients placed in an AII room because of suspected infectious TB disease of the lungs, airways, or larynx, airborne precautions can be discontinued when infectious TB disease is considered unlikely and either 1) another diagnosis is made that explains the clinical syndrome or 2) the patient has three negative AFB sputum-smear results. Incarcerated patients in whom the suspicion of TB disease remains after the collection of three negative AFB sputum-smear results should not be released from an AII room until they are on standard multidrug antiTB treatment and are clinically improving. A patient who has drug-susceptible TB of the lung, airways, or larynx; who is on standard multidrug anti-TB treatment; and who has had a clinical and bacteriologic response to therapy is probably no longer infectious. However, because culture and drug-susceptibility results typically are not known when the decision to discontinue airborne precautions is made, all patients in whom the probability of TB disease is high should remain in an AII room while incarcerated until they have 1) had three consecutive negative AFB sputum smear results, 2) received standard multidrug anti-TB treatment, and 3) demonstrated clinical improvement. Environmental Controls Environmental controls should be implemented when the risk for TB transmission persists despite efforts to screen and treat infected inmates. Environmental controls are used to remove, inactivate, or kill M. tuberculosis in areas in which the organism could be transmitted. Primary environmental controls consist of controlling the source of infection by using local exhaust ventilation (e.g., hoods, tents, or booths) and diluting and removing contaminated air using general ventilation. Secondary environmental controls consist of controlling the airflow to prevent contamination of air in areas adjacent to the source (AII rooms) and cleaning the air using HEPA filtration and/or UVGI. The efficiency of different primary or secondary environmental controls varies. A detailed discussion concerning the application of environmental controls has been published previously(71). Personal Respiratory Protection Respiratory protection is used when administrative (i.e., identification and isolation of infectious TB patients) and environmental controls alone have not reduced the risk for infection with M. tuberculosis to an acceptable level. The use of respiratory protection might be most appropriate in specific settings and situations within correctional facilities; for example, protection is warranted for inmates and facility staff when they enter AII rooms, transport infectious inmates in an enclosed vehicle, and perform or participate in cough-inducing procedures. In correctional facilities, a CDC/NIOSH-approved N95 airpurifying respirator will provide adequate respiratory protection in the majority of situations that require the use of respirators. All correctional facility staff members who use respirators for protection against infection with M. tuberculosis must participate in the facility's respiratory protection program (e.g., understand their responsibilities, receive training, receive medical clearance, and engage in fit testing). All facilities should develop, implement, and maintain a respiratoryprotection program for health-care workers or other staff who use respiratory protection. (Respiratory-protection programs are required for facilities covered by OSHA.) In addition to staff members, visitors to inmates with TB disease should be given respirators to wear while in AII rooms and instructed how to ensure their own respiratory protection by checking their respirator for a proper seal. Each facility, regardless of TB risk classification (i.e., minimal or nonminimal), should develop a policy on the use of respirators by visitors of patients. Diagnosis and Treatment of LTBI and TB Disease A diagnosis of TB disease should be considered for any patient who has a persistent cough (>3 weeks) or other signs or symptoms compatible with TB disease (e.g., bloody sputum [hemoptysis], night sweats, weight loss, anorexia, and fever). Diagnostic tests for TB include the TST, QFT-G, chest radiography, and laboratory examination of sputum samples or other body tissues and fluids. Persons exposed to inmates with TB disease might become infected with LTBI, depending on host immunity and the degree and duration of exposure. Therefore, the treatment of persons with TB disease plays a key role in TB control by stopping transmission and preventing potentially infectious cases from developing. LTBI is an asymptomatic condition that can be diagnosed by the TST or QFT-G. Regardless of age, correctional facility staff and inmates in the following high-risk groups should be given treatment for LTBI if their reaction to the TST is >5 mm: HIV-infected persons, recent contacts of a TB patient, persons with fibrotic changes on chest radiograph consistent with previous TB disease, and patients with organ transplants and other immunocompromising conditions who receive the equivalent of >15 mg/day of prednisone for >1 month. All other correctional facility staff and inmates should be considered for treatment of LTBI if their TST result is >10 mm induration. The preferred treatment for LTBI is 9 months of daily isoniazid or biweekly dosing administered by DOT. Although LTBI treatment regimens are broadly applicable, modifications should be considered for certain populations (e.g., patients with HIV infection) and when drug resistance is suspected. Individualized case management should be provided for all patients with TB disease. In addition, patient management should be coordinated with officials of the local or state health department. Regimens for treating TB disease must contain multiple drugs to which the organisms are susceptible. For the majority of patients, the preferred regimen for treating TB disease consists of an initial 2-month phase of isoniazid, rifampin, pyrazinamide, and ethambutol, followed by a continuation phase of isoniazid and rifampin lasting >4 months, for a minimum total treatment period of 6 months. The decision to stop therapy should be based on the number of doses taken within a maximum period (not simply a 6-month period). Persons with cavitary pulmonary TB disease and positive cultures of sputum specimens at the completion of 2 months of therapy should receive a longer, 7-month continuation phase of therapy (total duration: 9 months) because of the substantially higher rate of relapse among persons with this type of TB disease. Drug-susceptibility testing should be performed on all initial M. tuberculosis isolates from patients with TB disease. When results from drug-susceptibility tests become available, the treatment regimen should be adjusted accordingly. Medical providers treating patients with drug-resistant TB disease should seek expert consultation and collaborate with the local health department for treatment decisions. TB treatment regimens might need to be altered for HIV-infected persons who are receiving antiretroviral therapy. Whenever possible, the care of persons with concomitant TB and HIV should be provided by or in consultation with experts in the management of both TB and HIV-related disease. The primary determinant of treatment outcome is patient adherence to the drug regimen. Thus, careful attention should be paid to measures designed to enable and foster adherence. DOT is the preferred treatment strategy for all persons with TB disease and high-risk (e.g., HIV infected) persons with LTBI. DOT should be used throughout the entire course of therapy whenever feasible. Practitioners providing treatment to inmates should coordinate DOT with the local health department on an inmate's release. The local health department also may be involved in monitoring therapy for correctional facility staff. Discharge Planning Postrelease follow-up is a necessary component of TB control efforts. Effective discharge planning requires collaboration between corrections and medical staff (both intra- and interfacility), as well as with public health and community-based service organizations. To ensure uninterrupted treatment, discharge planning for inmates in whom TB disease is diagnosed must begin as soon as possible after diagnosis. Corrections or health service administrators (or their designees) should assign staff to notify the public health department of inmates receiving treatment for TB disease or LTBI. Inmates with TB disease should be interviewed while still incarcerated (ideally by public health staff) to enable facility administrators to assess and plan for the appropriate support and referrals that will be needed after discharge. All correctional facilities should assign personnel (preferably health-care professionals) to serve as case managers. These managers should be responsible for conducting discharge planning in the facility, which entails coordinating follow-up and communicating treatment histories with public health department and other health-care counterparts within the community. Contact Investigation The overall goal of a TB contact investigation is to interrupt transmission of M. tuberculosis. Ongoing transmission is prevented by 1) identifying, isolating, and treating other persons with TB disease (e.g., secondary patients) and 2) identifying infected contacts of the source and secondary patients and providing them with a complete course of treatment for LTBI. Because decisions involved in planning and prioritizing contact investigations in correctional facilities are seldom simple, the process benefits from the input of a larger, multi-disciplinary team when possible. The best preparation for contact investigations in correctional facilities is ongoing, formal collaboration between correctional and public health officials. The decision to initiate a contact investigation for an inmate or detainee with possible TB is made on a case-by-case basis. In general, contact investigations should be conducted in the following circumstances: 1) suspected or confirmed pulmonary, laryngeal, or pleural TB and cavitary disease on chest radiograph or positive AFB smear results (sputum or other respiratory specimens) or 2) suspected or confirmed pulmonary (noncavitary) or pleural TB and negative AFB smear results (sputum or other respiratory specimens) and a decision has been made to initiate TB treatment. A more limited initial investigation may be conducted for smear-negative cases. Contact investigation should be conducted in a stepwise fashion that includes 1) notifying correctional management officials; 2) conducting a chart review of the source patient; 3) interviewing the source patient; 4) defining the infectious period; 5) convening the contact investigation team; 6) updating correctional management officials about the strategy, process, and action steps involved in conducting the contact investigation; 7) obtaining source case inmate traffic history (i.e., the dates and locations of the TB source patient's housing during the infectious period); 8) touring exposure sites; 9) prioritizing contacts according to duration and intensity of exposure and risk factors for becoming infected with TB and progressing to TB disease; 10) developing contact lists; 11) conducting a medical record review on each high-priority contact; 12) evaluating HIVinfected contacts promptly; 13) placing and reading initial TSTs or QFT-Gs on eligible contacts; 14) making referrals for contact evaluation (e.g., referrals to the local health department for contacts of inmates who have been released or transferred to another facility, family members, frequent visitors of the source patient); 15) calculating the infection rate and determining the need to expand the investigation; 16) placing and reading follow-up TSTs or QFT-Gs; 17) determining the infection/transmission rate from the second round of testing; and 18) writing a summary report. Training and Education Although the level and detail of any employee's initial TB training and education session will vary according to staff members' job responsibilities, the following components should be included for all correctional workers, regardless of job function: 1) communication regarding the basic concepts of M. tuberculosis transmission, signs, symptoms, diagnosis (including the difference between LTBI and TB disease), and prevention; 2) provision of basic information regarding the importance of following up on inmates or correctional workers demonstrating signs or symptoms of TB disease; 3) explanation of the need for initiation of AII of inmates with suspected or confirmed TB disease; 4) review of the policies and indications for discontinuing AII precautions; 5) discussion of basic principles of treatment for TB disease and LTBI; and 6) discussion regarding TB disease in immunocompromised persons. Correctional workers in facilities with a high risk of TB transmission should receive enhanced and more frequent training and education regarding 1) the signs and symptoms of TB disease, 2) transmission of TB disease, and 3) infection-control policies (including instruction on and location of written infection-control policies and procedures, the facility's exposure control plan, and the respiratory protection program). State and local health department staff providing consultation or direct services to a correctional facility (including those who act as liaisons) should receive training and education regarding the unique aspects of health care and TB control in the correctional facility setting. Correctional facility administrators, contracted correctional facility health-care professionals, and health department staff should collaborate to develop an appropriate training program. Inmates should receive education from facility health-care professionals or other appropriately trained workers managing the screening or treatment process. Education and training should be appropriate in terms of the education level and language of the trainees. Program Evaluation Program evaluation should be performed based on the CDC framework. Successful monitoring and evaluation of a TB-prevention and -control program includes identifying collaborators, describing the TB-control program, focusing the evaluation to assess TB risk and performance, collecting and organizing data, analyzing data and forming conclusions, and using the information to improve the TB program. Collaboration and Responsibilities The management of TB from the time an inmate is suspected of having the disease until treatment is complete presents multiple opportunities for collaboration between correctional facilities and the public health department. Formal organizational mechanisms (e.g., designated liaisons, regular meetings, health department TB-program staff providing on-site services, and written agreements) have been demonstrated to be associated with more effective collaboration between correctional facilities and health departments. Correctional facilities and health departments should each designate liaisons for TBassociated efforts. Liaisons should serve as a familiar and accessible communication link between collaborating entities. The duty of liaison at the correctional facility should be assigned to the person responsible for TB control or to another staff member familiar with TB control and patient management at the facility. Correctional facilities and health departments should work together to agree on and delineate their respective roles and responsibilities. Establishing clear roles and responsibilities helps avoid duplication, confusion, the potential for breaching patient confidentiality, excess expenditures, and missed opportunities. Agreements about roles and responsibilities may be formal or informal, but they should be recorded in writing to avoid misunderstandings and to give the agreement longevity beyond personal relationships. Acknowledgments The following persons contributed to this report: G. Scott Earnest, PhD, Michael G. Gressel, PhD, Kenneth R. Mead, MS, Division of Applied Research and Technology; Teresa A. Seitz, MPH, Douglas B. Trout, MD, Division of Surveillance, Hazard Evaluations, and Field Studies, National Institute for Occupational Safety and Health, CDC. References 1. Elzinga G, Raviglione MC, Maher D. Scale up: meeting targets in global tuberculosis control. Lancet 2004;363:814--9. 2. MacNeil J, Lobato MN, Moore M. An unanswered health disparity: tuberculosis among correctional inmates, 1993 through 2003. Am J Public Health 2005;95:1800--5. 3. CDC. Prevention and control of tuberculosis in correctional facilities: recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR 1996;45(No. RR-8):1--27. 4. Bureau of Justice Statistics. Adult correctional populations, 1980--2004. Washington, DC: US Department of Justice, Office of Justice Programs; 2005. Available at http://www.ojp.usdoj.gov/bjs/glance/corr2.htm. 5. US Department of Justice. Prison and jail inmates at midyear 2003. Bureau of Justice Statistics Bulletin; 2004. NCJ 203947. 6. CDC. Reported tuberculosis in the United States, 2003. Atlanta, GA: US Department of Health and Human Services, CDC; 2004. 7. CDC. Probable transmission of multidrug-resistant tuberculosis in a correctional facility---California. MMWR 1993;42:48--51. 8. Braun MM, Truman BI, Maguire B, et al. Increasing incidence of tuberculosis in a prison inmate population: association with HIV infection. JAMA 1989;261:393-7. 9. White MC, Tulsky JP, Portillo CJ, Menendez E, Cruz E, Goldenson J. Tuberculosis prevalence in an urban jail: 1994 and 1998. Int J Tuberc Lung Dis 2001;5:400--4. 10. Salive ME, Vlahov D, Brewer TF. Coinfection with tuberculosis and HIV-1 in male prison inmates. Public Health Rep 1990;105:307--10. 11. Spencer SS, Morton AR. Tuberculosis surveillance in a state prison system. Am J Public Health 1989;79:507--9. 12. CDC. Tuberculosis prevention in drug-treatment centers and correctional facilities---selected U.S. sites, 1990--1991. MMWR 1993;42: 210--3. 13. Alcabes P, Vossenas P, Cohen R, Braslow C, Michaels D, Zoloth S. Compliance with isoniazid prophylaxis in jail. Am Rev Respir Dis 1989;140:1194--7. 14. Lobato MN, Leary LS, Simone PM. Treatment for latent TB in correctional facilities: a challenge for TB elimination. Am J Prev Med 2003;24:249--53. 15. Bellin EY, Fletcher DD, Safyer SM. Association of tuberculosis infection with increased time in or admission to the New York City jail system. JAMA 1993;269:2228--31. 16. Stead WW. Undetected tuberculosis in prison: source of infection for community at large. JAMA 1978;240:2544--7. 17. Jones TF, Craig AS, Valway SE, Woodley CL, Schaffner W. Transmission of tuberculosis in a jail. Ann Intern Med 1999;131:557--63. 18. Koo DT, Baron RC, Rutherford GW. Transmission of Mycobacterium tuberculosis in a California state prison, 1991. Am J Public Health 1997;87:279-82. 19. MacIntyre CR, Kendig N, Kummer L, Birago S, Graham NM. Impact of tuberculosis control measures and crowding on the incidence of tuberculosis infection in Maryland prisons. Clin Infect Dis 1997;24:1060--7. 20. Jones TF, Woodley CL, Fountain FF, Schaffner W. Increased incidence of the outbreak strain of Mycobacterium tuberculosis in the surrounding community after an outbreak in a jail. South Med J 2003;96:155--7. 21. Bur S, Golub JE, Armstrong JA, et al. Evaluation of an extensive tuberculosis contact investigation in an urban community and jail. Int J Tuberc Lung Dis 2003;7:S417--23. 22. CDC. Tuberculosis transmission in multiple correctional facilities---Kansas, 2002--2003. MMWR 2004;53:734--8. 23. Institute of Medicine, Committee on the Elimination of Tuberculosis in the United States. Ending neglect: the elimination of tuberculosis in the United States. Washington, DC: National Academy Press; 2000. 24. Graham NM, Nelson KE, Solomon L, et al. Prevalence of tuberculin positivity and skin test anergy in HIV-1 seropositive and seronegative drug users. JAMA 1992;267:369--72. 25. Wallace R, Wallace D. Socioeconomic determinants of health: community marginalization and the diffusion of disease and disorder in the United States. BMJ 1997;314:1341--5. 26. Zolopa AR, Hahn JA, Gorter R, et al. HIV and tuberculosis infection in San Francisco's homeless adults. JAMA 1994;272:455--61. 27. Hammett TM, Gaiter JL, Crawford C. Reaching seriously at-risk populations: health interventions in criminal justice settings. Health Educ Behav 1998;25:99-120. 28. Bandyopadhyay T, Murray H, Metersky ML. Cost-effectiveness of tuberculosis prophylaxis after release from short-term correctional facilities. Chest 2002;121:1771--5. 29. Tulsky JP, Pilote L, Hahn JA, et al. Adherence to isoniazid prophylaxis in the homeless: a randomized controlled trial. Arch Intern Med 2000;160:697--702. 30. Iademarco MF, Castro KG. Epidemiology of tuberculosis. Semin Respir Infect 2003;18:225--40. 31. Moua M, Guerra FA, Moore JD, Valdiserri RO. Immigrant health: legal tools/legal barriers. J Law Med Ethics 2002;30:189--96. 32. CDC. Post-detention completion of tuberculosis treatment for persons deported or released from the custody of the Immigration and Naturalization Service---United States, 2003. MMWR 2003;52:438--41. 33. Saunders DL, Olive DM, Wallace SB, Lacy D, Leyba R, Kendig NE. Tuberculosis screening in the federal prison system: an opportunity to treat and prevent tuberculosis in foreign-born populations. Public Health Rep 2001;116:210--8. 34. Mohle-Boetani JC, Miguelino V, Dewsnup DH, et al. Tuberculosis outbreak in a housing unit for human immunodeficiency virus-infected patients in a correctional facility: transmission risk factors and effective outbreak control. Clin Infect Dis 2002;34:668--76. 35. Frieden TR, Fujiwara PI, Washko RM, Hamburg MA. Tuberculosis in New York City---turning the tide. N Engl J Med 1995;333:229--33. 36. Reichard AA, Lobato MN, Roberts CA, Bazerman LB, Hammett TM. Assessment of tuberculosis screening and management practices of large jail systems. Public Health Rep 2003;118:500--7. 37. Lobato MN, Roberts CA, Bazerman LB, Hammett TM. Public health and correctional collaboration in tuberculosis control. Am J Prev Med 2004;27:112-7. 38. Roberts CA, Lobato MN, Bazerman LB, Klieg R, Reichert AA, Hammett TM. Tuberculosis prevention and control in large jails: a challenge to tuberculosis elimination. Am J Prev Med 2006;30:125--30. 39. Layton MC, Henning KJ, Alexander TA, et al. Universal radiographic screening for tuberculosis among inmates upon admission to jail. Am J Public Health 1997;87:1335--7. 40. Tulsky JP, White MC, Dawson C, Hoynes TM, Goldenson J, Schecter G. Screening for tuberculosis in jail and clinic follow-up after release. Am J Public Health 1998;88:223--6. 41. Brock NN, Reeves M, LaMarre M, DeVoe B. Tuberculosis case detection in a state prison system. Public Health Rep 1998;113:359--64. 42. Klopf LC. Tuberculosis control in the New York State Department of Correctional Services: a case management approach. Am J Infect Control 1998;26:534--7. 43. Anderson KM, Keith EP, Norsted SW. Tuberculosis screening in Washington State male correctional facilities. Chest 1986;89:817--21. 44. Bergmire-Sweat D, Barnett BJ, Harris SL, Taylor JP, Mazurek GH, Reddy V. Tuberculosis outbreak in a Texas prison, 1994. Epidemiol Infect 1996;117:485-92. 45. Valway SE, Richards SB, Kovacovich J, Greifinger RB, Crawford JT, Dooley SW. Outbreak of multi-drug resistant tuberculosis in a New York State prison, 1991. Am J Epidemiol 1994;140:113--22. 46. CDC. Drug-susceptible tuberculosis outbreak in a state correctional facility housing HIV-infected inmates---South Carolina, 1999--2000. MMWR 2000;49:1041--4. 47. CDC. Tuberculosis morbidity among U.S.-born and foreign-born populations--United States, 2000. MMWR. 2002;51:101--4. 48. National Commission on Correctional Health Care. Standards for health services in jails. Chicago, IL: National Commission on Correctional Health Care; 2003. 49. National Commission on Correctional Health Care. Standards for health services in prisons. Chicago, IL: National Commission on Correctional Health Care; 2003. 50. Puisis M, Feinglass J, Lidow E, Mansour M. Radiographic screening for tuberculosis in a large urban county jail. Public Health Rep 1996;111:330--4. 51. Jones TF, Schaffner W. Miniature chest radiograph screening for tuberculosis in jails: a cost effectiveness analysis. Am J Respir Crit Care Med 2001;164:77--81. 52. CDC. Anergy skin testing and tuberculosis preventive therapy for HIV-infected persons: revised recommendations. MMWR 1996;46(No. RR-15):1--10. 53. Huebner RE, Schein MF, Bass JB Jr. The tuberculin skin test. Clin Infect Dis 1993;17:968--75. 54. Holden M, Dubin MR, Diamond PH. Frequency of negative intermediate-strength tuberculin sensitivity in patients with active tuberculosis. N Engl J Med 1971;285:1506--9. 55. Mckay A, Kraut A, Murdzak C, Yassi A. Determinants of tuberculin reactivity among health care workers: interpretation of positivity following BCG vaccination. Can J Infect Dis 1999;10:134--9. 56. CDC. The role of BCG vaccine in the prevention and control of tuberculosis in the United States. MMWR 1996;45(No. RR-4):1--18. 57. Mori T, Sakatani M, Yamagishi F, et al. Specific detection of tuberculosis infection: an interferon-gamma--based assay using new antigens. Am J Respir Crit Care Med 2004;170:59--64. 58. CDC. Guidelines for using the QuantiFERON®-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR 2005;54(No. RR15):49--55. 59. CDC. Tuberculosis elimination revisited: obstacles, opportunities, and a renewed commitment. MMWR 1999;48(No. RR-9):1--13. 60. White MC, Tulsky JP, Reilly P, McIntosh HW, Hoynes TM, Goldenson J. A clinical trial of a financial incentive to go to the tuberculosis clinic for isoniazid after release from jail. Int J Tuberc Lung Dis 1998;2:506--12. 61. White MC, Tulsky JP, Goldenson J, Portillo CJ, Kawamura M, Menendez E. Randomized controlled trial of interventions to improve follow-up for latent tuberculosis infection after release from jail. Arch Intern Med 2002;162:1044--50. 62. CDC. Revised guidelines for HIV counseling, testing, and referral. MMWR 2001;50(No. RR-19):1--57. 63. Selwyn PA, Hartel D, Lewis VA, et al. A prospective study of the risk of tuberculosis among intravenous drug users with human immunodeficiency virus infection. N Engl J Med 1989;320:545--50. 64. American Thoracic Society, CDC. Targeted tuberculin testing and treatment of latent tuberculosis infection. Am J Respir Crit Care Med 2000;161:S221--47. 65. American Thoracic Society, CDC, Infectious Diseases Society of America. Treatment of tuberculosis. MMWR 2003;52(No. RR-11):1--80. 66. Edlin BR, Tokars JI, Grieco MH, et al. An outbreak of multidrug-resistant tuberculosis among hospitalized patients with the acquired immunodeficiency syndrome. N Engl J Med 1992;326:1514--21. 67. Al Zahrani K, Al Jahdali H, Poirier L, Rene P, Menzies D. Yield of smear, culture and amplification tests from repeated sputum induction for the diagnosis of pulmonary tuberculosis. Int J Tuberc Lung Dis 2001;5:855--60. 68. Conde MB, Soares SL, Mello FC, et al. Comparison of sputum induction with fiberoptic bronchoscopy in the diagnosis of tuberculosis: experience at an acquired immune deficiency syndrome reference center in Rio de Janeiro, Brazil. Am J Respir Crit Care Med 2000;162:2238--40. 69. Frieden T, ed. Toman's tuberculosis: case detection, treatment, and monitoring--questions and answers. 2nd ed. Geneva, Switzerland: World Health Organization; 2004. 70. Behr MA, Warren SA, Salamon H, et al. Transmission of Mycobacterium tuberculosis from patients smear-negative for acid-fast bacilli. Lancet 1999;353:444--9. 71. CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR 2005;54(No. RR-17): 1--140. 72. CDC. Guidelines for environmental infection control in health-care facilities: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC). MMWR 2003;52 (No. RR-10):1--44. 73. Institute of Medicine. Tuberculosis in the workplace. Washington, DC: National Academy Press; 2001. 74. American National Standards Institute, American Society of Heating, Refrigerating, and Air-Conditioning Engineers. ANSI/ASHRAE Standard 62.12004. Ventilation for acceptable indoor air quality. Atlanta, GA: American Society of Heating, Refrigerating, and Air-Conditioning Engineers; 2004. 75. American Correctional Association. Standards for adult correctional institutions, 4th ed. Lanham, MD: American Correctional Association; 2003. 76. American Correctional Association. 2004 standards supplement. Lanham, MD: American Correctional Association; 2004. 77. American Society of Heating, Refrigerating and Air-Conditioning Engineers. ANSI/ASHRAE Standard 52.2-1999. Method of testing general ventilation aircleaning devices for removal efficiency by particle size. Atlanta, GA: American Society of Heating, Refrigerating and Air-Conditioning Engineers; 2000. 78. American Society of Heating, Refrigerating and Air-Conditioning Engineers. Justice facilities. 2003 ASHRAE Handbook: HVAC applications. Atlanta, GA: American Society of Heating, Refrigerating and Air-Conditioning Engineers; 2003:8.1--8.3. 79. American Society of Heating, Refrigerating and Air-Conditioning Engineers. Health care facilities. 2003 ASHRAE Handbook: HVAC applications. Atlanta, GA: American Society of Heating, Refrigerating and Air-Conditioning Engineers; 2003:7.1--7.14. 80. Ikeda RM, Birkhead GS, DiFerdinando GT Jr, et al. Nosocomial tuberculosis: an outbreak of a strain resistant to seven drugs. Infect Control Hosp Epidemiol 1995;16:152--9. 81. Pavelchak N, DePersis RP, London M, et al. Identification of factors that disrupt negative air pressurization of respiratory isolation rooms. Infect Control Hosp Epidemiol 2000;21:191--5. 82. Kenyon TA, Ridzon R, Luskin-Hawk R, et al. A nosocomial outbreak of multidrug-resistant tuberculosis. Ann Intern Med 1997; 127:32--6. 83. Fraser VJ, Johnson K, Primack J, Jones M, Medoff G, Dunagan WC. Evaluation of rooms with negative pressure ventilation used for respiratory isolation in seven midwestern hospitals. Infect Control Hosp Epidemiol 1993;14:623--8. 84. Sutton PM, Nicas M, Reinisch F, Harrison RJ. Evaluating the control of tuberculosis among healthcare workers: adherence to CDC guidelines of three urban hospitals in California. Infect Control Hosp Epidemiol 1998;19:487--93. 85. Streifel AJ. Design and maintenance of hospital ventilation systems and the prevention of airborne nosocomial infections. In: Mayall CG, ed. Hospital epidemiology and infection control. 2nd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 1999:1211--21. 86. US Department of Health and Human Services. Respiratory protective devices. (Title 42 CFR part 84). Federal Register 2004;42:84. 87. Occupational Safety and Health Administration, Department of Labor. Personal protective devices--respiratory protection. (29 CFR part 1910.134). Federal Register 2004;29:1910.134. 88. American National Standards Institute. American national standard practices for respiratory protection. ANSI Standard Number 288.2-1992. New York, NY: American National Standards Institute; 1992. 89. European Committee for Standardization. Respiratory protective devices: filtering half masks to protect against particles---requirements, testing, marking. Brussels, Belgium: European Committee for Standardization; 2001. 90. CDC. Protect yourself against tuberculosis---a respiratory protection guide for health care workers. Atlanta, GA: US Department of Health and Human Services, Public Health Service, CDC; 1995:1--25. 91. CDC. NIOSH guide to industrial respiratory protection. Atlanta, GA: US Department of Health and Human Services, Public Health Service, CDC; 1987:1-296. 92. Ferebee SH. Controlled chemoprophylaxis trials in tuberculosis: a general review. Bibl Tuberc 1970;26:28--106. 93. American Thoracic Society, CDC, Infectious Diseases Society of America. Diagnostic standards and classification of tuberculosis in adults and children. Am J Respir Crit Care Med 2000;161:1376--95. 94. Conde MB, Loivos AC, Rezende VM, et al. Yield of sputum induction in the diagnosis of pleural tuberculosis. Am J Respir Crit Care Med 2003;167:723--5. 95. Greenberg SD, Frager D, Suster B, Walker S, Stavropoulos C, Rothpearl A. Active pulmonary tuberculosis in patients with AIDS: spectrum of radiographic findings (including a normal appearance). Radiology 1994;193:115--9. 96. Havlir DV, Barnes PF. Tuberculosis in patients with human immunodeficiency virus infection. N Engl J Med 1999;340:367--73. 97. Pitchenik AE, Rubinson HA. The radiographic appearance of tuberculosis in patients with the acquired immune deficiency syndrome (AIDS) and pre-AIDS. Am Rev Respir Dis 1985;131:393--6. 98. Snider D. Pregnancy and tuberculosis. Chest 1984;86:S10--3. 99. Siddiqui AH, Perl TM, Conlon M, Donegan N, Roghmann MC. Preventing nosocomial transmission of pulmonary tuberculosis: when may isolation be discontinued for patients with suspected tuberculosis? Infect Control Hosp Epidemiol 2002;23:141--4. 100. CDC. Reported tuberculosis in the United States, 2002. Atlanta, GA: US Department of Health and Human Services, Public Health Service, CDC; 2003. 101. CDC. Nucleic acid amplification tests for tuberculosis. MMWR 1996;45:950--2. 102. CDC. Update: nucleic acid amplification tests for tuberculosis. MMWR 2000;49:593--4. 103. CDC, American Thoracic Society. Update: fatal and severe liver injuries associated with rifampin and pyrazinamide for latent tuberculosis infection, and revisions in American Thoracic Society/CDC recommendations---United States, 2001. MMWR 2001;50:733--5. 104. CDC, American Thoracic Society. Update: adverse event data and revised American Thoracic Society/CDC recommendations against the use of rifampin and pyrazinamide for treatment of latent tuberculosis infection---United States, 2003. MMWR 2003;52:735--9. 105. CDC. Fatal and severe hepatitis associated with rifampin and pyrazinamide for the treatment of latent tuberculosis infection---New York and Georgia, 2000. MMWR 2001;50:289--91. 106. CDC. Update: fatal and severe liver injuries associated with rifampin and pyrazinamide treatment for latent tuberculosis infection. MMWR 2002;51:998--9. 107. CDC. Prevention and treatment of tuberculosis among patients infected with human immunodeficiency virus: principles of therapy and revised recommendations. MMWR 1998;47(No. RR-20):1--58. 108. Menzies RI. Tuberculin skin testing. In: Reichman LB, Hershfield ES, eds. Tuberculosis: a comprehensive international approach. 2nd ed. New York, NY: Marcel Dekker; 2000:279--322. 109. Caminero J, Pena M, Campos-Herrero M, et al. Exogenous reinfection with tuberculosis on a European island with a moderate incidence of disease. Am J Respir Crit Care Med 2001;163:717--20. 110. Small PM, Shafer RW, Hopewell PC, et al. Exogenous reinfection with multidrug-resistant Mycobacterium tuberculosis in patients with advanced HIV infection. N Engl J Med 1993;328:1137--44. 111. van Rie A, Warren R, Richardson M, et al. Exogenous reinfection as a cause of recurrent tuberculosis after curative treatment. N Engl J Med 1999;341:1174--9. 112. Iseman MD, Madsen LA. Drug-resistant tuberculosis. Clin Chest Med 1989;10:341--53. 113. Iseman MD. Treatment of multidrug-resistant tuberculosis. N Engl J Med 1993;329:784--91. 114. Chaulk CP, Moore-Rice K, Rizzo R, Chaisson RE. Eleven years of community-based directly observed therapy for tuberculosis. JAMA 1995;274:945--51. 115. Chaulk CP, Kazandjian VA. Directly observed therapy for treatment completion of tuberculosis: census statement of the Public Health Tuberculosis Guidelines Panel. JAMA 1998;279:943--8. 116. Weis SE, Slocum PC, Blais FX, et al. The effect of directly observed therapy on the rates of drug resistance and relapse in tuberculosis. N Engl J Med 1994;330:1179--84. 117. CDC. Acquired rifamycin resistance in persons with advanced HIV disease being treated for active tuberculosis with intermittent rifamycin-based regimens. MMWR 2002;51:214--5. 118. Goble M, Iseman MD, Madsen LA, Waite D, Ackerson L, Horsburgh CR Jr. Treatment of 171 patients with pulmonary tuberculosis resistant to isoniazid and rifampin. N Engl J Med 1993;328:527--32. 119. Simone PM, Iseman MD. Drug-resistant tuberculosis: a deadly and growing danger. J Respir Dis 1992;13:960--71. 120. Initial therapy for tuberculosis in the era of multidrug resistance: recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR 1993;42(No. RR-7):1--8. 121. Cummings KC, Mohle-Boetani J, Royce SE, Chin DP. Movement of tuberculosis patients and the failure to complete anti-tuberculosis treatment. Am J Respir Crit Care Med 1998;157:1249--52. 122. Nolan CM, Roll L, Goldberg SV, Elarth AM. Directly observed isoniazid preventive therapy for released jail inmates. Am J Respir Crit Care Med 1997;155:583--6. 123. White MC, Tulsky JP, Menendez E, Arai S, Goldenson J, Kawamura LM. Improving tuberculosis therapy completion after jail: translation of research into practice. Health Educ Res 2005;20:163--74. 124. Brewer TF, Heymann SJ. To control and beyond: moving toward eliminating the global tuberculosis threat. J Epidemiol Community Health 2004;58:822--5. 125. National Commission on Correctional Health Care. Health status of soonto-be-released inmates. Chicago, IL: National Commission on Correctional Health Care; 2002. 126. Hammett TM, Harmon P, Maruschak LM. 1996--1997 update: HIV/AIDS, STDs, and TB in correctional facilities: issues and practices. Washington, DC: US Department of Justice, Office of Justice Programs, National Institute of Justice; 1999. NCJ 176344. 127. Vigilante KC, Flynn MM, Affleck PC, et al. Reduction in recidivism of incarcerated women through primary care, peer counseling, and discharge planning. J Women's Health 1999;8:409--15. 128. Freudenberg N, Wilets I, Greene MB, Richie BE. Linking women in jail to community services: factors associated with rearrest and retention of drug-using women following release from jail. J Amer Med Womens Assoc 1998;53:89--93. 129. Wilcock K, Hammett TM, Parent DG. Controlling tuberculosis in community corrections. Washington, DC: National Institute of Justice Research in Action; 1995:1--11. 130. Marco A, Cayla JA, Serra M, et al. Predictors of adherence to tuberculosis treatment in supervised therapy programme for detainees before and after release. Study Group of Adherence to Tuberculosis Treatment of Prisoners. Eur Respir J 1998;12:967--71. 131. CDC. The status of TB prevention and control measures in large city and county jails in the U.S. Atlanta, GA: US Department of Health and Human Services, CDC; 2003. Available at http://www.cdc.gov/nchstp/tb/pubs/tbrelat_articles/statustb_jails/toc.htm. 132. CDC. Self-study modules on tuberculosis: TB surveillance and case management in hospitals and institutions. Atlanta, GA: US Department of Health and Human Services, CDC; 1999. 133. Menendez E, White MC, Tulsky JP. Locating study subjects: predictors and successful search strategies with inmates released from a U.S. county jail. Control Clin Trials 2001;22:238--47. 134. Rich JD, Holmes L, Salas C, et al. Successful linkage of medical care and community services for HIV-positive offenders being released from prison. J Urban Health 2001;78:279--89. 135. Sumartojo E. When tuberculosis treatment fails: a social behavioral account of patient adherence. Am Rev Respir Dis 1993;147:1311--20. 136. Bartlett JG, Tripoli LC, Rappaport ES, Ruby W. HIV in corrections. Chesterfield, MO: Correctional Medicine Institute; 2000. Available at http://www.cm-institute.org/hivin.htm. 137. Bazelon Center for Mental Health Law. Finding the key to successful transition from jail to the community: an explanation of federal Medicaid and disability program rules. Washington, DC: Bazelon Center for Mental Health Law; 2001. Available at http://www.bazelon.org/issues/criminalization/findingthekey.html. 138. Bazelon Center for Mental Health Law. Building bridges: an act to reduce recidivism by improving access to benefits for individuals with psychiatric disabilities upon release from incarceration: model law and commentary. Washington, DC: Bazelon Center for Mental Health Law; 2002. 139. Osher F, Steadman HJ, Barr H. A best practice approach to community reentry from jails for inmates with co-occurring disorders: the APIC model. Delmar, NY: The National GAINS Center for People with Co-occurring Disorders in the Justice System; 2002. 140. Richie BE, Freudenberg N, Page J. Reintegrating women leaving jail into urban communities: a description of a model program. J Urban Health 2001;78:290--303. 141. Conklin T, Lincoln T, Wilson R. A public health manual for correctional health care. Ludlow, MA: Hampden County Sheriffs Department; 2002. 142. Safyer S, Richmond L, Bellin E, Fletcher D. Tuberculosis in correctional facilities: the tuberculosis control program at the Montefiore Medical Center Rikers Island Health Services. J Law Med Ethics 1993;21:342--51. 143. Woods GL, Harris SL, Solomon D. Tuberculosis knowledge and beliefs among prison inmates and lay employees. J Correctional Health Care 1997;4:61-9. 144. White MC, Duong TM, Cruz ES, et al. Strategies for effective education in a jail setting: the Tuberculosis Prevention Project. Health Promot Pract 2003;4:422--9. 145. Goldberg SV, Wallace J, Jackson JC, Chaulk CP, Nolan CM. Cultural case management of latent tuberculosis infection. Int J Tuberc Lung Dis 2004;8:76--82. 146. Grinstead O, Zack B, Faigles B. Collaborative research to prevent HIV among male prison inmates and their female partners. Health Educ and Behav 1999;26:225--38. 147. National Commission on Correctional Health Care. Position statement on management of tuberculosis in correctional facilities. Chicago, IL: National Commission on Correctional Health Care; 1996. 148. Malotte CK, Rhodes F, Mais KE. Tuberculosis screening and compliance with return for skin test reading among active drug users. Am J Public Health 1998;88:792--6. 149. Perlman DC, Friedmann P, Horn L, et al. Impact of monetary incentives on adherence to referral for screening chest x-rays after syringe exchange-based tuberculin skin testing. J Urban Health 2003;80:428--37. 150. Johnston M, Cronin V, Wells M, Johri S. Individual educational sessions and inmate follow-up for latent tuberculosis infection treatment after jail release--a pilot study. Journal of Correctional Health Care 2003;10:47--58. 151. CDC. Preventing and controlling tuberculosis along the U.S.-Mexico border MMWR 2001;50(No. RR-1):1--27. 152. Federal Tuberculosis Task Force. Federal Tuberculosis Task Force Plan in response to the Institute of Medicine Report, Ending neglect: the elimination of tuberculosis in the United States. Atlanta, GA: US Department of Health and Human Services, CDC; 2003. 153. McNabb SJN, Surdo AM, Redmond A, et al. Applying a new conceptual framework to evaluate tuberculosis surveillance and action performance and measure the costs, Hillsborough County, Florida, 2002. Ann Epidemiol 2004;14:640--5. 154. McLaughlin SI, Spradling P, Drocuik D, Ridzon R, Pozsik CJ, Onorato I. Extensive transmission of Mycobacterium tuberculosis among congregated, HIVinfected prison inmates in South Carolina, United States. Int J Tuberc Lung Dis 2003;7:665--72. 155. Kimerling ME, Shakes CF, Carlisle R, Lok KH, Benjamin WH, Dunlap NE. Spot sputum screening: evaluation of an intervention in two homeless shelters. Int J Tuber Lung Dis 1999;3:613--9. 156. Marks SM, Taylor Z, Qualls NL, Shrestha-Kuwahara RJ, Wilce MA, Nguyen CH. Outcomes of contact investigations of infectious tuberculosis patients. Am J Respir Crit Care Med 2000;162:2033--8. 157. Reichler MR, Reves R, Bur S, et al. Evaluation of investigations conducted to detect and prevent transmission of tuberculosis. JAMA 2002;287:991--5. 158. Gerald LB, Bruce F, Brooks CM, et al. Standardizing contact investigation protocols. Int J Tuberc Lung Dis 2003;7:S369--74. 159. Shaw JB, Wynn-Williams N. Infectivity of pulmonary tuberculosis in relation to sputum status. Am Rev Tuberc 1954;69:724--32. 160. Grzybowski S, Barnett GD, Styblo K. Contacts of cases of active pulmonary tuberculosis. Bull Int Union Tuberc 1975;50:90--106. 161. Rose CE, Zerbe GO, Lantz SO, Bailey WC. Establishing priority during investigation of tuberculosis contacts. Am Rev Respir Dis 1979;119:603--9. 162. Bailey WC, Gerald LB, Kimerling ME, et al. Predictive model to identify positive tuberculosis skin test results during contact investigations. JAMA 2002;287:996--1002. 163. Gerald LB, Tang S, Bruce F, et al. A decision tree for tuberculosis contact investigation. Am J Respir Crit Care Med 2002;166:1122--7. 164. Golub JE, Bur S, Cronin WA, et al. Delayed tuberculosis diagnosis and tuberculosis transmission [Abstract]. Proc Am Thorac Soc 2005;2:A271. 165. CDC. Guidelines for the investigation of contacts of persons with infectious tuberculosis: recommendations from the National Tuberculosis Controllers Association and CDC. MMWR 2005;54(No. RR-15):1--47. 166. Rodriguez EM, Steinbart S, Shaulis G, Bur S, Dwyer DM. Pulmonary tuberculosis in a high school student and a broad contact investigation: lessons relearned. Md Med J 1996;45:1019--22. 167. Menzies D. Interpretation of repeated tuberculin tests: boosting, conversion, and reversion. Am J Respir Crit Care Med 1999;159:15--21. 168. Moreno S, Blazquez R, Novoa A, et al. The effect of BCG vaccination on tuberculin reactivity and the booster effect among hospital employees. Arch Intern Med 2001;161:1760--5. 169. CDC. Framework for program evaluation in public health. MMWR 1999;48(No. RR-11):1--40. 170. CDC. Controlling tuberculosis in the United States. MMWR 2005;54 (No. RR-12):1--81. 171. Hammett TM. Public health/corrections collaborations: prevention and treatment of HIV/AIDS, STDs, and TB. Washington, DC: US Department of Justice, National Institute of Justice; 1998. 172. California Health And Safety Code, Section 121361. Available at http://www.leginfo.ca.gov/calaw.html. * The epidemiology of TB in the United States has changed dramatically since the early 1990s. Immigration from countries with a high prevalence of TB contributes substantially to the continued high rates of disease and transmission among foreign-born persons. In 2003, the rate of TB among foreign-born persons in the Untied States was 8.7 times higher than the rate for persons born in the United States. More than half of new TB cases in 2003 occurred in foreign-born persons, particularly those from Mexico, the Philippines, and Vietnam. Of 114 patients in whom multi-drug resistant TB (MDR TB) were diagnosed, foreign-born persons accounted for 95 (83%) cases (6). Detention facilities and local jails frequently contract with U.S. Immigration and Customs Enforcement (ICE) to house detainees, a practice that should be accounted for in assessing a facility's risk status. † Therapy that involves providing the anti-TB drugs directly to the patient and watching as the patient swallows the medications. DOT is the preferred core management strategy for all patients with TB. DOT for LTBI is referred to sometimes as directly observed preventive therapy. § Formerly called a negative pressure isolation room, an AII room is a single -occupancy patient-care room used to isolate persons with suspected or confirmed infectious TB disease. Environmental factors are controlled in AII rooms to minimize the transmission of infectious agents that are usually spread from person to person by droplet nuclei associated with coughing or aerosolization of contaminated fluids. AII rooms should provide negative pressure in the room so clean air flows under the door gap into the room, an air flow rate of 6--12 air changes per hour (ACH), and direct exhaust of air from the room to the outside of the building or recirculation of air through a high efficiency particulate air (HEPA) filter. ¶ ACH is the ratio of the volume of air entering the room or booth per hour to the volume of that room or booth. It equals the exhaust airflow (Q) in cubic feet per minute (cfm) divided by the volume of the room or 3 booth (V) in cubic feet (ft ) multiplied by 60 minutes per hour, as expressed thus: ** Surgical masks should never be worn in place of a respirator. Surgical masks often fit so poorly that they provide only minimal protection from any airborne hazard, including M. tuberculosis. Surgical masks are designed to protect others from the wearer; they are not designed or tested to provide respiratory protection to the wearer. †† Asymptomatic contacts with normal chest radiographs typically do not require isolation. §§ Because being immunocompromised (having pathologic or iatrogenic immune suppression, e.g., HIV infection or chemotherapy) is a risk factor for TB disease, correctional workers should be educated on the relation between TB and medical conditions associated with being immunocompromised. Correctional workers should be encouraged to discuss known or possible immunocompromising conditions with their private physicians or health-care professionals. ¶¶ Public health departments typically track treatment completion rates for patients referred to their care. Table 1 Return to top. Table 2 Return to top. Table 3 Return to top. Table 4 Return to top. Table 5 Return to top. Table 6 Return to top. Table 7