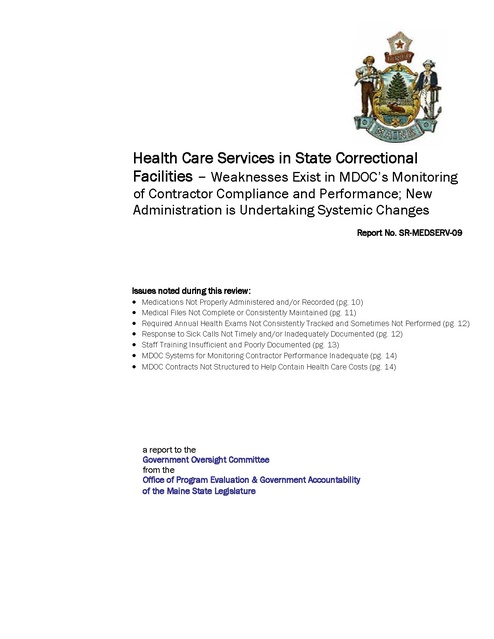
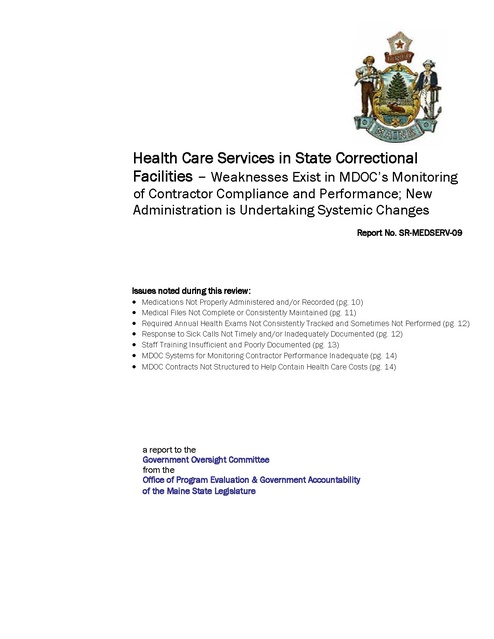
Gao Maine Doc Prison Health Care Services Violations Report 2012
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
FINAL REPORT Health Care Services in State Correctional Facilities – Weaknesses Exist in MDOC’s Monitoring of Contractor Compliance and Performance; New Administration is Undertaking Systemic Changes Report No. SR-MEDSERV-09 Issues noted during this review: • Medications Not Properly Administered and/or Recorded (pg. 10) • Medical Files Not Complete or Consistently Maintained (pg. 11) • Required Annual Health Exams Not Consistently Tracked and Sometimes Not Performed (pg. 12) • Response to Sick Calls Not Timely and/or Inadequately Documented (pg. 12) • Staff Training Insufficient and Poorly Documented (pg. 13) • MDOC Systems for Monitoring Contractor Performance Inadequate (pg. 14) • MDOC Contracts Not Structured to Help Contain Health Care Costs (pg. 14) a report to the Government Oversight Committee from the Office of Program Evaluation & Government Accountability of the Maine State Legislature November 2011 GOVERNMENT OVERSIGHT COMMITTEE OF THE 125TH LEGISLATURE Senator Roger J. Katz, Chair Senator Margaret M. Craven Senator Bill Diamond Senator Earle L. McCormick Senator Nancy B. Sullivan Senator A. David Trahan Representative David C. Burns, Chair Representative Andrea M. Boland Representative Joyce A. Fitzpatrick Representative Leslie T. Fossel Representative Stephen D. Lovejoy Representative Donald E. Pilon OFFICE OF PROGRAM EVALUATION & GOVERNMENT ACCOUNTABILITY Director Beth Ashcroft, CIA Staff Jennifer Henderson, Principal Analyst Wendy Cherubini, Senior Analyst Scott Farwell, Analyst Matthew Kruk, Analyst Maura Pillsbury, Analyst Etta Connors, Administrative Secretary Mailing Address: 82 State House Station Augusta, Maine 04333-0082 Phone: (207) 287-1901 Fax: (207) 287-1906 Web: http://www.maine.gov/legis/opega/ Email: etta.connors@legislature.maine.gov ABOUT OPEGA & THE GOVERNMENT OVERSIGHT COMMITTEE The Office of Program Evaluation and Government Accountability (OPEGA) was created by statute in 2003 to assist the Legislature in its oversight role by providing independent reviews of the agencies and programs of State Government. The Office began operation in January 2005. Oversight is an essential function because legislators need to know if current laws and appropriations are achieving intended results. OPEGA is an independent staff unit overseen by the bipartisan joint legislative Government Oversight Committee (GOC). OPEGA’s reviews are performed at the direction of the GOC. Independence, sufficient resources and the authorities granted to OPEGA and the GOC by the enacting statute are critical to OPEGA’s ability to fully evaluate the efficiency and effectiveness of Maine government. Requests for OPEGA reviews are considered by the Governor Oversight Committee in accordance with a standard process. Requests must be made in writing and must be initiated or sponsored by a legislator. Individual legislators or citizens should review the process and FAQ that are posted on OPEGA’s website at http://www.maine.gov/legis/opega/ProcessProducts.html. There is also a form there to help facilitate the GOC’s consideration of the request. Legislative committees can request reviews directly through a written communication to the Government Oversight Committee. Copies of OPEGA’s reports are free. Reports are available in electronic format at: http://www.maine.gov/legis/opega/ Hard copies of reports may be obtained by contacting OPEGA at: (207) 287-1901 Office of Program Evaluation & Government Accountability 82 State House Station • Augusta, ME • 04333-0082 Health Care Services in State Correctional Facilities Table of Contents――――――――――――――――――――――――――――― Introduction Questions, Answers and Issues In Summary Standards for Correctional Health Care Challenges in Correctional Health Care Administration National Standards for Correctional Health Care Incorporating Standards into the Health Delivery System MDOC’s Delivery of Health Care Services General Background MDOC’s Current Contract for Health Care Services MDOC’s Current Contract for Pharmaceutical Services Issues Noted by OPEGA’s Correctional Health Care Consultant Medications Not Properly Administered and/or Recorded Medical Files Not Complete or Consistently Maintained Required Annual Health Exams Not Consistently Tracked and Sometimes Not Performed Response to Sick Calls Not Timely and/or Inadequately Documented Staff Training Insufficient and Poorly Documented MDOC Systems for Monitoring Contractor Performance Inadequate Contracts Not Structured to Help Contain Health Care Costs Recent Changes in MDOC’s Health Care Administration Changes in MDOC’s Organizational Structure Changes in Philosophy on Services Provided Recommendations Agency Response Acknowledgements Appendix A. Scope and Methods Appendix B. OPEGA Information Brief – Heath Care Services in State Correctional Facilities: Opportunities to Contain Costs and Achieve Efficiencies 1 2 3 4 4 5 5 6 6 8 9 10 10 11 12 12 13 14 14 15 15 17 18 23 25 26 Health Care Services in State Correctional Facilities Health Care Services in State Correctional Facilities Health Care Services in State Correctional Facilities – Weaknesses Exist in MDOC’s Monitoring of Contractor Compliance and Performance; New Administration is Undertaking Systemic Changes Introduction ――――――――――――――――――――――――――――――――― The Maine Legislature’s Office of Program Evaluation and Government Accountability (OPEGA) has completed a review of Health Care Services in State Correctional Facilities. This review was performed at the direction of the Government Oversight Committee for the 124th Legislature. OPEGA contracted with an expert consultant, MGT of America, Inc. (MGT), to conduct most of the fieldwork for this review. This review was focused on health care services delivered by MDOC’s primary contractors, CMS and CorrectRX. OPEGA contracted with an expert consultant, MGT, to conduct the fieldwork. MDOC’s administration of prisoner health care services has been in a state of continuous change over the course of this review. This report reflects issues drawn from audit work conducted in fall 2010, relevant actions taken by the new administration, and recommendations for ongoing improvements. The review’s scope was limited to the adult and juvenile correctional facilities operated by the Maine Department of Corrections (MDOC). It was also specifically focused on the health care services delivered to prisoners by the private correctional care providers Correctional Medical Services (CMS) 1 and CorrectRx. Contracts with these providers represent most of the health care dollars spent on State prisoners, all of which are supported by the State’s General Fund. MGT conducted its fieldwork from September through November 2010 and began sharing its preliminary issues and recommendations with OPEGA and MDOC in January 2011. Subsequently, OPEGA discussed issues raised by MGT with MDOC management and performed some additional document review in the course of finalizing the issues and recommendations for this report. See Appendix A for complete scope and methods. MDOC’s administration of health services for prisoners has been in a state of continuous change since OPEGA began this review in the summer of 2010 and continues to undergo changes as this report is being published. When the review was initiated, the MDOC position of Health Care Services Director was vacant. The position is responsible for administration and oversight of health care services and was filled just prior to MGT beginning the fieldwork. In January 2011, while OPEGA was just beginning discussions with MDOC about reportable issues and corrective actions, a new Governor assumed office. A new MDOC Commissioner was appointed and started in the position in late February and the staff in other administrative positions directly related to managing health care services began to change as well. As a result, OPEGA put this project on hold during the spring of 2011 to allow time for the new management of MDOC to familiarize themselves with the Department’s functions, review the MGT findings, and form their own conclusions about the state of health care services in MDOC facilities. This report now reflects issues drawn from MGT’s point in time look at the Department’s health care services for prisoners during the fall of 2010, the relevant actions that have been taken to date by the new administration, and OPEGA’s recommendations for ongoing improvements. Correctional Medical Services has recently undergone organizational changes and now is know as Corizon. 1 Office of Program Evaluation & Government Accountability page 1 Health Care Services in State Correctional Facilities Questions, Answers and Issues ――――――――――――――――――――― 1. How well does the Maine Department of Corrections (MDOC) manage its contracts for medical, dental, pharmaceutical, and adult mental health services to ensure compliance with contract terms, conditions and expectations with regard to performance, quality and cost? see page 6 for more on this point The burden of delivering quality health care services to prisoners in a manner consistent with professional standards is the responsibility of the vendors that the State contracts to provide these services. MDOC sets the standards of care to be met by the contractors, both through contract language and through the policies and procedures established for health care delivery. OPEGA’s correctional health care consultant, MGT, found the terms of the contracts in effect in fall 2010 did adequately address the most critical areas of prisoner health care services. However, ensuring contractors meet the standards set by the Department requires effective contract monitoring systems as well as strong systems for developing and communicating policy. MDOC’s efforts in this area were not always adequate to ensure that expected standards of care were met. The weakness in monitoring appears to be due to the close and cooperative relationship that has existed between MDOC and its contractors, particularly its primary health care vendor, CMS. This type of partnership has advantages, but also carries significant risk when it interferes with the arms-length monitoring needed to ensure accountability and protect service quality. 2. How well are the selected contractors complying with the contract terms and provisions, relevant regulations and accepted practices that are most critical in delivering health care services to prisoners? see page 10 for more on this point Most of MDOC’s facilities have been accredited by the American Correctional Association (ACA) which, in terms of health care, means that service levels meet the basic performance standards established in the profession. Nonetheless, MGT found that CMS did not always comply with contract provisions requiring adherence to MDOC policies – even in the accredited facilities. Adherence to professional standards for medical care was also lacking in some areas. MGT observed that some prisoners did not receive standard medical services, such as physicals, dental services or sick call response within the timeframe required by MDOC’s contracts. Persistent issues with proper administration of prescribed medications were also noted. A new administration is now managing the Maine Department of Corrections and a Request For Proposal will soon be issued soliciting bids for the provision of all correctional health care services in State facilities. This is an opportune time to establish better mechanisms for monitoring contractors and holding them accountable for compliance with their contract provisions. Such efforts will help ensure prisoners receive appropriate and timely health care services. Office of Program Evaluation & Government Accountability page 2 Health Care Services in State Correctional Facilities The following issues were identified during the course of this review. See pages 18 - 22 for further discussion and OPEGA’s recommendations. • • • • • • • Medications Not Properly Administered and/or Recorded Medical Files Not Complete or Consistently Maintained Required Annual Health Exams Not Consistently Tracked and Sometimes Not Performed Response to Sick Calls Not Timely and/or Inadequately Documented Staff Training Insufficient and Poorly Documented MDOC Systems for Monitoring Contractor Performance Inadequate MDOC Contracts Not Structured to Help Contain Health Care Costs In Summary――――――――――――――――――――――――――――――――――――― MDOC and its health services contractors generally provide adequate prisoner care. However, some deficiencies in contractor compliance with MDOC policies and adherence to professional standards were noted. MDOC has not had a strong system for monitoring contractor performance and has not held contractors accountable for resolving issues identified. The longterm, cooperative relationship between MDOC and its contractors appears to be a contributing factor. MDOC has contracted with its major health care services provider, CMS, for nine years and with its pharmacy provider, CorrectRX, for five years. The terms and conditions of those contracts, including requirements to adhere to MDOC policies and procedures, are key mechanisms for ensuring adequate care for prisoners. While MDOC and its contractors generally provide more than adequate care to the prisoner population, deficiencies in contractor compliance with MDOC health care policies and adherence to professional standards were noted. Some of these deficiencies appeared to be persistent, with clear implications for the adequacy and timeliness of services provided to prisoners. Examples include issues related to medication administration and response to prisoner sick calls. MDOC has not had a strong and effective system for monitoring contractor performance and compliance, or held the contractor sufficiently accountable for resolving issues when they were identified. The long-term relationship between MDOC and its contractors appears to be a contributing factor as the delivery of health care has become more of a partnership than an arms-length arrangement. The facilities appear to be staffed with committed health care professionals and a good working relationship exists between MDOC and CMS, particularly at the clinical level. However, this working relationship needs to be tempered with an appropriate commitment to critical assessment of vendor performance, holding the vendor accountable, and improving the cost-effectiveness of the current contractual relationship. MDOC had begun planning a new RFP for health care services when fieldwork on this review commenced in the fall of 2010. OPEGA’s consultant, MGT, suggested approaches to be used in the RFP and the eventual design of the contractual relationship to help reduce correctional health care costs and maintain or improve quality. MGT shared these suggestions with MDOC, and OPEGA reported on these opportunities to the Legislature in an Information Brief earlier this year. (See Appendix B). During the course of OPEGA discussions with MDOC on the performance issues identified by MGT, there was a transition to a new administration. The new MDOC administration subsequently began taking significant actions impacting the Department’s relationship with its contractors and the health care services Office of Program Evaluation & Government Accountability page 3 An RFP for health care services will soon be issued and MDOC’s new administration seems to be taking positive steps toward improvements in the quality and cost of prisoner health care. Health Care Services in State Correctional Facilities delivered to prisoners. The completed and planned actions, as described to OPEGA, are positive steps and the Department currently appears to have substantial momentum directed toward change and improvement. As expressed in our recommendations, OPEGA considers continuation of those efforts critical to addressing the root causes of issues identified by OPEGA’s consultant MGT. Standards for Correctional Health Care ―――――――――――――――――― Challenges in Correctional Health Care Administration Prisoners have legal rights to receive adequate and timely care. The prisoner population tends to have special issues that make delivery of health services in a correctional setting more challenging than in a community setting. Understanding how correctional health care administration has evolved in the United States provides necessary context for evaluating how health care services are managed by MDOC. The legal rights of prisoners in the United States to receive adequate and timely medical treatment are well established. In 1976, the U.S. Supreme Court in Estelle v. Gamble established that health care for prisoners is a right embodied in the eighth amendment of the U.S. Constitution, affirming that prisoners have a right to be free of deliberate indifference to their health care needs. Since the mid-70’s corrections agencies have implemented policies and procedures to meet this legal requirement. Issues with the delivery of health services in a correctional setting differ somewhat from those of the community. Assuring adequate health care to prisoners requires ongoing attention to a number of special issues, including the following: • Many prisoners have little or no history of good preventive medical or dental care. • High-risk lifestyles lead to the early on-set of medical conditions, often rising to the level of chronic care needs (medical care which addresses preexisting or long term illness, as opposed to acute care which is concerned with short term or severe illness of brief duration). • A large portion of the prisoner population suffers from serious diseases. • Many prisoners express dissatisfaction in types of medications being prescribed and often seek narcotic-level pain medications because of their history with substance abuse. • Many prisoners are reluctant to cooperate in their own health care treatment plans. • Prisoners often have a history of self-mutilating behavior, aggression and violence toward others, lack of education, need for power and control, poor work history, and other anti-social characteristics. • The social disposition of some prisoners creates reluctance to have trust in medical caregivers. • Prisoners can benefit from patient education, but are often not likely to comply with the direction provided. • Establishing a continuum of patient care to follow prisoners upon their release is challenging. Office of Program Evaluation & Government Accountability page 4 Health Care Services in State Correctional Facilities National Standards for Correctional Health Care Policies and standards established by ACA and NCCHC provide national benchmarks and guidance for the practice of correctional health care. The level of care available to prisoners should generally mirror what is available to citizens in their local community. The challenge of delivering adequate health care to prisoners in compliance with legal requirements has led to the development of comprehensive standards and policies to assist correctional administrators. Organizations such as the American Correctional Association (ACA), the National Commission on Correctional Health Care (NCCHC), the American Medical Association (AMA), and the American Public Health Association (APHA) all have made substantial contributions to the development of these standards. As a result of these efforts, the basic principles of correctional health care management are well-established and are a significant component of most state and local correctional systems. Policies and standards established by the ACA and the NCCHC provide national benchmarks for the effective operation of correctional health care throughout the United States. These standards address clinical issues, treatment protocols, administrative controls, staff training and development, disease prevention, quality assurance, safety and emergency procedures, data management, sanitation, and other key issues, reflecting the professional consensus on best practices in all of these areas. Throughout this report, references to best practices and current care standards relate to the specific standards established by ACA and NCCHC to guide the actual practice of correctional health care. The basic guideline for the level of services provided has been, “the community standard of care,” meaning that the level of care available to prisoners in the prison system should generally mirror the level of service available to citizens in their local community. Providing the range of comprehensive medical services available in the community to prisoners in a correctional setting can be challenging. However, it is the State’s responsibility to ensure prisoners have appropriate access to care, consistent with the best use of available resources. Incorporating Standards into the Health Care Delivery System Health care performance standards are established in each correctional system through agencyspecific policies and specific provisions in contracts with helath care providers. ACA has an accreditation system that verifies compliance with the national ACA standards. One outcome of the significant effort to improve correctional health care management over the last thirty years has been substantially increased expenditures for these services, particularly as the prisoner population has grown. In order to better control these costs and gain access to expertise, many state and local correctional systems have privatized correctional health care service delivery by contracting with vendors and non-correctional agencies that specialize in delivering correctional health care services. There are a number of different approaches to privatization, but many systems have adopted a model where the vendor or outside agency provides on-site health care staff in the prison system, and supervises access to and delivery of services both on-site, and, where necessary, off-site in the community. MDOC has adopted this approach. Correctional systems establish performance standards for both vendors and overall system performance through the use of agency-specific health care policies that reflect desired levels of performance, combined with effective contract monitoring. The ACA maintains an accreditation system that verifies correctional agencies’ and facilities’ compliance with the national standards promulgated by the ACA. Accreditation is achieved through a series of reviews, evaluations, audits and hearings. Office of Program Evaluation & Government Accountability page 5 Health Care Services in State Correctional Facilities MDOC’s Delivery of Health Care Services ――――――――――――――― General Background Health care services are provided at each of MDOC’s facilities, mostly through contracts with third party providers. The Maine Department of Corrections (MDOC) operates seven adult and two juvenile penal institutions that housed more than 2,300 prisoners as of December 2010. MDOC is required to provide medically necessary health care to these prisoners. MDOC provides medical, dental, pharmaceutical, substance abuse, and mental health services, including psychiatry and mental health counseling, in both its adult and juvenile facilities. Each facility offers some health care services. When a facility is not able to provide the level of care a prisoner requires, the prisoner may be transported to another correctional facility or off-site health care facility to receive the necessary care. Table 1. Summary of Health Care Services, Providers and Population by Correctional Facility- 2010 ADULT FACILITIES AVG. POP. 2010 DENTAL CMS CMS Psychiatry - CMS CorrectRx 53 CMS CMS Psychiatry - CMS M.H. Counseling - CMS CorrectRx 136 CMS / MDOC CMS Psychiatry - CMS M.H. Counseling - CMS CorrectRx 147 Maine Correctional Center CMS CMS Psychiatry - CMS M.H. Counseling - CMS and MDOC CorrectRx 716 Maine State Prison and Bolduc Correctional Facility CMS / MDOC CMS Psychiatry - CMS M.H. Counseling - CMS and MDOC CorrectRx 987 CMS CMS Psychiatry - CMS M.H. Counseling - CMS CorrectRx 28 MEDICAL DENTAL Long Creek Youth Development Center CMS/ MDOC CMS Mountain View Youth Development Center CMS CMS Central Maine Pre-Release Center Charleston Correctional Facility Downeast Correctional Facility Women's Reentry Center JUVENILE FACILITIES MENTAL HEALTH PHARMACY SERVICES MEDICAL MENTAL HEALTH Psychiatry - Stroudwater Assoc. M.H. Counseling - Youth Alternatives, Ingraham, MDOC, DHHS Psychiatry - Acadia Hospital M.H. Counseling - The Charlotte White Center, MDOC, DHHS PHARMACY SERVICES AVG. POP. 2010 CorrectRx 114 CorrectRx 81 CMS = Correctional Medical Services; MDOC = Department of Corrections; DHHS = Department of Health and Human Services Source: Information provided by the Maine Department of Corrections. Although a few State employees still participate in the delivery of health care services, most services are provided through contracts with third parties as shown in Table 1. Since 2003, MDOC has contracted with Correctional Medical Services (CMS) to deliver medical, dental, and mental health care services and to administer its health care program. Since 2007, MDOC has also contracted with CorrectRx to provide pharmaceutical services in support of its health care program. MDOC is poised to issue a new Request for Proposals (RFP) for all health services provided in the correctional facilities, and intends to enter into new contracts for these services in the first half of 2012. Office of Program Evaluation & Government Accountability page 6 Health Care Services in State Correctional Facilities At the time of this review, both the CMS and the CorrectRx contracts were managed by the MDOC Health Care Services Director and a new person had just been hired into this position. The Department used a variety of methods to monitor the quality of health care and pharmacy services provided by these vendors, including management meetings, monthly reports, and periodic MDOC and CMS audits. MDOC held yearly meetings with CMS to define expectations, bimonthly management meetings to discuss system-wide issues, monthly Medical Audit Committee (MAC) meetings at Maine State Prison (MSP) and Maine Correctional Center (MCC), and quarterly MAC meetings at the other MDOC facilities. Figure 1 displays the MDOC’s management structure over the delivery of health care services in its facilities as of December 2010. Figure 1. Maine Department of Corrections Organizational Chart for Delivery of Health Care Services as of December 2010 --- -- -----I~- -I "'"'''':::;~ ,- - _ . ~- -- -. -- =..~OO' ,- . -- ,------------, , ~, ~-• _ ~ -, --- -~- • "", _ _ _ ",0 ------------- .~ -I :.--; I ,! .:f!:. , -. r -.-":-,,, r-_. ... ~-l~r-"---f ... ......- "' --. _. --, -I ---I ..-,, , --:r--•• :r--,, - ~- • ~ I • ~-., --", I I~'" . ~_.~ f ."O~""I ~_. ~ , , """",co-o --", 0 0 0 • , :r--- -I 0 0 L ______________ L _______________ Office of Program Evaluation & Government Accountability • • 1 ,, ,, ~ • "' "' _______ _ ..._p, I'~- I""""'='-"' page 7 Health Care Services in State Correctional Facilities MDOC’s health care policies and operating procedures follow ACA standards. All but two MDOC facilities have qualified for full ACA accreditation. Though physical plant issues prevent MDOC from seeking accreditation for those two facilities, the Department is confident that ACA medical standards are being met there as well. MDOC’s health care policies Acronyms for MDOC Facilities and operating procedures BCF - Bolduc Correctional Facility generally follow ACA CMPRC - Central Maine Pre-Release Center standards. Both of MDOC’s CFF - Charleston Correctional Facility juvenile facilities (MVYDC DCF - Downeast Correctional Facility and LCYDC) and four of the MCC - Maine Correctional Center MSP - Maine State Prison adult facilities (MSP, BCF, WREC - Women's Reentry Center MCC and CCF) currently LCYDC - Long Creek Youth Development Center have ACA accreditation. MVYDC - Mountain View Youth Development Center MCC just passed its reaccreditation audit and the other five facilities are up for reaccreditation in 2012. The Women’s Re-entry Center underwent its first ACA accreditation audit this year, and MDOC recently learned that it will be recommended for accreditation. MDOC has not sought ACA accreditation for the remaining two adult facilities CMPRC and DCF – as they would not meet ACA’s physical plant standards. MDOC reports, however, that the medical departments at both those facilities are held to the same ACA health care standards as the accredited facilities and there are no differences in the policies and procedures or way care is delivered in the nonaccredited facilities. MDOC is confident that all ACA medical standards are being met at CMPRC and DCF. MDOC’s Current Contract for Health Care Services MDOC’s contract with CMS has been amended and renewed multiple times since it was awarded in 2003. The FY2012 amount for the contract is just over $12 million. The contract requires CMS to provide certain services, and manage overall health care delivery for MDOC, in a manner that complies with MDOC policies and medical care standards. Achievement of ACA accreditation is also a contract requirement. For FY 2012 the Department of Corrections’ contract with CMS totaled just over $12 million and was entirely supported by the General Fund. The CMS contract, originally awarded via a RFP process, has been amended 14 times and renewed seven times since 2003. These amendments were related to increases in psychiatric services, population growth, addition of a facility, revised staffing plans, reduction in MaineCare reimbursement rates, and other factors. Critical provisions of the CMS contract include requirements for: • routine medical care; • health examinations upon admission to the prison system; • physical health assessments; • physician, dental and optometry services; • provision of medications and immunizations as prescribed; • emergency medical response; and • specialty and ancillary services. The contract requires CMS to manage health care delivery for MDOC, including negotiating payment rates, administering statewide health care programs, maintaining appropriate staff licensure, providing training, conducting discharge planning, administering medical records and providing overall clinical oversight. In addition, CMS is required to comply with applicable MDOC regulations, policies and medical care standards. Achievement of ACA accreditation is also a requirement in the CMS contract. Office of Program Evaluation & Government Accountability page 8 Health Care Services in State Correctional Facilities CMS’s contract also specifies the number and type of staff the contractor is required to provide at each facility. These contracted staff totaled 98 full time equivalents (FTEs) as of December 2010, but CMS was having persistent difficulties recruiting and retaining staff in some positions. Although the contract is for a specified dollar amount, CMS’s final compensation is determined by the cost of actual staff and services provided, plus administrative costs. MDOC’s Current Contract for Pharmaceutical Services CorrectRX has been contracted to provide pharmaceutical services since 2006. Those services are to be provided in accordance with State and federal standards as well as those of the NCCHC and ACA. CorrectRX is also required to provide regular utilization and monitoring reports and to visit each facility every three months to check that medications are being properly administered. The CorrectRx contract for pharmaceutical services at MDOC facilities was originally awarded via RFP in December, 2006 and has been amended and/or renewed four times since then. The current agreement is for $3,258,000 and can be adjusted up or down if costs exceed or are less than this amount. Under this contract, CorrectRx provides the following services in accordance with State and federal standards as well as those of the National Commission on Correctional Health Care (NCCHC) and American Correctional Association (ACA): • performs all monitoring services expected of a pharmacy including quarterly inspection of medication rooms and carts at all MDOC facilities where needed; • makes available a licensed pharmacist by telephone for consultation; • delivers all prescriptions and non-prescription medications to each facility in a timely manner; and • works cooperatively with all MDOC facility staff and medical and psychiatric services contractors and subcontractors to ensure timely and appropriate delivery of medications and health care services to all prisoners and residents. CorrectRx also maintains arrangements with community pharmacies located in close proximity to correctional facilities for an emergency backup supply of medications. The contract with MDOC requires CorrectRx to provide a number of regular reports to State administrators. These reports include quarterly utilization data, pharmacy services and facility monitoring reports, and quality assurance reports. In addition, CorrectRx must ensure a registered pharmacist visits each MDOC facility at least every three months to perform the following tasks: • review medication administration records for appropriateness of documentation; • review drugs on site for dating and storage; • ensure that medications are being destroyed appropriately; • provide recommendations as to therapy; and • provide education as needed. Office of Program Evaluation & Government Accountability page 9 Health Care Services in State Correctional Facilities Issues Noted by OPEGA’s Correctional Health Care Consultant ―― OPEGA’s consultant, MGT, identified numerous compliance issues, some of which were challenged by the MDOC health care administrators in place in January 2011. OPEGA was still in discussions with MDOC over these issues when MDOC health care administration began to change. The new administrators are now incorporating actions on all issues MGT identified into larger, systemic changes they are pursuing. The work performed by OPEGA’s consultant, MGT, is described in Appendix A. It included review of the relevant health care services contracts and Departmentwide policies and procedures, as well as interviews and observations at each of the facilities operated by MDOC. In addition, MGT conducted more in-depth review at the two largest adult facilities – Maine Correctional Center (MCC), and Maine State Prison (MSP) – and Long Creek Youth Development Center (LCYDC) which houses the most juveniles 2 . MGT reviewed the facility-specific policies and procedures, prisoner grievance logs, minutes of Medical Audit Committee meetings and other site specific materials at each of the three locations. A sample of 24 prisoner medical files, spread across the three facilities, was also examined to determine compliance with key MDOC health care policies, contract provisions and correctional health care standards. MGT’s sample was judgmentally selected from a list of current prisoners at each facility provided by MDOC. The draft findings and recommendations resulting from MGT’s work generated considerable discussion between OPEGA and the MDOC health care administrators in place in January 2011. MDOC agreed with some of the issues identified and explained challenges they faced that had contributed to those issues. On other issues, however, they challenged whether the exceptions were significant enough to warrant requiring CMS to take corrective action. For example, they felt the sample of medical files MGT reviewed was not large enough to be representative of overall conditions. They planned to conduct their own file review, with a much larger sample, to determine whether the concerns were valid. They also felt some exceptions identified by MGT were isolated incidents or had explanations that negated them. While OPEGA was still in discussions with MDOC, a new commissioner was appointed to the Department who began making changes to staff in other administrative positions directly related to managing health care services. OPEGA subsequently discussed MGT’s results, described below, with MDOC’s new administration. The new administrators are incorporating actions to address these issues into larger, systemic changes they are pursuing in correctional health care. Medications Not Properly Administered and/or Recorded MGT noted exceptions in documentation of medications dispensed for 59% of the prisoner medical files reviewed. MGT reviewed medication administration registers for the month of September 2010 for the sample of 24 prisoners, only 22 of whom were on medication. The results are summarized in Table 2. MGT found that CMS did not maintain files to show prisoners received medications as prescribed in more than half of the cases reviewed. For 11 of the 22 prisoners (50%), there was no evidence in the file that medications were dispensed per doctor’s orders. These prisoners had no entries in the time slots on the medical administration register to indicate whether the Maine State Prison and Maine Correctional Center together house about 78% of the total adult prisoners in the State correctional system. Long Creek Youth Development Center houses about 58% of the total juveniles in the system. 2 Office of Program Evaluation & Government Accountability page 10 Health Care Services in State Correctional Facilities prisoner took his medication, refused his medication, was absent at the pill line, or received the medication. For 2 prisoners (9%), medication administration registers could not be provided by medical staff. Table 2: Results from Testing of Medication Administration Registers at Three MDOC Facilities Files with No Total Number of Number of Files with No Evidence Medication Prisoners Files Prisoners on Medication was Properly Administration Institution Tested Medication Dispensed Percent Registers Percent MCC* 14 12 6 50% 1 5% MSP 7 7 4 57% 0 0% LCYDC 3 3 1 33% 1 33% Total 24 22 11 50% 2 9% *MCC has sections for both male and female prisoners. The sample included files for 11 male and 3 female prisoners. Source: MDOC medical files, as reviewed by MGT of America Inc. Minutes of 2010 meetings between CMS and MDOC, and prisoner grievances, indicate on-going issues with medication administration that should have resulted in corrective action. Minutes of management meetings between CMS and MDOC reflected ongoing concerns during 2010 regarding incorrect medications being given to prisoners, inconsistency with following stop and start dates of prescriptions and other poor practices associated with medication tracking and labeling. Meeting notes indicated that new procedures, better staff training and staff counseling were considered as potential solutions, but did not indicate whether any actions were taken. Several prisoner grievances or complaints related to medication were also filed during fiscal year 2009-10. The issues grieved included medication being distributed late, incorrect dosages, and incorrect medications given. Failing to provide the correct medication within the prescribed time frame is a violation of MDOC policies and accepted best practices. Professional standards call for the correct medication to be delivered to each prisoner in the prescribed amount and at the correct interval as prescribed by the physician. All dispensation of medications should be documented, including refusals to take medication as ordered. Medical Files Not Complete or Consistently Maintained MGT found that 46% of files reviewed did not have all required intake forms completed. Thirty-three percent also had sign-in sheets that were missing or not properly used. MGT found that CMS staff did not consistently follow MDOC policies related to medical intake and medical records. Specifically, CMS staff did not always ensure required intake forms and the required intake checklist were completed and included in prisoners’ files. Of the 24 medical files reviewed, 15 (63%) did not have completed intake checklists and 11 (46%) did not have all the required intake forms completed. Policy also requires that medical files contain an accurate and updated sign-in sheet with clear signatures and initials of employees and practitioners who update the file. The intent is to be able to identify the individuals whose signatures or initials are written in the medical chart. Three of the 24 files reviewed did not include a sign-in sheet at all and another five included a sign-in sheet that was blank or not updated. In some cases, the medical personnel writing to the chart had not signed the log. MGT also noted inconsistent understanding among staff at the facilities as to what the sign-in sheet was for and who should be signing it. Office of Program Evaluation & Government Accountability page 11 Health Care Services in State Correctional Facilities Required Annual Health Exams Not Consistently Tracked and Sometimes Not Performed Thirty-eight percent of files reviewed had inaccurate records for physical exams and 13% did not have any dental intake records at all. MGT found that CMS staff did not always properly document prisoner physical assessments and did not always provide annual physical assessments as required by the MDOC contract. The means of tracking when annual physical assessments were due was inconsistent and manual across facilities, despite the fact that all facilities were managed by CMS. As shown in Table 3, nine of the 24 medical files (38%) MGT reviewed had inaccurate records regarding physical assessments. Three prisoners—one of whom also had inaccurate records regarding physical assessments—had not received all required annual physical assessments. Table 3: Results from Testing of Required Annual Physical Exams at Three MDOC Facilities Total Number Prisoners with Inaccurate Prisoners Who Did Not of Prisoners Files Regarding Physical Receive All Annual Institution Files Tested Assessments Percent Physical Assessments MCC* 14 2 14% 1 MSP 7 6 85% 2 LCYDC 3 1 33% 0 Total 24 9 38% 3 Percent 7% 29% 0% 13% *MCC has sections for both male and female prisoners. The sample included files for 11 male and 3 female prisoners. Source: MDOC medical files, as reviewed by MGT of America Inc. Three of 24 prisoners had not received annual physical exams and two had not received annual dental services. CMS medical staff also failed to ensure dental intake and annual dental assessments were completed, or that documentation of them was included in prisoners’ medical files. Exceptions were noted in five of the 24 (21%) prisoner medical files reviewed. Three of those files (13%) did not have any dental records (and this was not due to the prisoner having been newly incarcerated), and two others (8%) had records indicating the prisoner had not received the annual dental services that appear to be required by MDOC policy. Response to Sick Calls Not Timely and/or Inadequately Documented MGT noted exceptions with response time or documentation for 11% of the 203 sick call slips reviewed. “Sick call” is a critical service provided to prisoners and guaranteed by CRIPA— the Civil Rights of Institutionalized Persons Act. Sick call slips allow a prisoner to alert health care staff of the desire or need for non-emergency medical or dental services. MDOC policy provides for sick call slips to be “readily available” to all prisoners, with medical staff at each facility establishing their own systems to process the sick call slips. Policy further states that “all non-emergency sick call slips shall be reviewed by nursing staff within 24 hours of receipt” and the prisoner shall be “seen by qualified health care staff within the next 24 hours (72 hours on weekends)”. MGT reviewed 203 sick call slips for the 24 prisoners whose medical files were reviewed. MGT found 23 slips, or 11%, that were either not resolved timely or had no resolution date or actions noted in the medical file. MDOC health care management meeting minutes in 2010 indicated the sick call process was too timeconsuming and there were too many sick calls to process in the time allotted for that purpose. MGT noted that this problem was hard for MDOC to quantify because sick call slips are kept in prisoners’ individual files. As a result, there is no easily aggregated data to help understand the amount of time being spent by staff on sick calls, the number of sick call slips being submitted by prisoners, or whether Office of Program Evaluation & Government Accountability page 12 Health Care Services in State Correctional Facilities Minutes of 2010 meetings between CMS and MDOC show concerns about the sick call process and inabilities to handle the high number of sick calls within the time allotted for them. Changes to the sick call process have now been made to address documentation and other issues. specific prisoners are particularly high users of sick call services and could perhaps have their health needs more efficiently met through some other avenue. According to MDOC and CMS staff, during October 2010, a new sick call process was being developed cooperatively between MDOC and CMS to address these issues and provide better care. The new administration has followed through on that effort and also implemented additional improvements. Facility nurses are now required to log the date and time when they examine a prisoner’s sick call slip, as well as the response they determined was appropriate. In the past, prisoners complained days had gone by since they submitted a sick call with no attention to their medical concerns. Nurses claimed the prisoners had been seen within a few hours of their requests and it was determined no further medical attention was required. There should now be a record of nurses’ actions, so although prisoners may still dispute whether the actions were appropriate, there can be no question as to whether the sick call was responded to within the timeframes required by MDOC policy. MDOC also reports having made changes to how the security and medical teams work together to handle sick calls. In September 2011, MDOC reported to OPEGA that the Health Services Coordinator had recently completed an audit of files to ensure CMS was following the new procedures and improving compliance with sick call standards. Staff Training Insufficient and Poorly Documented MGT noted that: • health care staff were not sufficiently knowledgeable of MDOC policies and health care standards; • CMS was having difficulty fulfilling some training requirements; and • training received by staff at MSP was not well documented. CMS’s contract specifically designates the vendor as responsible for providing training programs for all health care staff, whether MDOC or CMS personnel, as well as training for other security and non-security staff as outlined in an annual training plan. This training should cover topics associated with ACA accreditation, since achievement of accreditation is required under the contract and contingent upon staff adhering to ACA guiding principles, rules, and standards. However, MGT noted several conditions indicating that training of MDOC and CMS staff was insufficient. In addition to the failures to maintain proper medical records already discussed, MGT also reported that: • Discussions with medical staff during the fall of 2010 revealed that MDOC and CMS medical staff were not familiar with the full range of correctional health care standards that apply to the system. MGT also noted mixed understanding of MDOC’s agency-wide and facility-specific operating policies. • Minutes of health care management meetings in 2010 recorded staff concerns regarding insufficient training for CMS staff. The minutes also recorded that CMS was having an issue with providing required First Aid and CPR training to all MDOC staff due to the volume of staff to be trained. MGT requested the training files for staff members from each of the three facilities selected for detailed review—MCC, MSP, and LCYDC. The training files were difficult to obtain at MSP, and when found, were poorly organized and difficult to follow, making it a challenge to ascertain whether required trainings had been Office of Program Evaluation & Government Accountability page 13 Health Care Services in State Correctional Facilities delivered. As of December 2010, MDOC acknowledged issues in delivery and documentation of training, but believed all required training was being provided. MDOC Systems for Monitoring Contractor Performance Inadequate MDOC has permitted CMS to monitor and report on its own performance rather than establishing independent systems to ensure CMS meets contract requirements, provides adequate care, and manages costs reasonably. Minutes of meetings between CMS and MDOC also show identified issues being on the agenda month after month in 2010 with no actions or resolution recorded. Although MDOC policy requires an internal system of review, as of fall 2010 the Department was permitting CMS to monitor and report on its own performance. The Department had very little in the way of independent systems to oversee the contractor and ensure CMS was delivering on the contract requirements, providing adequate care to prisoners, and managing costs reasonably. MGT noted it appeared that MDOC and CMS had worked together for so long that their relationship had taken on the tone of a partnership between equals and lost the “arms-length” nature of most contractor-customer relationships. This is exemplified in MDOC’s hesitancy to hold CMS accountable when contract requirements were not fulfilled. In a follow-up discussion regarding this matter in December 2010, MDOC’s Health Care Services Director agreed that better performance management was needed, and stated that actions were already underway to improve in this area. However, she cited the lack of readily available performance and outcome data as complicating efforts to assess contractor performance and enforce accountability. The performance data that was available to MDOC at that time did not appear to be used to inform agency policymaking. Monthly statistical reports include detailed data about the numbers and types of medical services provided to the prisoner population that could have been used for analyzing trends, staff time, and other costs. This data was reviewed at Medical Audit Committee (MAC) meetings and quarterly executive committee meetings, but meeting minutes indicate little emphasis placed upon this data. Furthermore, it is unclear whether any staff member was monitoring the activity noted in the reports and following up as needed. MGT also noted that a number of issues and concerns were discussed in monthly MAC meeting minutes on a repeated basis during 2010. Meeting minutes often indicated the same issues were discussed over and over, with agenda items tabled from month to month, but no final resolution noted. Allowing issues to linger and remain unresolved for months on end, while noting “tabled” repeatedly on meeting agendas or in minutes, is not a productive use of meeting time and does little to address the issues identified. MDOC management, past and present, have explained that MAC meetings did resolve issues, and that they simply failed to document the actions taken. Contracts Not Structured to Help Contain Health Care Costs MDOC’s contracts with CMS and CorrectRx have not been structured or managed to maximize cost savings to the State. MDOC’s use of long-term, open-ended contracts diminishes vendor incentives to continually reduce costs. However, MDOC’s planned re-bidding of this contract is a good opportunity to bring competitive pressures to bear to reduce healthcare costs. As part of its review, MGT suggested approaches that MDOC could incorporate into a new RFP with the goal of better containing costs. OPEGA reported on these suggestions in an Information Brief published April 2011. (See Appendix B). Office of Program Evaluation & Government Accountability page 14 Health Care Services in State Correctional Facilities MDOC’s contracts with CMS and CorrectRX have not been structured to maximize cost savings to the State. In addition, the long-term nature of those contractual relationships has diminished vendor incentives to continually reduce costs. MGT suggested several cost containment strategies that could be incorporated into MDOC’s next RFP and the resulting health care services contract(s). There are two primary cost drivers in the MDOC healthcare contract: off-site treatment costs and staff costs. The key to generating cost efficiencies in management of off-site services is to shift some risk to the vendor, allowing it the opportunity to increase profitability if service costs decrease. If, for example, a vendor is not only responsible for managing off-site hospitalization care, but is also made responsible for the cost of that care, that vendor will have an incentive to aggressively manage cost. As a result of competition, some of these cost savings will be passed along to the State in the form of an overall lower bid for off-site treatment costs. To assure that these cost reductions reflect increased efficiency and not reductions in service levels, active management of the contract and oversight of the vendor by MDOC is necessary. Providing vendors with opportunities to achieve savings through their performance will also increase competition for these contracts, as they become potentially more profitable for more companies. On the staffing side of the contract, the MDOC-specified staffing plan establishes clinical staffing levels that are high relative to those of many other state correctional systems. There are many factors unique to Maine’s correctional system and public health that may account for this. However, allowing vendors to propose alternative staffing plans to meet designated contract service levels could produce more efficient staffing allocations, possibly producing significant medical contract staff savings for the MDOC. Finally consolidation of the pharmacy contract into the healthcare management contract would simplify administrative oversight and would vest financial responsibility for pharmaceuticals with the organization responsible for supervising the prescription of these drugs, significantly improving incentives for cost control. While there has been no independent research into the relative cost impact of different managed care approaches to correctional health care management, the widespread use of the approaches outlined above suggests that states have found them beneficial in controlling costs. Recent Changes in MDOC’s Health Care Administration ―――――― OPEGA met with the Department of Corrections’ new health care services administrative team in September 2011 to again discuss the reportable issues from this review and actions that would be taken to address them. OPEGA learned that significant organizational changes affecting roles and responsibilities for administering health care services contracts are underway. In addition, the prevailing philosophy regarding provision of health services to prisoners and oversight of health services contractors has changed significantly. Changes in MDOC’s Organizational Structure Since January 2011 there have been substantial changes in MDOC’s administrative layer which impact the administrative oversight and monitoring of health care services. The new Commissioner of MDOC appointed a new Associate Commissioner and also made structural changes to the central office positions responsible for health care services contracts and service delivery. Office of Program Evaluation & Government Accountability page 15 Health Care Services in State Correctional Facilities Since January 2011, substantial changes have been made in the MDOC administrative positions responsible for overseeing health care delivery. The changes are intended to streamline communications, improve monitoring of contractors, promote contractor accountability and resolve issues in a timelier manner. The position of Health Care Services Director, which had responsibility for the administration of health care contracts, has been eliminated. The previously existing position of Health Care Services Coordinator continues to serve as the direct liaison between MDOC management and the CMS Health Services Administrators at each correctional facility. That position has been reclassified, however, and now also has direct responsibility, and the requisite authority, for oversight of CMS and CorrectRX performance and compliance with standards and policies, as well as for the resolution of health care issues at each facility. The Coordinator now reports directly to the MDOC Associate Commissioner and is also functionally overseen by MDOC’s Clinical Director. The Clinical Director, who also reports to the Associate Commissioner, heads up the entire clinical area and serves as a bridge between the medical and mental health services being delivered. The employee who has filled the position of Health Care Services Coordinator for the past 3 years described several ways in which she is now empowered to deal with contractor performance issues and health care complaints or grievances. For example, she is now allowed to: • ask questions of the contract staff or investigate complaints and grievances on her own authority; and • communicate directly with MDOC’s Clinical Director, the Corizon (formerly CMS) Regional Medical Director and the CorrectRX Director of Medicaid Management without those communications being funneled through the MDOC Health Care Services Director. She explained that the simplified lines of communication allow health care issues to be resolved in a more coordinated and timely way. She also noted that having the authority to make inquiries and investigations has been beneficial in monitoring the contractors’ performance and increasing accountability. MDOC’s new Associate Commissioner reported that monthly calls are now being held that include herself, the MDOC Commissioner, the Health Care Services Coordinator and the Directors at both CMS and CorrectRX so they can cooperatively discuss MDOC’s expectations and issues that need to be addressed. MDOC is also hiring a Resource Administrator to assist in administration of the new health care services contract(s) by providing financial oversight and supporting the RFP process. The Resource Administrator will report to the Manager of Correctional Operations who reports to the Associate Commissioner. Once the contract is in place, this position will be responsible for monitoring and auditing the financial aspects of the health care delivery contracts, as well as some quality assurance efforts. An example of planned assignments is developing dashboard reports on utilization and complaint data that will allow MDOC to better monitor contractor performance, and identify and respond to emerging issues and trends that affect quality and cost of services provided. MDOC expects that the Health Care Services Coordinator and the Resource Administrator will work closely together in monitoring contractor compliance and performance. Prior to the initiation of this review, another issue related to organizational structure and staffing had come to OPEGA’s attention. OPEGA had received complaints about difficulties arising from contracted health services staff in MDOC facilities working with, and supervising, a small number of remaining State health Office of Program Evaluation & Government Accountability page 16 Health Care Services in State Correctional Facilities care employees. MGT observed this issue in its review as well, and recommended MDOC seek to transition all health care positions to contract staff to avoid the confusing commingling of contract and State employees. MDOC’s new health care administrators also recognized this as a problem and the upcoming RFP will require that the contractor provide all staff. At the time of this report, MDOC was moving to eliminate the remaining State health care positions through attrition. Four State positions, two each at LCYDC and MSP, currently remain and will be phased out by the time the new contract is established. Changes in Philosophy on Services Provided Since June 2011, MDOC has adopted a philosophy of providing only medically necessary care. Goods and over-the-counter medications previously prescribed only to improve prisoner comfort will now have to be purchased by prisoners at facility canteens. Medical procedures will likewise be limited to those deemed medically necessary. The intent is to reduce costs, bring Maine more in line with services provided in other states, and bring efficiencies to administrative and service delivery processes. As MDOC’s new administrative team began reviewing medication and prescribing practices, it learned that Maine had significantly more prescriptions for certain medications and items than other states. They attribute this in part to MDOC’s historical practice of allowing prisoners to receive prescription items or procedures that were “comfort measures” not truly required to treat any medical condition to the acceptable standard of care. New Balance sneakers are an example of comfort goods prisoners had been receiving through prescription. OPEGA had been told, by a source familiar with the health care being provided at one facility, that prisoners who found the standard issue sneakers uncomfortable because of their width frequently succeeded in getting prescriptions for the more expensive New Balance sneakers. MDOC’s review confirmed this practice. Examples of other comfort items provided by prescription include over-the-counter pain killers, such as Tylenol or Advil, and skin creams or baby powder. Since June 2011, MDOC has adopted a new philosophy of providing only necessary medical care. Under MDOC’s new philosophy, prisoners will still have access to many comfort items formerly provided which are over-the-counter in nature (such as skin creams), but will now need to purchase them from facility canteens. The new administrators say covering the cost of care that is not medically necessary is no longer sustainable as MDOC seeks to be increasingly cautious with its General Fund dollars. MDOC reports that each prisoner’s record was reviewed by a medical doctor to assure that prescriptions were continued for any medically necessary items. In addition to reducing costs, MDOC also expects that limiting prescribed items will improve the efficiency in distributing medications to prisoners, i.e. shorten the pill lines, and reduce the administrative burden of related documentation in prisoners’ files. MDOC’s new philosophy will also be applied in determining what medical procedures are provided for prisoners. Knee replacement surgery is an example of a procedure MDOC formerly provided, and paid for, that may no longer be covered unless replacement is necessary for the prisoner to function within the walls of the correctional facility. Otherwise, the prisoner’s treatment will focus on alleviating any discomfort associated with the knee condition. MDOC is currently also re-assessing the medical necessity for prisoner special diets and personal property like mattresses. MDOC recognizes that the new philosophy represents a significant shift from past practice and will likely result in substantial push-back from prisoners, their families, and advocacy groups. However, the Department feels this change will bring Maine’s correctional health care services more in line with other states while still Office of Program Evaluation & Government Accountability page 17 Health Care Services in State Correctional Facilities meeting its obligation to provide appropriate health care to prisoners. The Department has been taking steps to inform relevant stakeholders about the changes, including meeting with the Boards of Nursing and Medicine, having medical providers and administrators present at Town Hall meetings with prisoners, and reaching out to advocacy groups. The Commissioner and Associate Commissioner have also been meeting personally with prisoners on their complaints. Recommendations ――――――――――――――――――――――――――――― 1 MDOC Should Periodically Verify Contractor Compliance with Contract Terms, MDOC Policies and Health Care Standards MDOC has not had sufficient mechanisms for independently determining whether contractors are providing all services and goods specified in the contract at the agreed upon levels of quality and cost. The health care services contractors have regularly provided performance reports and reported issues they have to MDOC, but they have largely monitored themselves as MDOC has accepted this performance information without periodically verifying it. In addition, in a few cases where CMS was clearly not fulfilling its contractual obligations, the Department was reluctant to hold CMS directly accountable by requiring CMS to become compliant or applying financial penalties where the contract allowed for them. Instead, the Department appeared to either accept the contractor’s explanations for the non-compliance, or shared the responsibility for finding solutions to those issues. As previously described in this report, MGT had noted CMS compliance issues in a number of areas including: • medication administration practices and documentation; • sick call procedures; • consistent and appropriate maintenance of medical records; and • provision of required annual health and dental assessments. When these issues were brought to MDOC’s attention in January 2011, the health care services administrators challenged MGT’s evidence on some of the issues because it was not consistent with what CMS had been reporting to them on its own performance. MDOC acknowledged, however, that the Department itself had not been independently auditing prisoner files to determine compliance and, therefore, lacked any independent information on which to judge either CMS’ reports or MGT’s results. The exception was compliance with sick call standards and policies which MDOC and CMS had already identified as an issue. Efforts were already underway to improve the sick call system by introducing new procedures when MGT was conducting its work in the fall of 2010. Additional improvements have also been made by MDOC’s new administration. Office of Program Evaluation & Government Accountability page 18 Health Care Services in State Correctional Facilities Recommended Management Action: MDOC should ensure all contracts for health care services are adequately monitored for compliance with specific contract terms, critical MDOC policies and relevant correctional health care standards. MDOC should implement a formal plan for periodically verifying compliance independent of the contractor and contract staff. Such auditing or testing should be incorporated as a key component of an overall quality assurance process as described in Recommendation 2. MDOC should require the contractor to take corrective action when non-compliance is identified and follow-up to assure the corrective action was effective in correcting non-compliance issues. MDOC should also assess any penalties allowed under the contract. 2 MDOC Should Strengthen Quality Assurance System In addition to the lack of independent compliance monitoring, MGT also found MDOC had a weak overall Quality Assurance (QA) system. MDOC was not setting overall performance measures for health care nor collecting and analyzing data to monitor high risk areas or proactively identify potential concerns. MGT additionally noted that some identified issues seemed to be persistent, with little documentation of actions being taken to address them, indicating MDOC did not have an effective system for resolving issues in a timely way. A well-designed QA system should include ongoing and systematic monitoring and evaluation to detect potential weaknesses and provide for the proactive development of appropriate corrective measures. Key features include: • Identifying the services that are most critical in terms of risk and liability, and that should therefore be closely monitored; • Establishing minimum standards of performance for all critical services; • Collecting the data required to assess whether those minimum standards are being met continuously; • Developing action plans to address identified deficiencies; • Assessing the impact of the actions taken to ensure services have improved to an adequate level. Though MDOC has had little in the way of a formal QA system in place, a variety of potential quality issues have come to the attention of management via staff complaints, prisoner grievances, or through performance data provided by CMS. MDOC has, however, often failed to take adequate action to address the root causes of the issues. They have instead been dealt with on a case-by-case basis, or referred to the Medical Audit Committee where they appeared to be discussed month after month with no documented action or resolution. Office of Program Evaluation & Government Accountability page 19 Health Care Services in State Correctional Facilities Recommended Management Action: MDOC should strengthen its quality assurance plan for health care services, assign responsibility for analyzing monthly statistical reports and identifying trends, and review the types of statistics being gathered to determine if other kinds of information would be of greater use. In addition, responsibility should be assigned for ensuring action plans are developed to address areas of concern identified through the QA process with regular follow up to assure the expected actions were taken. As part of the QA system, MDOC should ensure all health care services contractors are adequately monitored for compliance as described in Recommendation 1. 3 MDOC Should Ensure Staff Involved in Health Care Service Delivery are Sufficiently Trained and Knowledgeable of Relevant Policies and Standards CMS’s contract requires that all medical and non-medical staff are thoroughly trained and understand the content of MDOC’s policies and procedures, as well as the standards of professional care related to health care services. As discussed on page 13, however, MGT noted several indications that CMS may not be ensuring that its staff is sufficiently trained and/or may not be providing all training required under its contract. These indications included: • a lack of documentation to demonstrate CMS had been providing the training as required; • CMS acknowledgement that providing First Aid and CPR Training to all staff, as required, had been an issue; • concern among leaders at facilities visited that CMS staff did not have adequate knowledge of MDOC’s security policies; and • some medical staff being unfamiliar with the language in some policies or having no knowledge of pertinent documents or their purpose. MGT also took issue with MDOC’s process for communicating updates in policy and procedures to medical staff. Hard copies of updated policies are placed into binders and are available in workplace offices. Simply making policies available, however, is not sufficient to assure staff familiarity with facility requirements, and is not consistent with best practices. Medical services staff should receive training on updated policies and should have a clear understanding of the rationale behind policy requirements and how the policy language translates to procedures at each facility. Recommended Management Action: MDOC should take steps to reinforce and ensure a mutual understanding of policy content among all affected parties in the organization, including contract staff. It should also hold its health care services contractor responsible for all training required under the contract, and should require the contractor to provide Office of Program Evaluation & Government Accountability page 20 Health Care Services in State Correctional Facilities documentation demonstrating when the training occurred, what topics were covered, and who was in attendance. A training file for each staff person to document whether and when they have received their annual policy update training and other required training should be kept. 4 Medical Records Should be Maintained Consistently Across the Correctional System MGT noted prisoner medical records were not maintained consistently across MDOC facilities and some medical records did not appear to be updated when health services were provided. This lack of consistency made it difficult to determine whether some prisoners had received the annual health assessments or dental care required, and complicated the transfer of prisoner records from one MDOC facility to another when necessary. There was also inconsistency among facilities in the method used by medical staff to track when prisoners were due for required services like annual physical and dental assessments. The tracking systems were primarily manual in nature, allowing for errors that may explain MGT’s findings that some prisoners had not received their annual physicals and dental exams. OPEGA issued an information brief in spring 2011 on a few topics relevant to managing costs in Maine’s correctional health services (see Appendix B). Those topics included the benefits of implementing an electronic medical records (EMR) system. In addition to reducing costs and providing management with better data for managing health care services, an EMR system would also bring consistency to health care documentation and the tracking of services that could improve prisoner care. The Department has recently decided to pursue getting an EMR independent of the vendor providing its health care services. As a first step in this direction MDOC secured a technical assistance grant from the National Institute of Corrections (NIC) to have a national expert in EMR assess what Maine would need to consider, and do, in order to transition to electronic medical records. The expert conducted his work over the summer of 2011 and presented MDOC with a final report in September. Recommended Management Action: MDOC management should hold the health services contractors accountable for ensuring that medical files at all MDOC medical facilities are organized consistently, updated to reflect services provided to prisoners, and maintained in compliance with MDOC procedures and standards. MDOC should also require the contractor implement an appropriate, standardized system for tracking of required prisoner health services, i.e. annual physical assessments, for all facilities. An EMR system would be beneficial to accomplishing these goals efficiently and MDOC should continue to pursue implementation of an EMR system. Office of Program Evaluation & Government Accountability page 21 Health Care Services in State Correctional Facilities 5 MDOC Should Continue to Pursue Cost Containment Strategies Through New Health Care Services Contract(s) MDOC soon plans to issue a new RFP for correctional health care services after a lengthy period developing the RFP over the course of the change in administrations. OPEGA has reviewed the draft RFP and found it does include a number of the potential cost containment measures recommended by MGT as discussed in the OPEGA Information Brief in Appendix B. Whether the Department is able to realize reduced costs as a result of this RFP depends, to a large extent, on what it receives for bids, how those bids are evaluated, and also on how the final contract for services is crafted to ensure all proposed cost savings are achieved. The Department plans to evaluate bids and select a vendor in the early spring of 2012 for a new contract starting on July 1, 2012. In addition to seeking to contain costs via its new RFP, the Department has also taken some steps to contain costs with its current vendors for the current fiscal year while the RFP process is underway. The CorrectRx contract has been flat funded over the last year, except for a small increase to cover the cost of a new service and an amount required to cover cost overruns from the prior year. The CMS contract has been reduced by $850,000 over the prior year and has also been amended to introduce a risk-sharing funding formula for off-site care. Under this new formula, the Department allows $1,640,000 for CMS’s provision of off-site care and will only cover 50% of any off-site care exceeding that amount. If the actual cost of off-site care is less than $1,640,000, the contract specifies CMS must return 75% of the remaining funds to MDOC. The other 25% is available to CMS as an additional profit and is intended as an incentive for containing costs. Recommended Management Action: OPEGA recommends that MDOC follow through on its plans to issue an RFP and establish a new contract by July 2012 incorporating cost containment strategies where reasonable. Once the contract is finalized, the Department should report back to the Legislature’s Joint Standing Committee on Criminal Justice and Public Safety on what cost management measures are contained in the contract and how they can be expected to affect overall prisoner health costs. Finally, MDOC should monitor its new vendor(s) closely, as outlined in Recommendations 1 and 2, to ensure that all expected cost containment measures are implemented effectively and that all cost savings due to the Department are captured. Office of Program Evaluation & Government Accountability page 22 Health Care Services in State Correctional Facilities Agency Response―――――――――――――――――――――――――――――― In accordance with 3 MRSA §996, OPEGA provided the Maine Department of Corrections an opportunity to submit additional comments on the draft of this report. The new administration has been developing solutions to address the issues raised and other areas for improvement that have since been identified. Actions MDOC expects to take specific to the recommendations in this report are discussed below. 1 MDOC Should Periodically Verify Contractor Compliance with Contract Terms, MDOC Policies and Health Care Standards The new position of Resource Administrator has recently been filled and will be monitoring contractor compliance with fiscal components of the contract. That monitoring is expected to include regular review of compliance with staffing provisions and monthly analysis of contractor bills. The Resource Administrator will attend the monthly calls with Corizon and Correct Rx and will work closely with the MDOC Health Services Coordinator. The MDOC Health Services Coordinator is responsible for monitoring contractor compliance with clinical aspects of the contract. She will make quarterly on-site visits to each correctional facility for the purpose of conducting medical record reviews. These reviews will include audit and examination of various sections of the prisoner medical records for completeness and adherence to MDOC health care policy. A random sampling of offender medical records will be audited at each site during the quarterly visit. A representative of the MDOC Quality Assurance Team will accompany the MDOC Health Services Coordinator on these site visits and gather performance measurement data on the same medical files. The data obtained during quarterly site visits will be compiled into a written report and disseminated to the vendor for review. All quarterly reports will be compiled for ongoing monitoring and trend analysis and data will be used to make future decisions regarding prisoner medical services. As necessary, corrective action plans will be required of the vendor to address any deficient areas identified by auditing or any other means. This monitoring process will become effective January 2012. 2 MDOC Should Strengthen Quality Assurance System MDOC central office staff is currently tracking medical requests and concerns that come into central office using a spreadsheet log. Additionally, monthly meetings are being held between MDOC central office staff, Corizon and CorrectRX to monitor costs and services, and discuss challenges and plans for improvement. The MDOC Commissioner is also in the process of establishing a new Quality Assurance Division within the Department. The primary mission of the QA Division will be to develop and implement a nationally recognized PerformanceBased Management system for corrections. The system includes a whole section on medical care relevant to many of the issues described in this report and will result in the regular collection of data that can help MDOC determine compliance and Office of Program Evaluation & Government Accountability page 23 Health Care Services in State Correctional Facilities make informed decisions about prisoner health care. Establishment of the QA division and how it will interact with regard to the medical contract will be pursued over the next few months. MDOC is getting technical assistance from the National Institute of Corrections on this effort. The new QA Director and staff are being trained by NIC on data collection in November 2011 and will begin implementing a data collection process for the entire adult system. The timeframe for implementation is somewhat dependent on the availability of resources from the Office of Information Technology. 3 MDOC Should Ensure Staff Involved in Health Care Service Delivery are Sufficiently Trained and Knowledgeable of Relevant Policies and Standards New policy and policy changes are already reviewed with staff. However, MDOC will seek additional assurance that all updated policies are available to staff through the new QA methodology. Each facility has a Manual of MDOC policies pertaining to medical services, and medical department staff has access to the Manual. At each quarterly site visit, the MDOC Health Services Coordinator will review the MDOC Medical Policies and Procedures to ensure that the most current policies and procedures are being utilized at each facility. Additionally, at least one MDOC policy pertaining to medical services will be reviewed at medical department staff meetings at the respective facilities each month. A MDOC policy pertaining to medical services will also be reviewed at each Medical Audit Committee meeting at each facility. Those reviews are to be reflected in the minutes of each meeting. 4 Medical Records Should be Maintained Consistently Across the Correctional System In September 2011, the National Institute of Corrections provided a consultant to review the Maine Department of Corrections health care system and the potential benefits of transitioning from a paper-based system to an electronic health record system. The consultant’s report recommends that MDOC pursue implementing an electronic medical record (EMR) system to increase efficiencies and standardize health care records and tracking systems. For several reasons, MDOC would prefer to pursue the purchase and implementation of an EMR system that is independent from whichever vendor may be selected to provide the correctional health care services. There is no funding available for an independent EMR system, however, and, therefore, the MDOC will consider an EMR system in the next RFP for health care services that is soon to be issued. If an EMR system does not get implemented, the MDOC will continue to monitor and improve medical records and tracking of required medical service as part of the on-going compliance and quality assurance review processes described in Actions 1 and 2 above. Office of Program Evaluation & Government Accountability page 24 Health Care Services in State Correctional Facilities 5 MDOC Should Continue to Pursue Cost Containment Strategies Through New Health Care Services Contract(s) As previously described in Recommendation 5 on page 22, MDOC intends to explore several cost containment strategies through the upcoming RFP for health care services and has also taken recent steps to reduce costs associated with current contracts. Those steps include amending the current contract with CMS to introduce a risk-sharing formula for off-site care and holding monthly meetings with Corizon and CorrectRX where the focus is on cost savings opportunities. These steps have proved extremely beneficial over the last 3 months as shown by these statistics (comparing to same time period as last year): Emergency room visits - down 88% with no admissions during the past three months; Inpatient days – down 66%; Outpatient Referrals – down 55%; RX costs (July-Oct 2011) – down 18%. Acknowledgements ―――――――――――――――――――――――――――― OPEGA would like to thank the management and staff of the Maine Department of Corrections for their cooperation during this review. Additionally, we appreciate the technical expertise and perspective that MGT of America, Inc., brought to this project. Office of Program Evaluation & Government Accountability page 25 Appendix A. Scope and Methods Health Care Services in State Correctional Facilities Early in this review, OPEGA decided to contract with a consultant to perform the majority of work on this project in order to benefit from the expertise of auditors that have reviewed medical services in correctional settings across the country. OPEGA selected MGT of America, Inc. through a competitive Request For Proposals process. MGT completed the majority of their work during the fall of 2010. To obtain an understanding of Maine’s correctional health care system, MGT reviewed relevant laws, regulations, and policies and identified those that were applicable and significant to the audit. In doing so, MGT reviewed MDOC’s policies and procedures related to contracted services. Also, MGT obtained documentation from MDOC headquarters and facilities. Finally, MGT interviewed MDOC and CMS staff to assess their roles and responsibilities with regard to health care services in MDOC. To develop an understanding of service delivery issues and assess MDOC’s contract monitoring processes, MGT examined monitoring terms and practices, quality assurance methods, claims processing procedures, and internal reviews. Also, MGT assessed contract administration, contractor responsiveness, MDOC operations, resources, external issues, and availability of medical professionals. To determine the level of compliance with key contract terms, MGT reviewed performance, contract staffing plans, penalties for vacancies, performance metrics, performance standards, and management reporting. MGT also performed detailed testing of a judgmental sample of the populations at the two largest adult facilities and one juvenile facility to determine compliance levels with contract terms and accepted standards of care. MGT weighed the data and information gathered against criteria including known best practices, industry standards, benchmarks to comparable peer jurisdictions, and established federal and state legal requirements and departmental goals and objectives. Specific work conducted by MGT during this review included: • Interviewing state and contracted managers and staff responsible for each facet of the delivery and administration of Maine’s correctional health care services, as needed; • Reviewing MDOC’s and contractors’ documented policies and procedures concerning the delivery and administration of health care services; • Reviewing MDOC’s contracts for medical and pharmaceutical services, including contract extensions and amendments, their approvals, and the purpose of each revision since 2004; • Conducting site visits of the nine correctional facilities, inspected the healthcare facilities, and analyzed operations with respect to the provision of health care services; • Interviewing the CMS regional manager and medical directors (outgoing and incoming); • Reviewing MDOC healthcare reports, reports of various committees and working groups in Maine, relevant audits, planning documents, as well as reports and meeting minutes that resulted from regular and special meetings related to MDOC’s health care services; • Reviewing laws, regulations, medical standards, and healthcare best practices; • Reviewing healthcare performance reports, metrics, and statistical reports; • Performing detailed review of a judgmental sample of prisoners’ medical files and medication administration reports at the two largest adult facilities (MCC and MSP) and one youth facility (LCYDC) to determine compliance with key contract provisions; • Reviewing extensive documentation related to site-specific practices, policies, procedures, reports, grievances, training records, co-pay tracking, contract monitoring, and other health care administration and delivery documentation for MCC, MSP and LCYDC; • Reviewing medical-related prisoner grievances and the grievance processes; • Evaluating MDOC’s current and planned practices related to elderly prisoners and end-of life health care services and comparing MDOC’s population to national correctional healthcare trends; Office of Program Evaluation & Government Accountability page 26 Health Care Services in State Correctional Facilities • • • • Analyzing MDOC’s methods for procurement of medical and pharmaceutical services and methods for contract oversight and administration; Reviewing contractor invoices and billing data for fiscal year 2009-10 and testing 100 percent of all invoices and statements during the year for appropriate review, approval, and calculation of billing paybacks and administrative penalties; Evaluating the information technology systems and manual record-keeping systems in place at MDOC’s healthcare facilities; and Requesting data from MDOC’s prisoner record management information system and human resources system. MGT presented OPEGA and MDOC with a draft report of results and recommendations in December 2010. Since that time OPEGA has been working with the Department to understand the root causes of some of the issues identified by MGT and to discern what actions the Department planned to take to resolve the issues. These discussions with management took much longer than is typical because of the significant changes occurring at the Department between January and August of 2011. Over that period of time, MDOC’s management team changed, as did its response to MGT’s findings. As a result, OPEGA staff spent additional time meeting with management and reviewing documentation to understand and confirm the changes being made within the organization. This report has been structured to incorporate all of the most current information about the status of health care services within Maine’s correctional system. Office of Program Evaluation & Government Accountability page 27 This Page Left Intentionally Blank Appendix B. OPEGA Information Brief OPEGA Health Care Services in State Correctional Facilities: Opportunities to Contain Costs and Achieve Efficiencies Information Brief Revise Contract Structure, Terms and Conditions Purpose Overview OPEGA has a review of health care services in Maine’s correctional system in progress. The review is primarily focused on the performance of key contractors MDOC uses to deliver health care services, and MDOC’s monitoring of those contractors. OPEGA engaged MGT of America, a national consultant with expertise in the provision of health care services in correctional facilities, to assist with this review. The final report is expected later this spring. This Information Brief discusses some of the specific suggestions MGT made for steps Maine could take to contain future costs and achieve efficiencies, while maintaining or improving the quality of care available to prisoners. MGT shared its suggestions with MDOC, which is interested in pursuing them. Implementation will require planning and action that should begin immediately if the State desires to reap benefits within the next several years. The Legislature may wish to discuss these opportunities with MDOC during this legislative session in the context of the Department’s priorities and any associated resource issues. April 2011 No SR-MEDSERV-09 Maine’s Department of Corrections (MDOC) operates nine correctional facilities—two for juveniles and seven for adults—housing more than 2,000 prisoners as of December 2010. Each facility offers some health care services, and when a facility is not able to provide the level of care a prisoner requires, the prisoner may be transported off site to another correctional or health care facility to receive the necessary care. Although a few State A employees still participate in the delivery of care, most services are provided through contracts with third parties. A summary of the services provided at each facility, and by which contractor, is provided in Table 1. Table 1. Summary of Health Care Services and Providers by Correctional Facility ADULT FACILITIES MEDICAL DENTAL PHARMACY Bolduc Correctional Facility CMS / MDOC CMS Correct Rx Central Maine Pre-Release Center CMS CMS Correct Rx Charleston Correctional Facility CMS CMS Correct Rx Downeast Correctional Facility CMS / MDOC CMS Correct Rx Maine Correctional Center CMS CMS Correct Rx Maine State Prison CMS / MDOC CMS Correct Rx Women's Reentry Center CMS CMS Correct Rx JUVENILE FACILITIES MEDICAL DENTAL PHARMACY Long Creek Youth Development Center CMS / MDOC CMS Correct Rx Mountain View Youth Development Center CMS CMS Correct Rx Legend: CMS = Correctional Medical Services; MDOC = Maine Department of Corrections Source: Information provided by the Maine Department of Corrections. As shown in the summary, Correctional Medical Services (sometimes supported by MDOC staff) provides all medical and dental care, and Correct Rx provides all pharmaceutical services. Contracts with these entities are supported only by General Fund resources and amounts expended for FY 2010 totaled $12.0 million under the Correctional Medical Services (CMS) contract and $2.7 million for Correct Rx. MDOC has contracted with CMS since 2003 and Correct RX since 2007. MDOC’s use of long-term, open-ended contracts diminishes vendor incentives to continually reduce costs. In addition, MDOC’s contracts with CMS and Correct Rx are “cost-plus” contracts. In these types of contracts the vendor is reimbursed at a specific rate, which includes actual costs for staff and services provided plus an amount to cover vendor overhead and profit. Cost-plus contracts are generally used in systems where costs are very well-defined and/or fixed, with little opportunity for cost savings. MGT of America (MGT), the correctional health care expert OPEGA hired for this review, noted two problems with this approach for contracting health care services from the standpoint of controlling costs: Office of Program Evaluation & Government Accountability (207) 287-1901 http://www.maine.gov/legis/opega/ Information Brief – Health Care Services in State Correctional Facilities 1. The State assumes all of the risk in managing health care costs and there is no financial incentive for the vendor to achieve efficiencies or reduce spending. Because the vendor is simply reimbursed for actual staffing and off-site care costs, they receive little direct benefit from any efforts to manage utilization and reduce health care spending. Whether hospitalization costs run high, or are instead below projections, the vendor simply passes these costs along to the State. One of the primary benefits of privatization is for the State to minimize its risk for escalating costs by shifting responsibility for management of those risks to vendors with very specific expertise in correctional health care management. Under the cost-plus approach, the vendor assumes no risk and opportunities to achieve efficiencies often expected from privatization of correctional health care are minimized. 2. Cost-plus contracts increase the administrative burden on the vendor, which passes additional processing costs back to the State. The burden is also larger on the State directly, due to workload associated with confirming actual vendor spending and reconciling payments against those expenditures to ensure the actual cost of care was paid to the vendor. In an alternative arrangement where the vendor’s compensation is fixed, administrative costs like reconciliation are avoided. Contract structures and terms that put the vendor at risk of losing money if costs exceed a certain level, or conversely provide an opportunity to increase profits if expenditures are reduced, are more likely to encourage effective cost management – particularly when vendor risk is allocated to those areas where the vendor’s experience and expertise can most effectively be leveraged. MDOC’s current contracts with CMS and Correct Rx do not include these kinds of risk sharing provisions and do not provide substantial financial incentives to aggressively control costs. However, the term of the CMS contract expires at the end of June 2011 and the Department has been preparing to issue a Request for Proposal (RFP) for correctional health care services. The upcoming bid of this contract is a good opportunity to bring competitive pressures to bear to reduce health care costs. MDOC has plans to incorporate some of MGT’s suggestions, as described below, into the RFP. Opportunities for Improvement MGT of America noted a number of proven contracting approaches that could contain future costs or generate cost savings in correctional health care services. The key to most of these approaches is to shift risk to the vendor, allowing them to increase their profitability as they decrease health care costs. Generally these approaches require vendors to bid a fixed price to cover the cost of health care services provided outside of correctional facilities. Establishing a fixed price incentivizes the vendor to effectively manage utilization, negotiate discounted rates for service and audit bills to achieve maximum efficiency in providing service. Providing vendors with opportunities to reduce their costs through their own performance should also increase competition for these contracts as they become potentially more profitable for more companies. Alternative approaches MGT has observed as providing the most savings assign vendor risk to relatively predictable areas, as well as to those areas where vendor experience and expertise can yield savings. For example, the contract could require the vendor to assume responsibility and financial risk for managing and controlling off-site care costs, but also establish catastrophic caps. These caps can be used to put a ceiling on vendor responsibility for individual case cost, or to share the cost of care beyond a certain level. Catastrophic caps are beneficial because they can eliminate the vendor’s built-in cost for stop loss insurance by reducing the vendor’s overall risk for high cost cases. This allows vendors to more effectively price routine care and avoids additional risk premium costs to cover the major cases that might, or might not, occur. Other costs, such as those associated with HIV, Hepatitis C, Factor VIII and IX, and organ transplants, can be very unpredictable. Vendors who must pay these full costs typically build a risk premium into their contract bid to cover these potential costs. The State could, instead, take responsibility to pay these costs in full, outside of the vendor contract. This allows the State to pay only the costs that actually arise rather than pay higher on-going rates to cover a built in premium based on potential costs in these areas. OPEGA observed that a contract that shifts risk to the vendor, and subsequently allows the vendor increased profit opportunity, could potentially entice a vendor to make decisions that would increase profits, but be detrimental to the quantity and quality of services provided to prisoners. The best control to prevent this from happening is 2 Information Brief – Health Care Services in State Correctional Facilities prudent contract administration and a strong system for monitoring vendor performance. MDOC would need to strengthen its current monitoring procedures to ensure quality of care under a non-cost plus contract. Aside from recommending a move away from cost-plus contracting, MGT also noted a number of measures that have worked in other states to better manage costs and increase efficiencies, regardless of whether a cost-plus, or some alternate contract model is used. These approaches include: • Set staffing reimbursement rates at 90 percent of contract requirements. CMS is currently paid each month on the basis of the full amount of staff hours required in the contract. There is then a monthly reconciliation process to determine what credits are due to MDOC for contracted hours that were not provided. According to the CMS regional manager, CMS’ accounting staff spends significant time preparing monthly reports based on actual time records, comparing on-site staff time to the contract staffing requirements. These calculations are then checked by MDOC staff. This monthly reconciliation can be quite detailed and time-consuming given the amount of vacancies present at any given time and normal staff time off. An alternative approach recognizes that staff fill rates seldom approach the contracted level and reduces monthly upfront payments to the vendor to recognize that. A number of systems pay vendors on the basis of 90 percent of contract hours provided, then just reconcile once a year to account for any overages or underages. The end result is improved cash flow for the Department due to reduced upfront payments, a simplified reconciliation process, and reduced overhead for both the Department and vendor as reconciliations are cut from 12 per year to once annually. • Consider including requirements for a comprehensive Electronic Medical Records (EMR) system in the RFP. The cost of these systems has come down in recent years, and acquiring a system through the contract process allows the cost of the system to be amortized over the life of the contract. MDOC should specify that any EMR system be non proprietary in nature, be compliant with any federal guidelines and be a system that is already operational on a large scale. The RFP should also continue to include telemedicine with requirements that the vendor have experience in developing and conducting those services. MGT has observed that integration of telemedicine and EMR systems have allowed a number of correctional systems nationally to dramatically improve the efficiency of service delivery. (See the EMR section on page 6 of this Brief for further discussion.) • Encourage bidders to propose alternative staffing plans. In structuring the RFP, all vendors should be asked to bid on the same staffing plan. However, MDOC should also request that bidders propose alternative plans, tied to specific benchmarks of service, that can be used for negotiations. While the staffing pattern MDOC uses may be appropriate for Maine, vendors with extensive expertise in managing correctional health care services may have different approaches that could generate savings. MGT also observed that converting all remaining State health care positions to contract positions in the RFP could be helpful in addressing administrative issues associated with the joint management of contract and State staff in the same unit. OPEGA observes that such a conversion would require changes to the Department’s appropriations and authorized positions and would likely have union contract implications. • Consider including pharmacy with medical services as a comprehensive contract. MGT finds that separating out medical and pharmaceutical services often drives up cost and dilutes accountability. An alternative model makes the vendor that is responsible for prescribing medication bear the financial consequences and risks of those prescribing practices. MDOC has had negative experiences with combining these services under one vendor in the past and believes this is a situation with both pros and cons that should be carefully considered. • Establish a fixed contract term of 3-5 years. A multi-year fixed term contract in this range allows a vendor a sufficient time horizon to recoup investments in the system, but also retains the benefit of competitive bidding for the Department. • Consider establishment of incentive programs, tied to performance benchmarks, to contain costs in medical care as well as other related areas such as security and transportation. MGT has found structured incentive programs are good alternatives to penalty programs, and will often generate improvements in medical outcomes, greater efficiency in delivery of care and more creative ideas in managing care. The establishment 3 Information Brief – Health Care Services in State Correctional Facilities of benchmarks for health outcomes is, however, critical to ensure appropriate care is not being shortchanged to meet incentives. Services that exceed the set benchmarks are rewarded with incentive payments. Incentives can be readily established for staffing fill rates. Another area where incentives could be beneficial is off-site care. Adding incentives in this area should motivate the contractor to find ways to provide services on site, reinforcing such things as telemedicine, chronic disease management, on site specialty care, and effective infirmary use. • Look for vendors with strong utilization management programs. RFPs should require bidders to provide a full explanation of their utilization management programs and MDOC should assess each program’s comprehensiveness. RFPs should not specify what should be included in the vendors’ utilization management programs. Rather, MDOC should look for those programs that have built-in systems designed to continually improve service management, such as where doctors and other clinical staff consult on and review cases to bring in multiple levels of expertise. A well designed utilization management program should help identify and manage high cost areas. Improve Planning and Care Alternatives for Chronically Ill and Elderly Prisoners Overview According to the Bureau of Justice Statistics in 2008, 4.7% of states’ prison populations were 55 years of age and older. Prisoners in their fifties are often considered geriatric due to their generally poor health and shorter life expectancy. While the number of these prisoners is small, they present special challenges in the delivery of health care. The cumulative effects of aging often mean they require more medical services, including costly long-term care. According to the National Hospice and Palliative Care Organization, end of life care in correctional settings will become increasingly necessary in coming years. As the number of aging and ill incarcerated men and women increases, correctional facilities’ methods to manage these prisoners in a humane and cost-effective manner are of particular importance. In addition, such care is guaranteed under the Civil Rights of Institutionalized Persons Act (CRIPA) and Americans with Disabilities Act Amendments Act of 2008 (ADAAA). In November of 2010, MDOC reported 189 prisoners 55 years of age or older in the State prison population. This group represented 9% of the total 2,094 prisoners in the population. Table 2 includes a breakdown of MDOC prisoners by age group and number of years until release. At the present time, Maine has no method of tracking medical costs specific to geriatric prisoners regarding use of specialists, types of treatment, durable medical equipment, health care appliances and medications. As a result, the exact cost of providing care for this group is currently unknown. Table 2. MDOC Population: Age and Years Left Until Release as of November 19, 2010 Years Until Release Age Total 51-55 56-60 61+ < 1 year 38 19 21 78 1 to 3+ years 37 23 28 88 4 to 5+ years 11 4 9 24 6 to 10+ years 11 9 8 28 11 to 20+ years 11 8 8 27 MDOC has few options for providing services to chronically ill or geriatric prisoners when the 21 to 30+ years 10 3 1 14 care they need is not available at the facility in >30 years 6 4 3 13 which they are housed. The Department does have a Medical Supervised Community Life 7 8 13 28 Confinement Program, which provides for community confinement of prisoners with Total 131 78 91 300 terminal, or severely incapacitating, medical Source: MGT America. conditions when care outside a correctional facility is appropriate from a medical and security perspective. When approved by the MDOC Commissioner, prisoners under this program live in a hospital or other appropriate care facility, such as a nursing facility, residential 4 Information Brief – Health Care Services in State Correctional Facilities care facility, or a facility that has a licensed hospice program. They are essentially under the supervision of the community facility, but may also be subject to periodic probation type check-ins. Under this program, the Commissioner also can approve home placement for prisoners that are at end of life and present no risk to others, if appropriate services can be arranged. Funding for these alternative placements varies according to a prisoner’s individual circumstances with MaineCare or private insurance. MDOC reports that, despite a tremendous amount of effort applied toward community placement, making it work is difficult. Since the Program’s inception, there have been three prisoners placed in alternative settings. One prisoner was approved for home placement. The prisoner’s overall health condition improved, to the extent the prisoner was re-assigned to a community facility, reached the end of his sentence and was released. Two other prisoners were placed in community facilities, but following significant problems both were returned to MDOC facilities. At present, there are no prisoners in this program. For those prisoners not suitable for community placement, however, the MDOC often must move them to a higher security facility where the medical care they require is available. This practice is not uncommon. MGT reports that many correctional systems tend to concentrate health care services at high security facilities due to the longer stays and more intensive needs of prisoners at these facilities. However, this ties up valuable infirmary beds available for treating the remainder of the population and may result in ill or elderly patients being held in a more restrictive (and therefore more costly) environment than is necessary. The more restrictive environment may also limit prisoners’ access to programs and services that may be required for rehabilitation or which must be successfully completed prior to consideration for release or community placement. Making special accommodations to continue such programming for ill or elderly prisoners moved to high security facilities is sometimes possible, but represents yet another additional cost. MDOC reports that currently four of the six infirmary beds at the Maine State Prison are filled, due to lack of alternatives for other appropriate placement, with prisoners who have long term care needs. Many more are also at risk of needing a bed for long term care. MDOC could be immediately facing a situation where it does not have enough infirmary beds for those needing long term care and will have to bear the expense of placing prisoners in off-site hospital beds instead. This situation would also mean there are no infirmary beds to house prisoners who have short term sicknesses. The Department has also expressed concern about housing the elder population in the future. Secure bed space, physical plant design, access to programs and services, medications, special diets, distance to emergency hospital services, and preparation for community re-entry are some of the expected challenges for this population. MDOC has contacted some other states regarding management of this population, but currently has no formal short-term or long-term plans to strategically address the issue. Opportunities for Improvement MGT suggests that MDOC consider the following actions to ensure appropriate planning and administration of health care services for chronically ill and elderly prisoners in the future: 1. Review MDOC’s strategic plan and revise accordingly, with specific goals, objectives and strategies listed for bed planning and health care management of the aging population, using the “right prisoner, in the right bed, for the right reason” method to utilize the best and most efficient resources. 2. Continue to analyze current data, and gather new data as needed, in order to identify: • costs of elder care; • medical and health care conditions most often being treated; • medications most often being prescribed; • prisoner demographics including gender, age, most severe crime committed, average length of sentence; • types of disabilities being managed; • typical kinds of accommodation requests being received and how those requests are being managed; • use and management of health care appliances and durable medical equipment including associated security implications; and • food service costs related to special dietary needs. 5 Information Brief – Health Care Services in State Correctional Facilities Such information will provide hard facts as a basis for MDOC and the Legislature’s future discussion of this issue. 3. Review current housing, programs, and staff supervision policies for this population. Evaluate the impact of ADAAA requirements on management of geriatric prisoners. 4. Conduct a review of end-of-life services and procedures using quality guidelines for hospice and end-of-life care in correctional settings developed by the National Hospice and Palliative Care Organization and seek opportunities for technical assistance, if possible. According to MDOC, there is a hospice program at the Maine State Prison as dying prisoners are most likely to be in the infirmary beds there. 5. Review policies, procedures, and practices related to infirmary care and associated costs. The Legislature may also want to consider further study of issues surrounding Maine’s geriatric corrections population. MGT suggests the cost of such a study may eventually be viewed as a small, upfront investment with a large benefit in the future. Community supervision, housing, ongoing and available treatment programs, employment, transportation, restitution, and reunification of families are some of the significant topics for consideration. Implement Electronic Medical Records System Overview MDOC’s current system of record keeping associated with prisoner health care services is mostly manual and varies from one facility to another. Archival of MDOC’s prisoner health care records appears to be bulky and burdensome for storage and access. According to MDOC and CMS staff, if a prisoner returns to the custody of MDOC, there is often a significant delay in researching and acquiring the prisoner’s prior paper medical charts and records from a central archive location. This practice is not efficient. It can result in creation of duplicate files and require additional staff effort, thus driving up unnecessary administrative costs. In addition, MDOC facilities do not have access to digital medical records used by doctors’ offices and hospitals in the community. This situation makes it difficult to obtain records for individual prisoners who have received care in non-institutional settings. Manual records and files also limit the ability to collect and analyze data on health care service delivery that should be used for effective utilization management, monitoring of contractor performance, planning for the prison population’s health care needs and tracking costs. Performance-based health care standards also call for collecting, analyzing, and actively using performance improvement data to foster quality assessment and performance improvement in all areas of care. Electronic Medical Record (EMR) systems offer users several benefits in the correctional setting. Centralizing the data allows access at any time, from any location by approved medical professionals. Difficulty in reading the handwriting of others is eliminated. Patient privacy is maintained. Required field completion and a defined sequence for entering notes about patient therapy, treatment and medication reduces errors and makes patient records more consistent. A link to pharmacy services is possible that could improve medication management, as well as links to daily, real-time prisoner moves, allowable property lists noting approved health care appliances and durable medical equipment, and information about special dietary needs. In addition, paperless record keeping contributes to storage space efficiency. With appropriate backup systems, historical data can be maintained indefinitely and valuable physical space that was previously used for bulky paper files can be repurposed. When agencies opt for “certified electronic health record technology,” systems may be compatible with jails and hospitals in the community. The end result is administrative efficiencies, improvements in record keeping, and valuable stored data that can be accessed at a moment’s notice in order to report on trends, demographics, housing or security issues, and many other topics that may be of use to legislators and management in considering issues of prisoner health care. 6 Information Brief – Health Care Services in State Correctional Facilities MGT reports that correctional systems in other states have adopted EMR systems, and in some cases have leveraged health care contracts to introduce the needed technology. However, though the value of such systems is evident, the initial cost can be high, depending upon the size of the correctional system and functionality required. MGT notes that states are often able to negotiate with vendors to have the cost of EMR implementation amortized over the life of the vendor’s contract so the State does not have to absorb the full cost in one year. Aside from financial investment, implementing an EMR system can also take a substantial investment of time and energy on the part of the Department. For an implementation to be optimally successful, the correctional system must prepare by undertaking a review of all processes, and reengineering them where necessary, to ensure procedures mesh efficiently with the new EMR system and maximize its effectiveness. This process assessment requires the involvement of stakeholders at all levels in the organization and, if substantial process change is necessary, can also result in a need for significant training hours to ensure all staff are adequately prepared to adhere to new procedures. MDOC has been interested in implementing an EMR system for some time and, in fact, has previously pursued obtaining this technology through an arrangement with a third party as the system CMS offered was not suitable. Those plans were disrupted, however, and until recently MDOC had not renewed efforts to get an EMR system in place. According to the Department, an EMR Task Force was activated a few months ago and is actively seeking the most cost effective medical management system. The National Institute of Corrections will be providing MDOC with assistance and guidance in this effort. Opportunities for Improvement The effective use of a functional and well-designed EMR system can drive improvements in the quality and efficiency of health care services delivered in Maine’s correctional system, potentially encompassing both State institutions and county jails. MDOC, with the involvement of the State’s Office of Information Technology, is again actively pursuing the selection and implementation of an EMR system. This system should be proven, compliant with federal guidelines and compatible with other systems, both public and private, with which it needs to, or should, interface. MDOC could explore the acquisition of such a system through the upcoming RFP process for medical services by soliciting bidders’ proposals on an EMR system as well as increased use of telemedicine. Any EMR system implemented by a MDOC vendor should be required to be non-proprietary in nature so MDOC maintains both the system and its future ability to bid out health care services. According to MGT, the integration of telemedicine and EMR systems has dramatically improved the efficiency of service delivery for a number of states’ correctional health care systems. Consequently, MDOC should also consider requiring vendors bidding on the new RFP to have experience in developing and conducting actual telemedicine services. The Department will likely need the Legislature’s support of the initiative to implement EMR as it could represent a significant investment of both human and financial resources. The Legislature can help assure that this effort remains a priority for MDOC and that adequate resources are appropriated and well spent by the Department. 7