COVID-19 Correctional Pandemic Response Plan, VitalCore Health Strategies, 2020
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
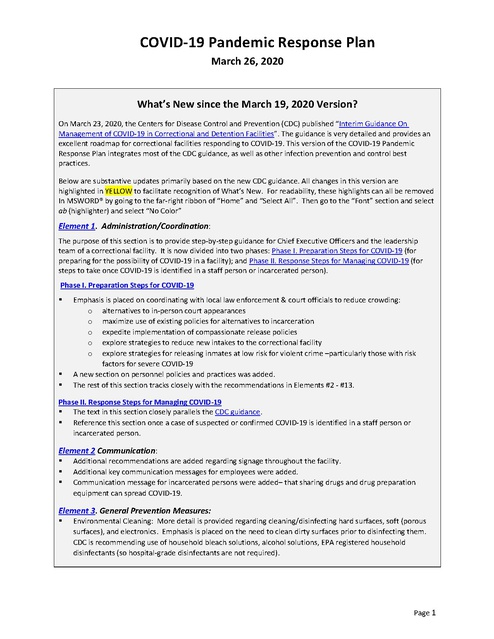
COVID-19 Pandemic Response Plan March 26, 2020 What’s New since the March 19, 2020 Version? On March 23, 2020, the Centers for Disease Control and Prevention (CDC) published “Interim Guidance On Management of COVID-19 in Correctional and Detention Facilities”. The guidance is very detailed and provides an excellent roadmap for correctional facilities responding to COVID-19. This version of the COVID-19 Pandemic Response Plan integrates most of the CDC guidance, as well as other infection prevention and control best practices. Below are substantive updates primarily based on the new CDC guidance. All changes in this version are highlighted in YELLOW to facilitate recognition of What’s New. For readability, these highlights can all be removed In MSWORD® by going to the far-right ribbon of “Home” and “Select All”. Then go to the “Font” section and select ab (highlighter) and select “No Color” Element 1. Administration/Coordination: The purpose of this section is to provide step-by-step guidance for Chief Executive Officers and the leadership team of a correctional facility. It is now divided into two phases: Phase I. Preparation Steps for COVID-19 (for preparing for the possibility of COVID-19 in a facility); and Phase II. Response Steps for Managing COVID-19 (for steps to take once COVID-19 is identified in a staff person or incarcerated person). Phase I. Preparation Steps for COVID-19 § § § Emphasis is placed on coordinating with local law enforcement & court officials to reduce crowding: o alternatives to in-person court appearances o maximize use of existing policies for alternatives to incarceration o expedite implementation of compassionate release policies o explore strategies to reduce new intakes to the correctional facility o explore strategies for releasing inmates at low risk for violent crime –particularly those with risk factors for severe COVID-19 A new section on personnel policies and practices was added. The rest of this section tracks closely with the recommendations in Elements #2 - #13. Phase II. Response Steps for Managing COVID-19 § The text in this section closely parallels the CDC guidance. § Reference this section once a case of suspected or confirmed COVID-19 is identified in a staff person or incarcerated person. Element 2 Communication: § § § Additional recommendations are added regarding signage throughout the facility. Additional key communication messages for employees were added. Communication message for incarcerated persons were added– that sharing drugs and drug preparation equipment can spread COVID-19. Element 3. General Prevention Measures: § Environmental Cleaning: More detail is provided regarding cleaning/disinfecting hard surfaces, soft (porous surfaces), and electronics. Emphasis is placed on the need to clean dirty surfaces prior to disinfecting them. CDC is recommending use of household bleach solutions, alcohol solutions, EPA registered household disinfectants (so hospital-grade disinfectants are not required). Page 1 COVID-19 Pandemic Response Plan March 26, 2020 What’s New since the March 19, 2020 Version? (continued) § § Social distancing measures: Additional examples of social distancing measures are included. Infection prevention & control guidance for staff screening visitors, staff, and new intakes was added. Element 4. Visitors / Volunteers / Contractors / Lawyers: § § If visits are continuing, post signage to instruct visitors to postpone visits if respiratory illness. Screen visitors for symptoms and a temperature prior to entry. Attachment 1a. Visitor Screening form was added . Element 5. Employee Screening: § Attachment 1b. Employee Screening form was revised. Element 6. New Intake Screening: § Attachment 2. New Intake Screening form was revised. Element 8. Personal Protective Equipment: § § N95 respirators are generally preferred over face masks, if available. Table 3. COVID-19 Personal Protective Equipment Recommendations provides an at-a-glance chart to identify the type of PPE to be used in various situations. Consider posting this throughout your facility. Element 10. Isolation (Symptomatic Persons): § § § § § Ideally isolation will occur in a private room with a bathroom attached. CDC provides guidance on the order of preference for rooms for isolating inmates. Cohorting is a last resort option. If possible, designated custody staff should be assigned to monitor isolated individuals to minimize exposures. Specific guidance regarding handling isolation room laundry is provided. Specific guidance regarding handling food service items is provided. Information is provided regarding cleaning spaces where COVID-19 cases spent time. Element 11. Care for the Sick: § Identify if ill persons have risk factors for COVID-19 complications. Those with increased risk should be monitored more closely. Implement telemedicine or provider-to-provider consultations for management of COVID-19 patients. Element 12. Quarantine: § § § § § § Close contact to COVID-10 is defined and discussed CDC recommends that close contacts be quarantined individually if feasible. Cohorting multiple quarantined close contacts could result in transmission of COVID-19 to persons who are uninfected so should only be practiced if there are no other available options. CDC provides guidance on the order of preference for rooms for quarantining inmates CDC recommends that PPE for quarantine include: face mask, eye protection, gloves. A gown should be worn if close contact with a quarantined person is anticipated. Attachment 4. Quarantine Room Sign was revised. Element 13. Data Collection, Analysis and Reporting was added. Element 14. Summary, Evaluation and Continuous Quality Improvement was added. Page 2 COVID-19 Pandemic Response Plan March 26, 2020 Plan Overview (March 16, 2020) COVID-19 presents unique challenges for containment in the confined correctional environment. Knowledge about COVID-19 and public health guidance for responding to this Pandemic is evolving quickly. Adaptable and updatable practical tools are needed to develop infection prevention and control plans for COVID-19 across a diverse array of U.S. jails and prisons. This COVID-19 Correctional Pandemic Response Plan provides an outline of infection prevention and control information that should be considered for correctional facilities related to a COVID-19 response. The plan outline is paired with a fillable MS WORD® Implementation Worksheet that can be easily customized to address local issues of concern for the facility and affected community. The 1918-19 influenza pandemic provides important lessons for responding to COVID-19. During the 1918–19 influenza (“flu”) pandemic, certain cities fared better than others. Those U.S. cities that both acted promptly to control the flu and implemented multiple layers of protective measures had fewer flu cases and lower overall mortality. This VitalCore COVID-19 Correctional Response Plan includes multiple layers of protective measures to minimize the impact of the virus in the correctional environment. The Response Plan is divided into 14 response elements. Each element is outlined in the plan with a corresponding section of the Implementation Worksheet. When completing the Worksheet, it is recommended to reference the corresponding text in the Response Plan. This worksheet can be readily adapted to meet the unique challenges of a specific facility. This COVID-19 Correctional Response Plan is based upon current guidance from the CDC that is adapted for the correctional setting. It is anticipated that the CDC guidance will continue to change so the plan will require updating accordingly. Effective response to the extraordinary challenge of COVID-19 is going to require that all disciplines in a correctional facility come together to develop, modify and implement plans as information and conditions change. Swift, decisive, yet evidenced-based planning is paramount. I hope you find this document useful in advancing our collective efforts to better ensure the health and safety of our correctional workers and our incarcerated patient populations. Viola Riggin, CEO VitalCore Health Strategies Approved by: Lannette Linthicum, MD, VitalCore Medical Consultant Developed by: Sarah Bur, MPH, RN, VitalCore Consultant Newton E. Kendig, MD, VitalCore Consultant Page 3 COVID-19 Pandemic Response Plan March 26, 2020 Table of Contents COVID-19 Overview .................................................................................................. 5 COVID-19 Pandemic Response Plan Elements ........................................................... 6 1. Administration/Coordination ............................................................................. 6 2. Communication ................................................................................................ 10 3. General Prevention Measures .......................................................................... 11 4. Visitors / Volunteers / Contractors / Lawyers .................................................. 15 5. Employee Screening ......................................................................................... 15 6. New Intake Screening ....................................................................................... 15 7. Initial Management and Testing of Cases of Respiratory Illness ..................... 16 8. Personal Protective Equipment (PPE) and Other Supplies ............................... 17 9. Transport .......................................................................................................... 20 10. Isolation (Symptomatic Persons) ................................................................... 20 11. Care for the Sick ............................................................................................ 22 12. Quarantine (Asymptomatic Exposed Persons)............................................... 23 13. Data Collection, Analysis & Reporting ........................................................... 24 14. Summary, Evaluation and Continuous Quality Improvement (CQI) .............. 25 COVID-19 Pandemic Response Plan Implementation Worksheet .............................26 Attachment 1a. COVID-19 Visitor Screening Form ..................................................37 Attachment 1b. COVID-19 Employee Screening Form .............................................38 Attachment 2. COVID-19 New Intake Screening Form ............................................39 Attachment 3. Respiratory Infection Isolation Room Sign ........................................40 Attachment 4. Quarantine Room Sign ....................................................................42 TABLE 3. COVID-19 Personal Protective Equipment Recommendations………………..19 Page 4 COVID-19 Pandemic Response Plan March 26, 2020 COVID-19 Overview This guidance provides general information regarding the COVID-19 pandemic and will be updated regularly. What is Coronavirus Disease 2019 (COVID-19)? Coronavirus Disease 2019 (COVID-19) is a respiratory illness that can spread from person-to-person. The virus that causes COVID-19 is a Novel Coronavirus that was first identified during an investigation into an outbreak in Wuhan, China and is now causing an International Pandemic. How is the virus causing COVID-19 transmitted? The virus is thought to spread mainly between people who are in close contact with one another (within approximately 6 feet) through respiratory droplets produced when an infected person coughs or sneezes. It also may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes. What are the symptoms of COVID-19? Patients with COVID-19 have had mild to severe respiratory illness with symptoms of: § Fever § Cough § Shortness of breath Complications of COVID-19 can include pneumonia, multi-organ failure, and in some cases death. How can I help protect myself? People can help protect themselves from respiratory illness with everyday preventive actions. § Avoid close contact with people who are sick. § Avoid touching your eyes, nose, and mouth with unwashed hands. § Wash your hands often with soap and water for at least 20 seconds. § Use an alcohol-based hand sanitizer that contains at least 60% alcohol if soap and water are not available. How long does it take for symptoms to develop? The estimated incubation period (the time between being exposed and becoming ill) averages 5 days after exposure with a range of 1-14 days. Is there a vaccine? There is currently no vaccine to protect against COVID-19. The best way to prevent infection is to take everyday preventive actions, like avoiding close contact with people who are sick and washing your hands often. Is there a treatment? There is no specific antiviral treatment for COVID-19. People with COVID-19 can seek medical care to help relieve symptoms. Page 5 COVID-19 Pandemic Response Plan March 26, 2020 COVID-19 Pandemic Response Plan Elements 1. Administration/Coordination This section on Administration/Coordination is designed for use by Chief Executive Officers to provide a broad overview of the plan. The subsequent elements provide detailed information about how to implement the plan. This section is divided into two phases: PHASE I. PREPARATION STEPS for COVID- 19 summarizes activities that all correctional facilities should be engaged in while preparing for the possibility of COVID-19 in the facility. These steps can be used as an outline for daily meetings about COVID-19 to quickly review the status of plan implementation. PHASE II. RESPONSE STEPS for MANAGING COVID-19 summarizes activities that should be implemented after case(s) of suspected or confirmed COVID-19 have been identified in the facility in either a staff person or incarcerated person. PHASE I. PREPARATION STEPS for COVID-19 a) Coordination of Facility Response § It is critically important that correctional and health care leadership meet regularly to review the current status of COVID-19, review updated guidance from the Centers for Disease Control and Prevention (CDC) and flexibly respond to changes in current conditions. § Regular meetings should be held, roles and responsibilities for various aspects of the local response determined, and evidence-based plans developed and rapidly implemented. § Consideration should be given to activating the Incident Command System within the facility to coordinate response to the crisis. § Responsibility should be assigned for tracking National and Local COVID-19 updates. b) Coordination with local law enforcement and court officials to minimize crowding. § Explore alternatives to in-person court appearances. § Maximize use of existing policies for alternatives to incarceration. § Expedite implementation of compassionate release policies. § Explore strategies to reduce new intakes to the correctional facility. § Explore strategies for releasing inmates at low risk for violent crime –particularly those with risk factors for severe COVID-19. c) Review Personnel Policies and Practices § Review the sick leave policies of each employer in the facility to determine which officials will have authority to send symptomatic staff home. § Review/revise/devise telework policies. § Review contingency plans for reduced staffing. Page 6 COVID-19 Pandemic Response Plan March 26, 2020 § Consider offering alternative duties to staff at higher risk of severe illness with COVID-19. § Remind staff to stay at home if they are sick § Institute employee screening of all employees (see Element #5) § Send staff home if they are identified with identified symptoms (fever, cough or shortness of breath) and advise to follow CDC recommended steps for persons with COVID-19 symptoms § Utilize following criteria for symptomatic staff to return to work: § o no fever for at least 72 hours (i.e., 3 full days of no fever without use of medicine that reduces fever); AND o other symptoms improved (e.g., cough or shortness of breath have improved); AND o at least 7 days have passed since symptoms first appeared Identify staff with COVID-19 Exposures (see definition of close contact in Element #12) o If a staff member has a confirmed COVID-19 infection, inform other staff about possible exposure to COVID-19 (maintaining confidentiality per American with Disabilities Act. o Decide if exposed staff will self-quarantine for 14-days or work wearing face mask. § NOTE: CDC recommends that employees, who are COVID-19 close contacts, self-monitor for symptoms and, if feasible—given staffing constraints—be under self-quarantine for 14 days. If due to staffing constraints, self-quarantine is determined not to be feasible, then asymptomatic exposed staff should come to work and wear a face mask (cloth or disposable) while working, with frequent hand hygiene. d) Communication (Element #2): § Initiate and maintain ongoing communication with local public health authorities § Communicate with community hospital about procedures for transferring severely ill inmates. § Develop and implement ongoing communication plans for staff, incarcerated persons, and families. e) Implement General Prevention Measures (Element #3) § Promote good health habits among employees (Table 1) o Review current policy regarding alcohol-based hand sanitizer and consider relaxing restrictions to allow more staff to carry individual-sized bottles for hand hygiene. § Conduct frequent environmental cleaning of high touch surfaces. Increase number of inmate workers assigned to this duty. § Institute social distancing measures to prevent spread of germs. Review list of possible measures listed in Element #3 and develop plans for your facility. o Make decisions about movement § Minimize movement both within the facility and between facilities Page 7 COVID-19 Pandemic Response Plan March 26, 2020 § o Consider restricting transfers of incarcerated persons to and from other jurisdictions unless necessary for medical evaluation, isolation/quarantine, clinical care, extenuating security concerns or to prevent overcrowding. Postpone non-urgent outside medical visits § Employees stay at home if sick. Review communications with employees about this. § If influenza vaccination is still in stock offer to unvaccinated staff (higher priority) and incarcerated persons. § Implement infection prevention control guidance for staff doing screening (of visitors, employee, new intakes) (Element #3) f) Make decisions about access for visitors, volunteers, contractors and lawyers (Element #4) § Communicate with potential visitors § Institute screening of visitors for symptoms and temperature (Attachment #1a) g) Institute Employee Screening (Element #5) (Attachment #1b) h) Institute New Intake Screening (Element #6) (Attachment #2) i) Appropriately manage and test symptomatic incarcerated persons (Element #7) § Suspend co-pays for incarcerated persons seeking medical evaluation for respiratory symptoms. j) Attempt to acquire needed personal protective equipment (PPE) and other supplies (Element #8) § Ensure that sufficient stocks of hygiene supplies, cleaning supplies, personal protective equipment (PPE) , and medical supplies are available and there is a plan in place for re-stocking. § Review Table 3. COVID-19 Personal Protective Equipment Recommendations and post as needed in facility. § Implement staff training on donning and doffing PPE. k) Assure that transport officers have received training on safe transport utilizing PPE (Element #9). § Identify staff who will provide transport l) Identify rooms to be used for isolation (Element #10) and quarantine (Element #12). § NOTE: CDC strongly recommends single rooms for persons isolated and quarantined. Cohorting of groups of persons should be done as a last resort. § Print out color isolation and quarantine signs for future use (Attachment #3 & Attachment #4). § Discuss how custody staff will be assigned to work in isolation/quarantine rooms. Page 8 COVID-19 Pandemic Response Plan March 26, 2020 § Appropriately train staff and incarcerated workers who work in laundry and food service. § Train staff and incarcerated workers on how to clean spaces where COVID-19 workers spent time. m) Health services should review procedures for caring for the sick (Element #11) § Maintain communication with public health authorities to determine how COVID-19 testing will be performed and recommended criteria for testing § Explore options for expanding telehealth capabilities. PHASE II. RESPONSE STEPS for MANAGING COVID-19 n) Implement alternative work arrangements, as deemed feasible. o) Suspend all transfers of incarcerated persons to and from other jurisdiction and facilities unless necessary for medical evaluation, medical isolation/quarantine, extenuating security concerns, or to prevent over-crowding. p) When possible, arrange for lawful alternatives to in-person court appearances. q) Consider quarantining all new intakes for 14 days before they enter the facility’s general population, if feasible. r) Incorporate screening for COVID-19 symptoms and a temperature check into release planning. Provide inmates who are under isolation or quarantine who are releasing with education about recommended follow-up. s) Coordinate with local public health authority regarding persons being isolated/quarantined with COVID-19. t) Communicate with community hospital regarding potential need to transfer severely ill inmates. u) Hygiene: § Continue to ensure that hand hygiene supplies are well-stocked in all areas of the facility. § Continue to emphasize practicing good hand hygiene and cough etiquette v) Environmental Cleaning: § Continue emphasis on cleaning and disinfection especially on frequently touched surfaces § Reference specific cleaning and disinfection procedures for areas where a COVID-19 case spent time (Element #10) Page 9 COVID-19 Pandemic Response Plan March 26, 2020 x) Implement medical isolation of confirmed or suspected COVID-19 cases (see Element #10). Implement telehealth modalities as much as possible. y) Implement quarantine of close contacts of COVID-19 cases (see Element #12). z) Implement system for tracking information about incarcerated persons and staff with suspected/confirmed COVID-19 and quarantined persons (Element #13). 2. Communication § The importance of regular communication with staff, the incarcerated population, and their families cannot be over-emphasized. You cannot communicate too much. § Specific methods of communication for all groups should be established. Staff should be assigned to be responsible for crafting and disseminating regular updates. § Post signage throughout the facility communicating the following: o For all: symptoms of COVID-19 and hand hygiene instructions o For incarcerated/detained persons: report symptoms to staff o For staff: stay at home when sick; if symptoms develop while on duty, leave the facility as soon as possible and follow CDC-recommended steps for persons who are ill with COVID-19 symptoms. o Ensure that signage is understandable for non-English speaking persons and those with low literacy § During COVID-19, group educational sessions should be avoided and instead, communicate with electronic and paper methods of communication. § Key communication messages for employees include: o Symptoms of COVID-19 and its health risks o Reminders about good health habits to protect themselves, emphasizing hand hygiene. o The importance of staying home if signs and symptoms of fever, cough, or shortness of breath or if known close contact with a person with COVID-19. o Review of sick leave policy o If staff develop fever, cough, or shortness of breath at work: immediately put on a face mask, inform supervisor, and leave facility, and follow CDC recommended steps for persons who are ill with COVID-19 symptoms. o Elements of the facility COVID-19 Response Plan to keep employees safe, including social distancing. § Key communication messages to incarcerated persons: o The importance of reporting fever and/or cough or shortness of breath (and reporting if another incarcerated person is coughing in order to protect themselves). Indicate how these reports should be made. o Reminders about good health habits to protect themselves, emphasizing hand hygiene. o Communicate that sharing drugs and drug preparation equipment can spread COVID-19. o Plans to support communication with family members (if visits are curtailed). o Plans to keep incarcerated persons safe, including social distancing. Page 10 COVID-19 Pandemic Response Plan March 26, 2020 § Key communication messages for families: o Information about visiting. If visiting is curtailed information about alternatives to in-person visits. o What the facility is doing to keep incarcerated persons safe. § Local public health authorities: Contact should be made and maintained with local public health authorities to get local guidance, especially with regard to managing and COVID-19 testing of persons with respiratory illness. § Local hospital: Communication should also be established with your local community hospital to discuss referral mechanisms for seriously ill incarcerated persons. 3. General Prevention Measures Throughout the duration of the COVID-19 pandemic the following general prevention measures should be implemented to interrupt viral infection transmission. These are listed in Table 1 below. Table 1. General Prevention Measures a. Promote good health habits among employees and incarcerated individuals: 1) Avoid close contact with persons who are sick. 2) Avoid touching your eyes, nose, or mouth. 3) Wash your hands often with soap and water for at least 20 seconds. 4) Cover your sneeze or cough with a tissue (or into a sleeve). Then throw the tissue in the trash. 5) Avoid non-essential physical contact. Avoid handshakes, “high-fives” b. Conduct frequent environmental cleaning of “high touch” surfaces. c. Institute social distancing measures to prevent spread of germs, e.g., minimize selfserve foods, minimize group activities. d. Employees stay at home if they are sick. e. Influenza (flu) vaccine is recommended for persons not previously vaccinated. f. Infection prevention and control guidance for persons doing screening (visitors, employees, new intakes) a. Good Health Habits § Good health habits should be promoted in various ways, i.e., educational programs, posters, campaigns, assessing adherence with hand hygiene, etc. § This CDC website has helpful educational posters: § Each facility should assure that adequate supplies and facilities are available for hand washing for both incarcerated individuals and employees, including: soap, running water, hand drying machines or disposable paper towels. § Provide tissues and no-touch trash receptacles for disposal. § With approval of the Chief Executive Officer (CEO), health care workers should have access Page 11 COVID-19 Pandemic Response Plan March 26, 2020 to alcohol-based hand rub. § Provisions should be made for employees and visitors and new intakes to wash their hands when they enter the facility. b. Environmental Cleaning § The frequency of routine cleaning of surfaces that are frequently touched should be increased. These can include doorknobs, keys, handrails, telephones, computer keyboards, elevator buttons, cell bars, etc. § One strategy is to increase the number of incarcerated individuals who are assigned to this duty. § Hard Surfaces: o If surfaces are dirty, they should be cleaned using a detergent or soap and water prior to disinfection. o For disinfection, diluted household bleach solutions, alcohol solutions with at least 70% alcohol, and most common EPA-registered household disinfectants should be effective. § Diluted, unexpired household bleach can be used if appropriate for the surface. Never mix household bleach with ammonia or any other cleanser. § Prepare bleach solution by mixing: 5 tablespoons (1/3 cup) bleach per gallon of water or 4 teaspoons of bleach per quart of water § Soft (porous) surfaces, i.e., carpeted floor, rugs, drapes o Remove visible contamination and clean with appropriate cleaners for these surfaces o If washable, launder in hottest water setting for the item and dry completely o Otherwise, use products with EPA-approved viral pathogens claims § Electronics cleaning and disinfection o For electronics such as tablets, touch screens, keyboards, and remote controls, remove visible contamination if present. o Follow the manufacturer’s instructions for all cleaning and disinfection products. o Consider use of wipeable covers for electronics. o If no manufacturer guidance is available, consider the use of alcohol-based wipes or spray containing at least 70% alcohol to disinfect touch screens and other surfaces. Dry surfaces thoroughly to avoid pooling of liquids. c. Social Distancing Measures Strategies for social distancing are myriad and markedly dependent on local factors. Various administrative measures should be implemented to reduce contact between people and reduce chance of spreading viruses. It is recommended that an interdepartmental brainstorming meeting be held to discuss what would work in your facility. Examples of such measures include: Page 12 COVID-19 Pandemic Response Plan March 26, 2020 § § § § § § § Common areas o Enforce increased space between individuals in holding cells, as well as in lines and waiting areas such as intake (e.g., remove every other chair in a waiting area). Recreation o Choose recreation spaces where individuals can spread out o Stagger time in recreation spaces o Restrict recreation space usage to a single housing unit (where feasible), performing. o Disinfection between individual use of equipment and between groups o Eliminate close-contact sports, i.e., basketball, soccer o Emphasize individual activities, i.e., running, walking, jumping jacks o Stop the use of equipment that multiple people will touch Meals o Stagger meals o Rearrange seating in dining hall to increase space between individuals, e.g., remove every other chair and use only one side of a table o Minimizing self-serve foods, e.g., eliminate salad bars o Provide meals inside housing units or cells Group activities o Limit size of group activities o Increase space between individuals during group activities o Consider alternatives to existing group activities, in outdoor areas or other areas where individuals can spread out o Suspend group programs* *Note: With discontinuation of group activities, it is vitally important to creatively identify and provide alternative forms of activity to support the mental health of incarcerated individuals during the pandemic. Education o Convert curriculum to self-study o Provide education through use of video modalities Housing o Arrange bunks so that individuals sleep head to foot o Rearrange scheduled movements to minimize mixing of individuals from different housing units o Ensure thorough cleaning/disinfection of living space when inmates leave o If space allows, reassign bunks to provide more space between individuals (ideally 6 feet or more in all directions Medical o Leverage telehealth modalities, e.g., tele-video and provider to provider consultation o If possible, designate a room near each housing unit to evaluate individuals with COVID-19 symptoms o Designate a room near intake area to evaluate new intakes with identified COVID-19 symptoms or exposure risk before they move to other parts of facility o Discontinue pill-lines and administering medication on units Page 13 COVID-19 Pandemic Response Plan March 26, 2020 Assure that inmates who come to sick call with respiratory symptoms are immediately placed in separate room with mask on and perform hand hygiene. Minimize inmate movement o Minimize transferring of inmates between units o Stopping movement in and/or out o Suspending work release programs Providing virtual visits o § § d. Sick/exposed employees remain home § COVID-19 could gain entrance to a facility via infected employees. Staff should be educated to stay home if they have fever and respiratory symptoms. § If employees become sick at work, they should be advised to promptly report this to their supervisor and go home. § Employees should be advised to consult their health care provider by telephone. § Employees who are sick should be advised to follow CDC guidance on What to do if you are sick? § Determine employee policy regarding quarantine, i.e., exposed employees self-quarantine for 14 days or come to work wearing a facemask and frequent hand hygiene. Exposed staff should promptly report symptoms if they occur. e. Influenza vaccination § While influenza season is still ongoing flu vaccination remains an important measure to prevent an illness that presents similarly to COVID-19. § If there is influenza vaccine still in stock, unvaccinated staff (highest priority) and incarcerated persons should be offered the flu vaccine. f. Infection prevention & control guidance for staff screening visitors, staff, and new intakes. The following is a protocol to safely check an individual’s temperature: o Perform hand hygiene o Put on a face mask, eye protection (goggles or disposable face shield that fully covers the front and sides of the face) and a single pair of disposable gloves* o Check individual’s temperature § Non-contact or disposable thermometers are preferred over reusable oral thermometers. § If disposable or non-contact thermometers are used and the screener did not have physical contact with an individual, gloves do not need to be changed before the next check. If non-contact thermometers are used, they should be cleaned routinely as recommended by CDC for infection control. § If performing oral temperature check on multiple individuals, ensure that a clean pair of gloves is used for each individual and that the thermometer has been thoroughly disinfected in between each check. o Remove and discard PPE o Perform hand hygiene Page 14 COVID-19 Pandemic Response Plan March 26, 2020 * Note: CDC recommends wearing a gown for this process. Given the current shortage of gowns in many facilities this is not routinely recommended in this plan. 4. Visitors / Volunteers / Contractors / Lawyers § Consideration should be given to begin limiting access to the facility by visitors and volunteers and non-essential contractors. o Arrangements should be made to increase options for incarcerated persons to communicate with their families via telephone or tele-video. § If possible, legal visits should occur remotely. § Communicate with potential visitors instructing them to postpone visits if they have respiratory illness. Post signage regarding visitor screening. § All visitors should be screened for symptoms and a temperature taken prior to entry utilizing the form in Attachment 1a. 5. Employee Screening § In locations where it is identified that there is sustained COVID-19 community transmission, employees should be screened upon arrival with a temperature, and asked questions about respiratory symptoms and if they have had contact with a known COVID-19 patient (Attachment 1b). § This form can be laminated for employees to review the questions for individuals to verbally respond to them. § A temperature should also be taken ideally with a no-touch infra-red thermometer. § Employee screenings do not require documentation unless the person responds “YES” to any question or has a temperature. § Screening can be performed by any staff person with training. § Employees who screen positive for symptoms should be sent home and advised to consult their healthcare provider. § Employees who have had close contact with a COVID-19 case should self-monitor for symptoms (i.e., fever, cough, or shortness of breath) and, if feasible given staffing constraints, be under selfquarantine for 14 days. If due to staffing constraints, self-quarantine is not feasible, asymptomatic exposed staff should come to work and wear a face mask (cloth or disposable) while working, with frequent hand hygiene. 6. New Intake Screening § New intakes should be screened per usual protocols. Consider conducting this screening outdoors or in a covered area (weather and logistics permitting). § Temperature should be taken, ideally with an infra-red no-touch thermometer with staff wearing PPE as described in Element #3f. Page 15 COVID-19 Pandemic Response Plan March 26, 2020 § Additional questions should be asked regarding symptoms and exposure to COVID-19 (Attachment 2). § New arrivals should be segregated from other incarcerated individuals until the screening process has been completed. § If new intakes are identified with symptoms then immediately place a face mask on the person, have the person perform hand hygiene, and place them in a separate room with a toilet while determining next steps. Staff entering the room shall wear personal protective equipment (PPE) in accordance with guidance in Element #8. § Identify incarcerated persons who were transferred with the symptomatic new intake for need for quarantine (see Element #12). § If new intakes report history of exposure to COVID-19 then they should be placed in quarantine (see Element #12). 7. Initial Management and Testing of Cases of Respiratory Illness § Source control (placing a mask on a potentially infectious person) is critically important. If individuals are identified with symptoms, then immediately place a face mask on the patient and have them perform hand hygiene. § Place them in a separate room with a toilet and sink while determining next steps. If the facility has an airborne infection isolation room this could be used for this purpose. Staff in the same room shall wear personal protective equipment (PPE) as outlined in Element #8. § Decisions about how to manage and test incarcerated persons with mild respiratory illness should be made in collaboration with public health authorities. The vast majority of persons with respiratory illness will not have COVID-19, especially during seasonal flu season. It is unlikely that hospitals will have the capacity to evaluate incarcerated persons with mild respiratory illness. § The CDC current priorities for testing are listed at this link. § CDC recommendations for clinical specimens for COVID-19 include collecting and testing upper respiratory tract specimens (nasopharyngeal swab). New (3/24/20) CDC recommendation indicate that if nasopharyngeal swabs are not feasible that nasal swabs are an acceptable alternative. CDC also recommends testing lower respiratory tract specimens, if available. For patients who develop a productive cough, sputum should be collected and tested for COVID-19. Note: rapid blood tests for COVID-19 have become commercially available that test for IgG and IgM. These indicate that the results should not be the sole basis to diagnose or exclude infection. Therefore, at this time it is recommended that these tests not be used. § If feasible, during flu season it is recommended that rapid flu tests with nasopharyngeal swab be performed. It is important that nasopharyngeal swabs be performed correctly. § Nasopharyngeal swabbing should only be performed by staff with demonstrated competency. See instructional video at: https://www.youtube.com/watch?v=DVJNWefmHjE § Suspend co-pays for incarcerated persons seeking medical evaluation for respiratory symptoms. Page 16 COVID-19 Pandemic Response Plan March 26, 2020 8. Personal Protective Equipment (PPE) and Other Supplies PERSONAL PROTECTIVE EQUIPMENT § The CDC recommends the following PPE when a person comes into contact with a person with suspected or confirmed COVID-19. o N95 respirator or face mask § N95 respirators are preferred. When N95 respirators are in short supply they should be reserved first for use when a patient is undergoing an aerosol-generating procedure including testing for COVID-19 and second for confirmed COVID-19 patients. § N95 respirators should not be worn with facial hair that interferes with the respirator seal. § If N95 respirators are to be used, they must be used in the context of a fit-testing program. Fit testing is specific to the brand/size of respirator to be used. Table 2. Definitions of “Face Masks” and “Respirators” Face Masks: Disposable FDA-approved masks, which come in various shapes and types (e.g., flat with nose bridge and ties, duck billed, flat and pleated, pre-molded with elastic bands). Respirators: N-95 or higher filtering, face-piece respirators that are certified by CDC/NIOSH. o Gown § If gowns are in short supply they can be reserved for times when direct, close contact with a patient is being implemented. o Gloves o Eye Protection (goggles or disposable face shield that fully covers the front and sides of the face). § This does not include personal eyeglasses. § If reusable eye protection is used, it should be cleaned and disinfected in accordance with manufacturer’s instructions. § It is strongly emphasized that hand hygiene be performed before and after donning and doffing PPE. § Staff who are wearing PPE should be trained on its use. CDC instructions on donning and doffing PPE are available at: https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf. § Inventory current supplies of PPE. § CDC (3/17/20) has published new recommendations on strategies to use in the absence of available PPE. § Criteria for using various types of PPE based upon the situation is outlined in Table 3 (next page). § Make contingency plans for the probable event of PPE shortages during the COVID-19 pandemic (see CDC guidance on optimizing PPE supplies). CDC now recommends that in the case of shortage of disposable face masks that re-usable cloth masks can be considered. Page 17 COVID-19 Pandemic Response Plan March 26, 2020 OTHER SUPPLIES § Other supplies that should be obtained and inventory tracked include: o o o o o o o o Standard medical supplies and pharmaceuticals for daily clinic needs Tissues Liquid soap Bar soap Hand drying supplies Alcohol-based hand sanitizer containing at least 60% alcohol (where permissible based on security restrictions) Cleaning supplies, including EPA-registered disinfectants effective against the virus that causes COVID-19 Sterile viral transport media and sterile swabs to collect nasopharyngeal specimens if COVID-19 testing is indicated Page 18 COVID-19 Pandemic Response Plan March 26, 2020 Table 3. COVID-19 Personal Protective Equipment Recommendations Situation N95 Face respirator mask Eye protection Gloves Gown/ coveralls X X 1 X2 X X X X2 X X X X X X X X X X X X STAFF Staff performing temperature checks on: staff, visitors, or incarcerated/detained persons Isolation: Staff providing medical care for suspected/confirmed COVID-19 cases Isolation: Correctional staff entering isolation room Staff present during aerosolizing procedure on suspected or confirmed COVID-19 case (including testing) Staff handling laundry (from a COVID-19 case or case contact) Staff handling used food service items (from a COVID-19 case or case contact) Staff cleaning an area (where a COVID-19 case has spent time) Transport of suspected/confirmed COVID-19 Prior to & following transport (if close contact) Quarantine: No direct contact with asymptomatic persons who are close contacts to COVID-19 Quarantine: Direct contact with asymptomatic persons (including medical care/temperature checks) X X Additional PPE may be needed based on the disinfectant label. X2 During transport X2 X X X X X X X X X X X X X X X X INCARCERATED/DETAINED PERSONS Confirmed or suspected COVID-19 cases, or showing symptoms of COVID-19 Laundry worker (handling items from COVID-19 case or case contact) Food service worker (handling items from COVID-19 case or case contact) Worker performing cleaning (areas where COVID-19 case has spent time) Quarantine: Asymptomatic COVID-19 close contacts 3 X Additional PPE may be needed based on the disinfectant label. Apply face masks for source control, as feasible, based on local supply, especially if cohorted 1 Note: CDC recommends wearing a gown for this process. Given the current shortage of gowns in many facilities this is not routinely recommended in this plan. 2 A NIOSH-approved N95 is preferred. However, based on local and regional situational analysis of PPE supplies, face masks (including cloth face masks) are an acceptable alternative when the supply chain of respirators cannot meet the demand. During this time, available respirators should be prioritized for procedures that are likely to generate respiratory aerosols, which would pose the highest exposure risk to staff. 3 If a facility chooses to quarantine new intakes (without symptoms or known exposure to a COVID-19 case) before integrating into the facility’s general population, face masks are not necessary. Adapted from: CDC. Interim Guidance On Management of COVID-19 in Correctional and Detention Facilities (Table 1); 3/24/19. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctionaldetention.html#Min_Mod_Trans Page 19 COVID-19 Pandemic Response Plan March 26, 2020 9. Transport If a decision is made to transport a patient with signs and symptoms of severe respiratory illness, to a health care facility the following guidance should be followed regarding transport. § Notify the receiving health care facility of the pending transport of a potentially infectious patient. § Patient wears a face mask and performs hand hygiene. § Correctional officer wears face mask (or N-95 respirator). Wear gloves, gown, and eye protection if in close contact with inmate prior to transport. § Prior to transporting, all PPE (except for face mask / N-95 respirator) is removed and hand hygiene is performed. This is to prevent contaminating the driving compartment. § Ventilation system should bring in as much outdoor air as possible. Set fan to high. § DO NOT place air on recirculation mode. § Weather permitting, drive with the windows down. § Following the transport, if close contact with the patient is anticipated, put on new set of PPE. Perform hand hygiene after PPE is removed. § After transporting a patient, air out the vehicle for one hour before using it without a face mask or respirator. § When cleaning the vehicle wear a disposable gown and gloves. A face shield or face mask and goggles should be worn if splashes or sprays during cleaning are anticipated. § Clean and disinfect the vehicle after the transport utilizing instructions in Element #3b. Table 4. Definitions of “Isolation” and “Quarantine” Isolation: Confining individuals who are sick either to single rooms or by cohorting them with other viral infection patients. Quarantine: Confining asymptomatic persons who are contacts to COVID-19 while they are in the incubation period (up to 14 days for COVID-19). 10. Isolation (Symptomatic Persons) § Isolation Defined: A critical infection control measure for COVID-19 is to promptly separate incarcerated individuals who are sick with fever or respiratory symptoms away from other incarcerated individuals in the general population. Ideally isolation will occur in a private room with a bathroom attached. If not, incarcerated individuals will have to wear a face mask to go to the bathroom outside the room. § Cohorting: As a last resort option, persons with diagnosed COVID-19 can be cohorted together. Inmates with laboratory confirmed COVID-19 should be housed separately from those with undiagnosed respiratory illness. § § The CDC guidelines describe the order of preference of rooms for isolating inmates. Rooms where incarcerated individuals with respiratory illness are either housed alone or cohorted should be identified and designated “Respiratory Infection Isolation Room”. No Page 20 COVID-19 Pandemic Response Plan March 26, 2020 special air handling is needed. The door to the isolation room should remain closed. o § § § § § § § § § Note: The PPE requirements for COVID-19 do not fall into any one of the usual categories for the CDC transmission-based precautions, i.e., droplet, airborne, or contact. For the purposes of this document we have labeled the precaution sign “Respiratory Infection Isolation Room” since the rooms may house persons with undiagnosed respiratory infection as well as diagnosed COVID-19. Signage: A sign should be placed on the door of the room indicating that it is a Respiratory Infection Isolation Room that lists recommended personal protective equipment (PPE) (see Attachment 3) described in Element #8. Face Masks: If available—to minimize the likelihood of disease transmission—persons who are isolated or cohorted should wear a face mask while isolated. Face masks should be replaced as needed. It is particularly important for those cohorted with undiagnosed respiratory illness to wear a mask so that persons with respiratory illnesses other than COVID-19 are protected. Bunk beds: Depending on how ill the incarcerated individuals are, bunk beds may or may not be suitable. Assignment of custody staff: If feasible, designated custody staff should be assigned to monitor isolated individuals in order to minimize exposures. Provide individuals in isolation with tissues, and if permissible and available, a lined notouch trash receptacle. Dedicated medical equipment, i.e., blood pressure cuffs should be left in room (ideally) or decontaminated in accordance with manufacturer’s instructions. Masks outside of room: If individuals with respiratory illness must be taken out of the isolation room, they should wear a face mask and perform hand hygiene before leaving the room. Aerosol generating procedures: If a patient who is in isolation must undergo a procedure that is likely to generate aerosols (e.g., suctioning, administering nebulized medications, testing for COVID-19) they should be placed in a separate room. An N-95 respirator (not a face mask), gloves, gown, and face protection should be used by staff. Laundry: o Laundry from a COVID-19 cases can be washed with other individuals’ laundry. o Individuals handling laundry from COVID-19 cases should wear disposable gloves, discard after each use, and perform hand hygiene. o Do not shake dirty laundry. This will minimize the possibility of dispersing virus through the air. o Launder items using the hottest appropriate water setting and dry items completely. § Food service items. Cases under medical isolation should throw disposable food service items in regular trash in their medical isolation room. Non-disposable food service items should be handled with gloves and washed with hot water or in a dishwasher. Individuals handling used food service items should clean their hands after removing gloves. § Criteria for discontinuing isolation § For individuals who will NOT be tested to determine if they are still contagious: o The individual has been free from fever for at least 72 hours without the use of fever-reducing medications; AND o The individual’s other symptoms have improved (e.g., cough, shortness of breath); AND o At least 7 days have passed since the first symptoms appeared Page 21 COVID-19 Pandemic Response Plan March 26, 2020 For individuals who had a confirmed positive COVID-19 test but never showed symptoms: o At least 7 days have passed since the date of the individual’s first positive COVID-19 test; AND o The individual has had no subsequent illness Cleaning spaces where COVID-19 cases spent time o Close off areas used by infected individual. If possible, open outside doors and windows to increase air circulation in the area. o Wait as long as practical, up to 24 hours under the poorest air exchange conditions before beginning to clean and disinfect. o Ensure that persons performing cleaning wear recommended PPE for isolation (See Table 3). o Thoroughly clean and disinfect utilizing instructions in Element #3b with an emphasis on frequently touched surfaces. § § 11. Care for the Sick § There are no specific treatments for COVID-19 illness. Care is supportive. § Identify if ill persons have risk factors for COVID-19 complications. Those with increased risk should be monitored more closely. § Treatment consists of assuring hydration and comfort measures. The recipe for oral rehydration solution is in Table 4 below. § Acetaminophen is the preferred antipyretic for treating fever in most patients with COVID-19 considering its efficacy and safety profile. Ibuprophen is as an alternative, antipyretic choice; however, it can cause kidney damage and other adverse effects in some patients. Recent reports suggest that ibuprophen may worsen the course of COVID-19; however, this theoretical risk is still under investigation. § Patients should be assessed at least twice daily for signs and symptoms of shortness of breath or decompensation. § A low threshold should be used for making the decision to transport an inmate to the hospital if they develop shortness of breath. § Implement telemedicine or provider-to-provider consultations for management of COVID-19 patients. Page 22 COVID-19 Pandemic Response Plan March 26, 2020 Table 5. Oral Rehydration Solution Recipe 1-gallon clean water 10-tablespoons of sugar 4-teaspons salt Directions: Stir up. Do not boil. Can add sugar -free drink mix to flavor. Use within 24 hours. 12. Quarantine (Asymptomatic Exposed Persons) § The purpose of quarantine is to assure that incarcerated individuals who are known to have been exposed to the virus are kept separate from other incarcerated individuals to assess whether they develop viral infection symptoms. If cases of COVID-19 are identified, it may be appropriate to identify close contacts and quarantine them in a separate room or unit. § Close contact defined: In the context of COVID-19, an individual is considered a close contact if they have: o Been within 6 feet of a COVID-19 case for a prolonged period of time OR o Had direct contact with infectious secretions of a COVID-19 case Considerations when assessing close contact include the duration of exposure and the clinical symptoms of the person with COVID-19 (i.e., coughing likely increases exposure risk as does exposure to a severely ill patient). § Identification of Quarantine Rooms: Facilities should make every effort to quarantine close contacts of COVID-19 cases individually. Cohorting multiple quarantined close contacts could result in transmission of COVID-19 to person who are uninfected. Cohorting should only be practiced if there are no other available options. o If an entire housing unit is under quarantine due to contact with a case from the same housing unit, the entire housing unit may need to be treated as a cohort and quarantine in place. o Ideally do not cohort individuals who are at higher risk of severe illness from COVID-19. o CDC guidelines describe the order of preference for housing of inmates in quarantine. § Signage: The door to the Quarantine Room should remain closed. A sign should be placed on the door of the room indicating that it is a Quarantine Room which lists recommended personal protective equipment (PPE) (see Attachment 4). PPE includes face mask, eye protection, gloves, and a gown if close contact with a quarantined person is anticipated. § Face masks: (If there is a sufficient supply of face masks) To minimize the likelihood of disease transmission to persons cohorted in quarantine, quarantined persons should be required to wear a face mask. Face masks should be replaced as needed. § As feasible, the beds/cots of quarantined incarcerated individuals should be placed at least 6 feet apart. Page 23 COVID-19 Pandemic Response Plan March 26, 2020 § No Movement: Quarantined incarcerated individuals should be restricted from being transferred, having visits, or mixing with the general population. § PPE: A face mask, eye protection and gloves are recommended for staff who are in direct, close contact (within 6 feet) of asymptomatic quarantined incarcerated individuals. § Monitoring: CDC recommends that inmates in quarantine should be screened twice daily for symptoms including subjective fever, and a temperature. Symptomatic patients need to be isolated. Laundry: o Laundry from quarantined persons can be washed with other individuals’ laundry. o Individuals handling laundry from quarantined persons should wear disposable gloves, discard after each use, and clean their hands after. o Do not shake dirty laundry. This will minimize the possibility of dispersing virus through the air. o Launder items using the hottest appropriate water setting and dry items completely. o Clean and disinfect clothes hampers according to guidance above for surfaces. If permissible, consider using a bag liner that is either disposable or can be laundered. § § Meals should be provided to quarantined individuals in their quarantine spaces. Disposable food service items can be disposed of in regular trash. Individuals handling used food service items should wear gloves and dishes washed in hot water. Wash hands after removing gloves. § The duration of quarantine for COVID-19 is the 14-day incubation period. If a new case is identified in the quarantine unit then the 14-day quarantine period starts again. 13. Data Collection, Analysis & Reporting Implement systems for tracking information about incarcerated persons and staff with suspected/confirmed COVID-19 § Ill/Exposed Staff Persons: The following basic information should be tracked on a line list o Symptomatic Y/N o Date of symptom onset o Exposed? Y/N o Date of exposure o Current status (will change over time) § Exposed – Working § Exposed – Self-Quarantine § Person Under Investigation (PUI)- testing pending § PUI, test result pending § PUI, tested negative § Laboratory confirmed case Page 24 COVID-19 Pandemic Response Plan March 26, 2020 § o Date left work o Date returned to work Incarcerated Persons - Symptomatic: The following basic information should be tracked on a line-list: o Date of symptom onset o Reported symptoms (fever, cough, shortness of breath) o Date isolated o Influenza tested? Y/N o Influenza result o Date COVID-19 tested o Date COVID-19 test result o Result o Current status (will change over time) § Person Under Investigation (PUI)- testing pending § PUI, test result pending § PUI, tested negative § Laboratory confirmed case o Current housing: Isolation o Date isolation discontinued o Hospitalized Y/N o Hospitalization Date o Deceased Y/N NOTE: Incarcerated persons who are identified with suspected/confirmed COVID-19 must be reported to public health authorities. You will be asking questions about cases found on this CDC COVID-19 reporting form. § Incarcerated Persons – Exposed o Date of exposure o Current Housing § Quarantined – alone § Quarantined – cohort o Date quarantine discontinued o Developed signs and symptoms of COVID-19? Y/N o Date Isolated 14. Summary, Evaluation and Continuous Quality Improvement (CQI) Periodically and at the conclusion of the outbreak review the implementation of the COVID-19 Pandemic Response Plan and identify what has worked well and what has not worked well, total numbers of cases and contacts treated/evaluated. Engage the CQI committee in evaluating the facility pandemic response. Identify areas for improvement and report these recommendations to the leadership team. Page 25 COVID-19 Pandemic Response Plan March 26, 2020 COVID-19 Pandemic Response Plan Implementation Worksheet This MS Word® template worksheet is designed for facilities to operationalize the guidance in this COVID-19 Response Plan. It should be adapted to the unique needs of your facility. Date Updated: Completed by: 1. Administration/Coordination Coordination of Response Identify members of the facility leadership team responsible for COVID-19 response planning and implementation: Will the facility utilize the Incident Command System? YES NO If not, how will COVID-19 response plans be developed and implemented? Schedule regular meetings to review implementation of all elements listed in the Administration/Coordination section of the document. Who is responsible for monitoring COVID-19 updates from CDC and State Health Department? CDC Website: https://www.cdc.gov/coronavirus/2019-ncov/index.html State of _________ Website:_________________________________________________________ Coordinate response with local law enforcement and court officials. § Explore alternatives to in-person court appearances: § Maximize use of existing policies for alternatives to incarceration: § Expedite implementation of compassionate release policies: Page 26 COVID-19 Pandemic Response Plan March 26, 2020 § Explore strategies to reduce new intakes to the correctional facility: § Explore strategies for releasing inmates at low risk for violent crime –particularly those with risk factors for severe COVID-19: Personnel Policies and Practices. § Review the sick leave policies of each employer that operates in the facility. o Do policies actively encourage staff to stay home when sick? YES NO. If no, how will staff be encouraged to stay home if sick? o What officials will have the authority to send symptomatic staff home? § Identify staff whose duties would allow them to work from home and review/revise telework policies. § What/where are contingency plans for reduced staffing? § Will your facility offer revised duties to staff who are at higher risk of severe illness with COVID-19? YES NO § What mechanisms are in place to remind staff to stay at home if they are sick? § When will you institute employee screening of all employees (see Element #5) (even if you are not in a community with sustained community transmission)? § Review and incorporate into your plans the criteria for staff to return to work with COVID19 symptoms: § Review guidelines regarding COVID-19 Exposures/Quarantine. What is the policy in your facility regarding staff related to self-quarantine vs continue working with face mask? Page 27 COVID-19 Pandemic Response Plan March 26, 2020 § The plan suggests consider relaxing restrictions on allowing alcohol-based hand sanitizer. In this facility the following categories of staff can carry alcohol-based hand sanitizer: Movement How will movement be minimized within the facility? How will movement be minimized between facilities? Will non-urgent medical visits be postponed? YES NO Will copays for incarcerated persons seeking medical evaluation for respiratory symptoms be waived? YES NO 2. Communication The mechanisms for regular updates (paper/electronic/telephonic) will be as follows: -----Staff: -----Incarcerated persons: -----Families of incarcerated persons: The following staff person(s) are responsible for assuring regular communication with stakeholders: Review recommendations regarding signage in the facility. What signage will be posted in the Page 28 COVID-19 Pandemic Response Plan March 26, 2020 facility and where will it be posted? c. Local Public Health Agency: Contact person(s) for COVID-19: Phone: Email: d. Communicate with your local health department and discuss guidance on management and COVID-19 testing of persons with respiratory illness. Document date of communication and the plans discussed: __/__/__ e. Local community referral hospital: ______________________________________ Contact person(s) for COVID-19: Phone: Email: 3. General Prevention Measures a. Good Health Habits: How will good health habits be promoted with your staff (e.g., posters, leadership emphasizing hand hygiene, email messages to staff)? 1) Are there facilities for employees and visitors to wash hands when entering and leaving the facility? YES NO If no, what are plans to address this issue? 2) Are there facilities for incarcerated individuals to wash hands at intake? YES NO no, what are plans to address this issue? If Page 29 COVID-19 Pandemic Response Plan March 26, 2020 3) Are soap dispensers or hand soap available in all employee and incarcerated person restrooms? YES NO What is the plan to assure that soap dispensers are refilled regularly? 4) What is the plan to assure incarcerated individuals have an adequate supply of bar soap? 5) Is signage for hand hygiene and cough etiquette at entry, in public and visible areas around? 6) Are tissues available? YES NO If so, where? 7) Are no-touch trash receptacles available? YES NO If so, where? b. Environmental Cleaning: Review updated CDC recommendations regarding environmental cleaning – noting that common EPA-registered household disinfectants are considered effective? What disinfectants will you use in your facility? (If deemed necessary) purchase EPA hospital-grade disinfectants from Schedule N: https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2. (Recommended products are both a surface cleaner and disinfectant with a 3-minute wet time or less.) Identify “high-touch” surfaces in this facility (i.e., doorknobs, keys, telephones): The following plan will be implemented to increase frequency and the extent of cleaning and disinfection of high-touch surfaces in this facility: c. Social Distancing Measures: What administrative measures is your facility going to institute to increase social distancing within your facility (Review across all departments in the facility)? REVIEW additional suggested measures in the plan. It is recommended that an interdepartmental group review the list and brainstorm what would work In your facility. Then add those agreed upon to the list below. 1) Measure… Page 30 COVID-19 Pandemic Response Plan March 26, 2020 The following new activities will be implemented for incarcerated persons while they are confined to a housing unit: d. Employees Stay Home When Sick: Does communication with employees include message that they should stay home when sick or under quarantine? YES NO Sick employees should be advised to follow CDC guidance on What to do if you are sick? e. Flu Vaccine: Is there flu vaccine in stock? YES NO If yes, number of doses? If yes, what plans are there to continue offering vaccination to employees who have not been vaccinated? If yes, what plans are there to continue offering vaccination to incarcerated persons who have not been vaccinated? f. Review and implement infection prevention and control guidance for staff screening visitors, staff, and new intakes. How will these be implemented? 4. Visitors / Volunteers / Contractors / Lawyers What changes in procedures / polices are being instituted in response to COVID-19 for: a. Visitors: b. Volunteers: c. Non-Essential Contractors: d. Lawyers: Page 31 COVID-19 Pandemic Response Plan March 26, 2020 What signage/communication is being used to communicate with visitors? Is screening for visitors for symptoms and temperature being implemented? YES NO If yes, who will be conducting this screening? 5. Employee Screening Is sustained community-transmission occurring in your community? YES NO If yes, screening of employees upon arrival to work is recommended. Do you have an infrared no-touch thermometer for this purpose? YES NO If no, what are your plans for acquiring them? What are your plans for employee screening? The following system will be utilized for employees to report illness/exposures and to track this information: 6. New Intake Screening It is recommended that new arrivals be isolated from rest of population until screening is performed. New intakes should be screened with temperature and questionnaire. Where will screening occur? Who will conduct screening? What other screening logistics are being considered? Page 32 COVID-19 Pandemic Response Plan March 26, 2020 7. Initial Management and Testing of Cases of Respiratory Illness It is recommended that individuals with symptoms be immediately issued a face mask and be placed in a separate room with a toilet and sink. What separate room will be used for this purpose? Do you have capacity in this facility to perform rapid flu tests? YES NO If yes, what are plans to assure competency in nasopharyngeal swabbing? What are current recommendations from your local health department regarding COVID-19 testing? Review CDC recommendation for clinical specimens? Do you have needed supplies for testing? YES NO If no, what are your plans to obtain them? 8. Personal Protective Equipment and Other Supplies Date: __ /__/__ What is the current inventory of the following PPE: Face Masks: N-95 respirators: Gowns (disposable): Gowns (washable): Eye Protection- Goggles: Eye Protection—Disposable face shields: What is your plan for securing and maintaining an adequate supply of PPE? Page 33 COVID-19 Pandemic Response Plan March 26, 2020 If respirators are available what activities will they be prioritized for? What is your plan for fit-testing correctional officers? What is your plan for fit-testing health care workers? What are your plans for training regarding donning & doffing of PPE? Correctional Officers? Who? When? Health Care Workers? Review Table 3. COVID-19 Personal Protective Equipment Recommendations. What are your plans for posting this chart throughout the facility? 4. Review supply list in plan and determine current stock. What are your strategies for acquiring more supplies during this time of shortage? o Standard medical supplies for daily clinic needs o Tissues o Liquid soap o Bar soap o Hand drying supplies o Alcohol-based hand sanitizer containing at least 60% alcohol (where permissible based on security restrictions) o Cleaning supplies, including EPA-registered disinfectants effective against the virus that causes COVID-19 o Sterile viral transport media and sterile swabs to collect nasopharyngeal specimens if COVID-19 testing is indicated 9. Transport What categories of staff will be responsible for transport of ill persons? Page 34 COVID-19 Pandemic Response Plan March 26, 2020 What is your plan for training transport officers on procedures for transport? 10. Isolation / Cohorting (Symptomatic Persons) Review CDC guidelines regarding the order of preference of rooms for isolating inmates. Are there any changes to your responses below based upon this? (On right-hand ribbon go to “Management” and scroll down to “Medical Isolation…” What is your capacity for isolating ill inmates in single rooms with a toilet? Detail available rooms: What is your capacity for cohorting inmates together in a room with toilets/sinks? Detail available rooms or unit: What is your plan for designating and training officers assigned to isolation rooms on isolation room procedures? Is it feasible to designate specific custody staff to only monitor isolated individual to minimize exposures? YES NO If yes, how will staff be selected for this duty? Review recommendations for laundry and food service items? What are your plans for educating staff and incarcerated workers regarding these recommendations? Review recommendations for cleaning spaces where COVID-19 cases spent time. What are your plans for training staff and incarcerated workers regarding these recommendations? 11. Care for the Sick Do you have an adequate supply of Tylenol and other medications for supportive care of a respiratory illness? How will you identify if ill persons have risk factors for COVID-19 complications who are in need of closer monitoring? What plan will you have for monitoring ill inmates? Page 35 COVID-19 Pandemic Response Plan March 26, 2020 12. Quarantine Review CDC guidelines regarding the order of preference of rooms for isolating inmates. Are there any changes to your responses below based upon this? (On right-hand ribbon go to “Management” and look for “Quadrating Close Contacts…” What rooms could be used for individual quarantine? What rooms could be used for charted (group quarantine)? How do you plan to monitor persons under quarantine? What is your plan for supplying face masks needed for an entire housing unit of incarcerated persons for a period of 14 days? What is you plan/ability to provide single rooms for exposed persons who have risks for complications, e.g., over age 60 or with medical risk factors? Note that the BLUE Quarantine sign has been changed. Destroy these signs if you have printed them and print the RED Quarantine sign (which includes wearing gowns if close contact with quarantined persons). 12. Data Collection, Analysis, and Reporting What is your plan for ongoing collection of data on staff and incarcerated persons with suspected/confirmed for COVID-19 or history of exposure? Who is responsible for data collection, and analysis? This person should be prepared to updated numbers at each of the regularly schedule planning meetings. 14. Summary, Evaluation and Continuous Quality Improvement (CQI) Who is responsible for ongoing evaluation of the pandemic response? How will these evaluations be incorporated into local planning meetings? Page 36 COVID-19 Pandemic Response Plan March 26, 2020 Attachment 1a. COVID-19 Visitor Screening Form (revised 3/25/20) § § § It is suggested that this be form be laminated. Upon arrival to the facility that visitors are be asked to respond verbally to these questions and a temperature taken. Screening can be conducted by any staff person. If an answer to one of the questions is YES or a temperature exceeds 100.4 then hand the ask the visitor to leave immediately. Advise them to communicate with their doctor by telephone. YES NO In the past 14 days, have you had contact with a person known to be infected with COVID-19 (corona virus)? Today or in the past 24 hours, have you had any of the following symptoms? YES Fever, felt feverish, or had chills? NO YES Cough? NO YES Difficulty Breathing? NO Temperature Page 37 COVID-19 Pandemic Response Plan March 26, 2020 Attachment 1b. COVID-19 Employee Screening Form (revised 3/25/20) § § § § It is suggested that this be form be laminated. Upon arrival to the facility the employees are be asked to respond verbally to these questions and a temperature taken. Screening can be conducted by any staff person. If an answer to one of the questions is YES or a temperature exceeds 100.4 then hand the employee a mask to wear and send them home and recommend that they call their supervisor and consult their doctor. A written copy of this form is only required for employees that answer YES to any of the screening questions or have a temperature exceeding 100.4. YES NO In the past 14 days, have you had contact with a person known to be infected with COVID-19 (corona virus)? Today or in the past 24 hours, have you had any of the following symptoms? YES Fever, felt feverish, or had chills? NO YES Cough? NO YES Difficulty Breathing? NO Temperature Screening Date: ____/____/_____ Employee Name (Last/First): _____________________________ Phone Number: ____________________________ Screening Employee Name: __________________ Signature:________________ Page 38 COVID-19 Pandemic Response Plan March 26, 2020 Attachment 2. COVID-19 New Intake Screening Form (revised 3/25/20) 1. Assess the Risk Of Exposure Have you…… In the past 14 days, have you had contact with a person known to be infected with COVID-19 (corona virus) ? Yes No 2. Assess for Signs or Symptoms of Illness • Persons with symptoms of illness or cough should be masked immediately and separated from others. Date of Onset: Do you have a…….. Yes No Fever, felt feverish, or had chills? Record temperature: Yes No Cough? Yes No Difficulty Breathing? 3. If YES SYMPTOM questions, place mask on person and have them perform hand hygiene and evaluate in accordance with instructions in Element 7. 4. If YES to ANY RISK questions, but NO, to all SIGNS or SYMPTOMS, place person in QUARANTINE. Inmate Name: _________________________________ Number: _____________________ Employee Name: ____________________________________ Date: ___/___/___ Employee Signature: ____________________________________________ Page 39 COVID-19 Pandemic Response Plan March 26, 2020 Attachment 3. Respiratory Infection Isolation Room Sign On the following page is a Respiratory Infection Isolation Room sign for posting on the doors of isolation units. Page 40 COVID-19 Pandemic Response Plan March 26, 2020 Page 41 COVID-19 Pandemic Response Plan March 26, 2020 Attachment 4. Quarantine Room Sign On the following page is a Quarantine Room Sign for posting on the doors of housing units being used for quarantine. Note that this sign was modified in the March 25, 2020 version of this document to include use of gown when in close contact with a person in quarantine, i.e., medical personnel taking temperatures. Page 42 COVID-19 Pandemic Response Plan March 26, 2020 Page 43