Goldenson Report Herrera v Pierce County 8-5-2008
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
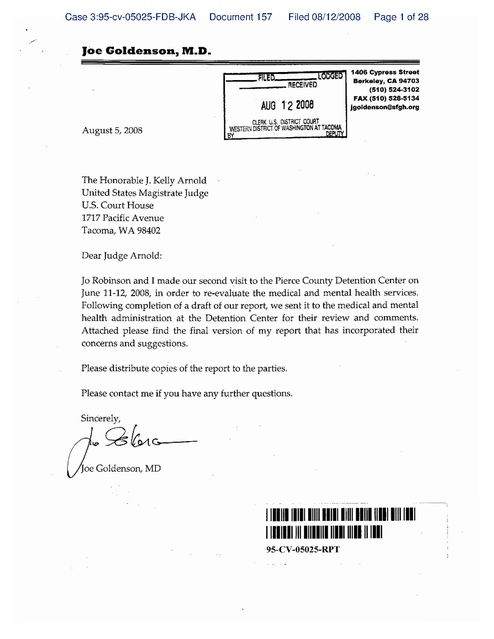
Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 1 of 28 ·..... Joe Goldenson, M.D. _--_n----..,.,~~ 1406 Cypress Str_t CII Cl'\ I t'\l'Vlr: _ _ _ _- RECEIVeO Berkeley, CA 94703 (510) 524-3102 FAX (510) 528-5134 jgoldenson@sfgh.org . AUG l2 2008 August 5, 2008 ClERK U.S. DISTRlCf COURT J.fSTERN DISTl1ICT.OF WASHINGTON ATT~~~~ The Honorable J. Kelly Arnold Uriited States Magistrate Judge U.S. Court House 1717 Pacific Avenue Tacoma, WA 98402 Dear Judge Arnold: Jo Robinson and I made our second ~isit to the Pierce County Detention Center on June 11-12, 2008, in order to re-evaluate the medical and mental health services. Following completion of a draft of our report, we sent it to the medical and mental health administration at the Detention Center for their review and comments. Attached please find the final version of my report that has incorporated their concerns and suggestions. Please distribute copies of the report to the parties. Please contact me if you have any further questions. Sincerely, ~g~~oe Goldenson, MD .. 111111111111111111111111111111111111111111111 1111111111111111111 1111111111111111 95-CV-05025-RPT _._---\ Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 2 of 28 PIERCE COUNTY DETENTION & CORRECTIONS CENTER HEALTH SERVICES Sandra Herrera, et al v. Pierce County, et al United States District Court Western District of Washington Case No. C95-5025FDB REPORT OF FINDINGS Submitted by: Joe Goldenson, MD August 5, 2008 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 3 of 28 This is the second progress report of Court Monitor Joe Goldenson, MD, on the status of health care services at the Pierce County Detention & Corrections Center (PCDC) in Tacoma, Washington. Jo Robinson, MFT, assisted in the evaluation of the mental health services. Ms. Robinson and I visited PCDCC on June 11 and 12, 2008. We toured the facility, reviewed medical records, and interviewed patient-inmates, health care staff, and custody staff. In addition, I met with Chief Masko and Craig Adams to discuss some of the areas that will need budgetary support, such as the need for additional staff, in order for the facility to come into compliance. The audit conducted during our visit was not comprehensive. We primarily focused on those administrative and programmatic issues that we had identified as needing improvement during our prior visit on November 15-16, 2007. In our first report, we had recommended a number of corrective actions and studies related to the areas of our concern. Prior to our second visit, we requested updates on these activities. We did not, however, receive most of the requested information until the day of our visit, so we did not have an opportunity to review it before our arrival. In addition, we did not have the time during this visit to fully evaluate the quality of the clinical care. We will look at this area during future visits through a more extensive review of medical records. This report will address the issues and concerns raised in our first report and any new findings that we made during our recent visit. Discussions of areas that were previously found to be in compliance will not be repeated. As noted in our prior report "PCDC has expressed a desire to use the National Commission on Correctional Health Care (NCCHe) Standards as their guidelines and final goalpost for their health care system." While the standards are not in and of themselves proof of an adequate health care system, they do represent a "well thought out and systematic approach to the difficulties of providing a quality system of health care in corrections, and have consistently shown a high level of concern for inmate welfare." For these reasons, this and future reports will follow the outline of the NCCHC standards, and will comment on progress towards meeting the standards. Compliance with the standards does not guarantee, however, that the clinical care being provided at a facility is adequate. As indicated above, future reports will also evaluate the quality of care based ~pon a clinical review of selected medical records. It is important to note, that while the NCCHC standards are used as a method of organizing the reports, the findings and recommendations related to compliance with the Stipulated Order and Final Judgment are not based on those standards. Our findings and recommendations are based on what changes are necessary, in our professional judgment, for the health services at the peDC to meet a constitutional level of care. Prior to submitting this report to the Court, we sent a draft copy to the health care staff at peDC for their review and comments. We have incorporated many of their suggestions Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 4 of 28 into this final report. As during our prior visit, the health care and corrections staff graciously assisted us throughout our stay and answered all of our questions. They were completely cooperative with our requests, and we would like to express our appreciation and gratitude for their support of our monitoring effort. Without their help and cooperation, our task would have been unachievable. REPORT The population of the jail was 1,279 on June 11, 2008 (as compared to 1,458 on November 15, 2007). There were 616 inmates in the main facility and 663 in the new facility. There were approximately 75 to 80 new bookings per day. Medical and Mental Health Infirmary/Sheltered Living Level Housing The usage of the cells in the health services area of the main jail that are designated to be medical and mental health beds has not changed since our first visit. For the most part, they are not being utilized due to a lack of necessary custody and nursing positions. The exceptions to this are: (1) patients who are being evaluated for suspected tuberculosis disease are occasionally housed in the negative pressure airborne isolation rooms; and (2) patients who require a higher level of medical care than is available in general population are sometimes housed in the medical beds. In those cases, custody and medical staff is increased in the clinic area. Medical administrative staff has recently developed a Special Housing policy that addresses the use of these medical rooms. In addition, they have been tracking the number of patients that are housed in the airborne isolation, infirmary, and sheltered living rooms, as well as the reason for such placement. They have also conducted a survey of incoming and long-term inmates to determine the number who would benefit from sheltered living or infirmary housing such as high risk diabetic, cardiac, or asthmatic patients, individuals at high risk for alcohol withdrawal, high risk pregnant women, post-operative patients, and patients requiring observation. As a result of these activities, the medical staff concluded that, while it was not necessary to fully open and staff this unit, there was a need for more flexible use of these beds in order to appropriately house patient-inmates who require more care and/or monitoring than can be provided in general population. In order to accomplish this, the staff determined that an additional full-time licensed· practical nurse (1.0 FTE plus relief) would be necessary during the day shift. This position would also provide coverage to the clinic area, which is chronically short-staffed due to lack of relief when nurses are sick or on vacation. In addition, custody staff would need to be available to perform the required 3D-minute checks and to provide nighttime relief to 2 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 5 of 28 the registered nurse during his/her lunch break. The policy on Special Housing should be revised to reflect these changes, including a discussion of who can make the decision to place a patient into this unit as well as the procedure whereby medical and custody staff will coordinate their activities when a bed on this unit needs to be opened. Access to Care As noted in our prior report, the triage nurses who evaluate patients who have submitted health care requests only work five days per week. On weekends, the medical kites (request forms) from the main jail are reviewed by a nurse in the clinic and those from the new jail are reviewed by the nurse at intake. As a result, only patients with "urgent" complaints are seen over the weekend. Those with "non-urgent" complaints are deferred until Monday. In OUr first report we noted that, "Many inmates, however, are medically unsophisticated and have poor writing skills, and therefore, the kites may not accurately reflect the urgency of their medical problems. In many cases, such as patients complaining of headaches or abdominal pain} more information than is written on the request is required before the immediacy of need can be determined. A nurse needs to interview such inmates in order to determine the urgency of their problem. Given the responsibilities of the booking and clinic nurses, it is not clear that they have enough time to adequately screen the medical kites on the weekends." Subsequent to our first visit, the medical administrative staff reported to me that they had concluded that there was a need for 7-day per week nursing tria·ge. In order to accomplish this, they determined that they would require an additional 2 full-time registered nurses (2 FTE's plus relief). After reviewing the draft version of this report, Vince Goldsmith informed me that PCDe does not agree that more staff are needed. Since this issue has not been resolved, peDC needs to conduct the quality improvement study· recommended in the first report to evaluate the process by which inmates access care. This is also an area that I will review during future visits. After evaluating a patient, the triage nurses can address minor medical complaints through the use of protocols; consult with Dr. Balderrama, the Medical Director, or one of the Physician Assistants; or refer the patient to the medical clinic in the main jail for further evaluation and care. In his final report} Dr. Shelton had recommended that peDe implement a training program for the nurses on triaging, "including history, exam, findings and what is urgent, what is routine, what can be handled by self care methods." Medical administrative staff informed us that they are in the process of arranging for a nursing assessment and skill-training course that will take place in the fall. We did not formally evaluate how long it took for patients to be seen by a practitioner following referral, but it appeared that those in general population units were being seen within an acceptable time frame. We will review this in more detail during future visits. Access to medical care in special housing units remains problematic. While there has 3 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 6 of 28 been improvement, the required three-times per week nursing rounds are not always occurring. (Monitoring reports revealed that checks were done 100% of the time in February and April, they were only done 80% of the time in December and January, and 75% of the time in March.) In addition, staff reported that patients from these units are still not being seen in a timely manner for nursing care or provider sick call. Chart reviews of inmate-patients who were housed in administrative segregation revealed the following examples: Patient 1 On 5/20/08, the patient was referred on an urgent basis to see a provider for evaluation of tingling and numbness in his hand. He was not seen until 6/6/08. There were daily nursing notes prior to his being seen stating"staff unable to see." Patient 2 The patient was scheduled to be seen for follow-up of his asthma on 5/23/08. As of 6/12/08, he had not been seen. Patient 3 The patient was scheduled to be seen for follow-up of his hypertension on 5/20/08. There was a note in his record that he refused on 5/20 and again on 5/23. There were, however, no refusal forms in the medical recordr and no evidence of counseling or further followup. Patient 4 The patient has a history of a deep vein thrombosis for which he had been taking Coumadin (an anti-:coagulant) prior to his arrest. The medication was ordered when he entered the jail on 6/3/08. On 6/5/08, a blood test revealed that his INR (a blood test used to determine if a patient is receiving the correct dose of Coumadin) was sub-therapeutic, indicating that he was at risk for further blood clots and that his Coumadin dose should be increased. This is a problem that should be addressed on an urgent basis. The patient had not received any follow-up as of 6/11/05. PatientS The patient was booked into the jail on 6/6/08. Prior to his booking, he had been taken to the emergency room for treatment of dog bites. The booking nurse ordered daily dressing changes and antibiotics as recommended by the emergency room physician. Over the next five days, the dressing changes were only done on two occasions. According to documentation subsequ·ently supplied by PCDC, the dressing changes were not done because the patient "was in court once, "No Showed" once, and on another occasion wasn't seen because of custody issues." 4 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 7 of 28 In addition to continuing to improve the frequency with which administrative segregation checks are occurring, PCDC needs to ensure that patients who are housed in administrative segregation are seen for medical care in a timely manner. We request that the medical staff continue to audit the administrative segregation checks and that staff conduct a quality improvement study on how to improve access to care for patients housed in administrative segregation. Through our interviews with inmates, we also identified problems with the access to mental health care. Patient-inmates with mental health concerns submit kites which are then picked up by nursing staff and referred to mental health services. The kites are then evaluated by the Mental Health Unit Supervisor who triages them. This review does not always take place in a timely manner. Patient-inmates who were interviewed complained about the long delays and the need for multiple kites in order to be seen. Furthermore, our assessment revealed that mental health staff does not respond to many patientinmates requests for care. Unlike medical kites! there is no policy that requires a response to the mental health kite. A policy and procedure needs to be created to address how mental health responds to patient-inmates' kites in an appropriate and timely manner. During Our visit!}o Robinson reviewed mental health's kites from the first 12 days of June. Her review revealed the following problems: Patient A The patient-inmate submitted a kite on 6/9/08 stating! //Could you please corne talk with me.// The patient-inrnate's chart showed no indication that the patient had been seen by mental health. The kite had been filed by mental health and not placed on the follow-up board. PatientB Mental health staff had seen the patient on 4/22/08. He submitted a kite to mental health on 6/9/08. Review of his medical record that mental health had not seen him as of 6/12/08. The kite had been filed by mental health and not placed on the follow-up board. Patient c:. The patient had been seen by mental health on 6/3/08. He submitted kites on 6/6/08 and 6/10/08 stating that he was experiencing an increasing mood swings! a decrease in sleep, and no t'toticeable difference in his appetite. Review of his medical record revealed that mental health had not seen him as of 6/12/08. The kite had been filed by mental health and not placed on the follow-up board. 5 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 8 of 28 PatientD The patient had been seen by mental health on 11/16/06 and had had suicidal ideation at that time. The patient submitted a kite on 6/3/08 stating, "meds - seizures making it impossible to control emotions - put in several kites." The patient wrote a second kite on 6/9/08 stating, "Why aren't my kites being answered. I need help badly." A review of his medical record revealed a mental health had not responded to his kites as of 6/12/08. The kites had been filed by mental health and not placed on the follow-up board. Patient E The patient submitted a kite on 6/9/08 stating, "I feel sad, depressed, too many thoughts running through my head." Review of his medical record revealed that he had been seen by mental health in the past. Mental health staff had not responded to his kite as of 6/12/08. The kite had been filed by mental health and not placed on the follow-up board. Patient F The submitted a kite on 6/1/08. Mental health staff attempted to see him on 6/90/08 but he .was on the phone. There was no indication in his medical record that staff made any further attempts to see him. The kite had been filed by mental health and not placed on the follow-up board. Patient G The triage nurse saw the patient on 5/20/08 and advised him to submit a kite to mental health for his problem. The patient submitted a kite on 6/8/08. Mental health staff reviewed the tight on 6/9/08 but had notresponded to it as of 6/12/08. The kite had been filed by mental health and not placed on the follow-up board. PatientH The patient submitted a kite on 6/5/08 stating, "depression". Mental health staff had not responded to the kite as of 6/12/08. The kite had been filed by mental health and not placed on the follow-up board. Patient I Mental health staff saw the patient on 5/31/08 and referred him to the psychiatrist. There was no indication that a psychiatrist saw the patient. The patient submitted a kite on 6/4/08 requesting mental health services. Mental health staff reviewed it on 6/11/08, but as of 6/12/08 the patient had not been seen. Receiving Screening Initial health screening is performed by a health trained correctional officer. 6 New Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 9 of 28 arrestees with any medical concerns are to be referred to the booking nurse who is on duty 24 hours per day for further evaluation. Medical staff report that the booking nurse evaluated between 30 and 60% of incoming inmates. During our first visit, staff reported that it is not uncommon, especially during busy times, for inmates with identified health concerns to be housed prior to being seen by the booking nurse. Following our first visit, we recommended that PCDe conduct a study to determine if the booking nurse is evaluating all new arrestees with medical or mental health problems. In our first report, we further concluded that given the number of daily bookings conducted at peDC, we believed that a health professional should perform the initial screening to ensure that all newly arrived arrestees are appropriately evaluated and to allow the nurse to review the electronic medical records of all incoming inmates. During our recent visit, medical administrative staff told us that they had reviewed the above issues and that they agreed that a registered nurse should screen all incoming inmates. In order to accomplish this, staff stated that they would need a minimum of an additional registered nurse position 16 hours per day. To achieve this level of staffing, PCDe would require 3.0 FTE registered nurse positions plus relief to cover vacation, educational, and sick leave. Once this staffing was in place, they would determine if it was sufficient. After reviewing the draft version of this report, Vince Goldsmith informed me that peDC . does not agree that registered nurses need to screen all incoming inmates. In my opinion, however, given the staffing and the number of daily bookings conducted at PCDe, I would expect that a health professional perform the initial screening. In our first report, we also concluded that the current system for continuing outside medications needed to be reviewed. We were concerned that some patients were not receiving essential medications in a timely manner. Our review of medical records during our recent visit revealed ongoing problems with continuity of medications. Patient 6 The patient, who has a history of diabetes, entered the PCDe on 5/12/08. She told the booking nurse that she had been taking Metformin (an oral medication for diabetes) and other medications, but had not had any for two days. Her blood sugar at that time was noted to be 260 (high). The booking nurse was unable to verify a current prescription. There was an entry in her medical record from 1/30/08, noting that her primary care physician had stated that the patient had been prescribed medications for diabetes, asthma and hyperlipidemia, including Lisinopril (an anti-hypertensive medication prescribed to many patients with diabetes to protect their kidneys). The patient's blood sugar was 249 on 5/13 and 319 on 5/14 (both high). Her medications were not ordered until 5/15. (The provider did not order the Lisinopril.) 7 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 10 of 28 Patient 7 The patient, who has a history of astluna, entered the peDe on 4/15/08. She told the booking nurse that she took medication for her asthma. The booking nurse was not able to verify a current prescription. The booking nurse did not order the medication and did not refer the patient to a provider for follow-up. (The medical record revealed that the patient had been treated for asthma in the jail in 11/07.) On 5/5/08 the patient submitted a kite stating that she was experiencing increasing shortness of breath and requested an inhaler. The triage nurse obtained an order for an inhaler from the on-call provider. The patient was not seen by a provider until 6/3. Patient 8 The patient, who has a history of hypertension for which he had been treated in th~ peDe in 11/07 and 3/08, entered the jail on 5/27/08. His blood pressure at that time was '153/115 (high). The booking nurse was unable to verify a current prescription. She referred the patient to a provider on an urgent basis. There were entries in the medical record on 5/ 28, 29 and 30 noting that the patient was a no show in clinic. It was also noted thathe refused to have his blood pressure checked. There were no refusal forms in the medical record. There was an entry from the triage nurse on 6/2 noting that the patient was requesting his medication. The nurse further noted that the patient stated he had not come to clinic because "no one woke him up." The patient was referred to see the provider on 6/3. His blood pressure at that time was 162/113. The provider ordered medication for hypertension. Patient 9 The patient, who has a history of HIV disease, entered the peDe on 5/4/08. He had been in the facility in 2006 and 2007 and had received medications. The booking nurse was not able to obtain a current prescription for medications and did not refer the patient to a provider for follow-up. The triage nurse saw the patient on 5/7 in response to a kite the patient had submitted. The nurse noted that the patient asked to see the physician because he was HIV infected and was not receiving his medications. The nurse referred the patient to the provider on an urgent basis, but he was not seen until the following day. At that time, the PA ordered the patient's medications. In our first report, we recommended that peDe conduct a quality improvement study to evaluate the timeliness with which patients receive essential medications when they first enter the jail. The study was not done, but a memorandum was issued to staff on May 16, 2008, identifying changes to the medication continuation procedure. In addition, I suggested changes to the Booking Nurse Guidelines that would help to address this issue with Mary Scott, RN, the Director of Nursing. peDe needs to monitor and evaluate whether these changes ensure that patients receive their medications in a timely manner. 8 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 11 of 28 In our first report, we also noted that there was no examination table or electrocardiogram (EKG) machine in the medical clinic in the booking area. This issue had not been resolved at the time of our second visit. Medical administrative staff informed us that they were working with custody staff to identify space in the booking area that could be used as an exam room. Staffing At the time of our visit, there were 3 nursing vacancies - 1 registered nurse position and 2 licensed practical nurse positions. We were told that the registered nurse position and one of the licensed practical nurse positions had been vacant for over one year. Medical administrative staff stated that the difficulty in filling these positions was largely due to the onerousness, length, and complexity of the hiring process. Applicants are asked very personal questions, must undergo a polygraph test, and must agree to have their neighbors interviewed.. Staff informed us that many qualified candidates do not apply or withdraw their applications upon learning about the hiring process. In 2007, out of 38 nurses who applied for positions, 8 (21 %) withdrew their applications prior to completing the process. As noted in our first report, this has been a long-standing problem. A process needs to be developed that fulfills the security needs of the facility while allowing hiring to take place in a more timely fashion. As noted above, I believe that there is a need for additional nursing positions in order to adequately staff the booking area_and to provide coverage for the medical beds in the clinic area. Furthermore, there may be a need for additional staff to adequately address patient-inmates' health complaints on weekends. To institute these changes would require at least 5 FTE registered nurse positions and 1 FTE licensed vocational nurse position. In addition, staffing needs to be increased to provide relief for vacation, education, and sick leave. Furthermore, staffing will have to be re-assessed as peDe implements a chronic disease management program and begins performing health assessments. We were informed that there are discussions about opening up two more housing units in the New Jail. If this were to occur, medical administrative staff stated that they would need an additional 1 FTE licensed practical nurse position (with a relief factor). At the time of our second VISIt, mental health staffing consisted of 6 Mental Health Program Specialists (MHP), five of whom provide 7 days per week coverage in the jail. An additional MHP has been hired and will soon start to work in the jail. The sixth MPH position works in the courts as a diversion specialist and provides part-time coverage in the jail. The clerical position noted in our first report remains open. This will place addition burdens on the MHP. In order to address the access to care problem (described 9 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 12 of 28 above) and the lack of follow-up for patients removed from suicide watch (described below), peDe's mental health program requires an increase in staffing of 2 FTE's. After reviewing the draft version of this report, Judy Snow, the mental health coordinator at PCDC, informed us that Pierce County does not agree that 2 additional staff are needed for the mental health program. The mental health services at PCDC continues to operate with only 14 hours of psychiatrist time per week with psychiatric coverage on Monday, Tuesday, Wednesday, and Thursday. The current coverage is not adequate to serve the mental health needs of the PCDC population. Long delays, up to 30 days, were found during chart review and some patients were never seen, even though there were multiple referrals to the psychiatrist (Patient I, Patient J & Patient K). However, the nurse practitioner position (ARNP) that has been vacant for over 2 year, has been filled. When the ARNP begins to work, coverage will be expanded to include 10 hours on Friday and 10 hours on Saturday. This should greatly improve the timeliness of the psychiatric coverage and the prescribing capabilities of the mental health services. The adequacy of this coverage will be evaluated on future visits. Intoxication and Withdrawal The alcohol withdrawal protocol has been revised. While the new procedure appears to adequately address the concerns raised in our prior report, we will continue to review the identification, monitoring and treatment of individuals at risk for and undergoing alcohol withdrawal to ensure that they are receiving appropriate care. During the current visit, I reviewed the records of 5 patients who were at risk for alcohol withdrawal. A problem was noted with the care of the following patient: Patient 10 The patient entered the PCDC on 5/21/08, at 2:56 a.m. The booking nurse noted that the patient had a history of alcohol withdrawal and referred him to be seen later that morning on an urgent basis. The patient was not seen by the provider until the following day, 5/22. At that time, the provider placed the patient on the alcohol withdrawal protocol and ordered Librium. There was no documentation that the patient was monitored or evaluated by medical staff until one week later. Nursing Protocols The nursing protocols have been revised to address the issue of when the nurse should contact a physician for further orders. There were a few minor concerns that I discussed with Mary Scott, the nursing supervisor. Ms. Scott stated that she would revise the protocols in order to address these concerns. In addition, the policy and procedure on 10 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 13 of 28 Nursing Assessment Protocols O-E-ll) needs to be updated to address the use of the nursing protocols. Mental Health Services The limited number of mental health staff continues to affect the ability of the mental health program to provide an appropriate level of care. A professional, dedicated staff can provide only limited care when resources are inadequate. Every inmate interviewed described the MHPs as caring and professional; however, each commented on how difficult it is to "get into" the mental health system at PCDe. Those who did receive care, expressed great appreciation for the staff and the services they provided. Kites serve as an important entry point into mental health services and as a request for follow-up care. For the most part, MHP's will see a patient one time, and then instruct them to submit a kite if they need further care. Mental health is not responding to a significant number of mental health kites (see access to care). Both Ms. Robinson and I have serious concerns with regards to this failure and believe that the mental health program must find a way to address patient's mental health needs in a timely and appropriate manner. The mental health program has made some improvements since we last visited PCDe. The Mental health Unit Supervisor is· providing twice-monthly individual clinical supervision to the MHPs at PCDC and holding a weekly staff meeting that includes a case conference. Additionally, we were advised that monitoring rounds have increased to include monthly checks of the mental health housing unit. Mental health stopped using a priority list for the psychiatrist (this prioritization was a concern addressed in our last report). Review of medical records indicated, however, that some patients are still experiencing long waits (see access to care). To enhance care, psychiatrists now refer their patients, when clinically indicated, to MHP's for scheduled follow-up checks between the psychiatric appointments. This is a practice that we strongly support. This visit revealed an additional, significant, concern - some patients are released from suicide watch with no follow-up checks from mental health. As part of the suicide prevention policy, patients discharged from suicide watch must remain on regularly scheduled follow-up assessment by menta~ health for a period of time. There is no nationally acceptable schedule for follow-up. Lindsay Hayes, a recognized expert on jail suicide prevention, recommends daily for 5 days, once a week for 2 weeks, and then once a month until release. Mental heath needs to create a policy and procedure that addresses this issue. No women were housed in the level one security housing area during this visit. In future 11 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 14 of 28 visits, we will continue to monitor all levels of inmates to insure access to an appropriate level of mental health care. The PAs continue to order psychiatric medications that the nursing staff have verified from the, community and provide the follow-up care for many inmates on psychiatric medications during their incarceration. In our first report, we requested that mental health and medical staff develop a joint policy to address this practice. We asked that the policy include guidelines, including indications as to when this was not clinically appropriate. At the time of our second visit to PCDC, this policy had not been written. Since our visit, JUdy Snow has informed us that the mental have staff have developed policies and new procedures to address problems we identified with the mental health care. We will continue to monitor these areas to ensure that the policies and procedures are implemented and adequately address our concerns. Medical Records The problems related to the electronic medical record that were noted in our prior report have not been addressed: 1. Medication administration records are not scanned into the EMR and may not be 2. 3. 4. 5. available when the patient is being evaluated. In addition, while the medical kites are scanned into the medical record, mental health kites are not scanned. Insulin does not appear on this list of medications that a patient has been ordered. Clinical information is not entered into the electronic medical record in a consistent way. Progress notes from the practitioners and the nurses can be in one of multiple sections - Synopsis, Appointments, or Correspondence (the scanned copy of the booking sheet). This makes it very difficult to review a medical record and increases the likelihood that important clinical information may be missed. Chronic illnesses are not always noted on the Problem List. In addition, mental health problems are not noted on the Problem List. Clinical documentation of patient encounters is often insufficient. Many of the notes from booking and triage are poorly written and do not contain sufficient information about a patient's condition. In addition, when nursing staff provides wound care, the nurse only notes whether the patient was seen or not seen. S/he does not document the condition of the wound or the type of care provided. PCDC needs to develop a policy and procedure for the EMR that delineates what information needs to be in the medical record and where it should be entered. Staff also thought that some simple programming changes could facilitate the resolution of some of these charting issues. 12 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 15 of 28 Billing/Co-Pay Discussions with inmate-patients did not reveal any evidence that the current co-pay system deterred individuals from accessing the health care system. We still recommend that staff perform, as part of their quality improvement program, the monitoring studies recommended by Dr. Shelton to track whether or not there was any impediment to access based upon the co-pay. . Medical Diets I spoke to the head of the kitchen staff and reviewed the monthly meal calendar and list of medical diets. The dietician from Aramark, the company that provides the meals in the jail, has certified that the meals meet nutritional requirements. If the medical staff has continued concerns, they should hire an independent nutritional consultant to review the food service. Dental Care Dental care continues to be available only one day per week. On 6/12/08, there were 40 patients on the dental priority list. According to the policy on Oral Care G-E-06), dental priorities are to be seen at the next dental clinic. Many of these patients had been on the list for over 2 months. In addition, 93 patients were on the waiting list for routine dental care. Many of these patients had been waiting over 4 to 6 months to see the dentist. The following cases are representative of some of the problems identified in our review of dental records: Patient 11 The patient was placed on the dental list 1/23/08, for evaluation of a probable dental abscess. He had not been seen as of 6/12/08. Patient 12 The patient was placed on the dental list 3/6/08, for a broken tooth. He had not been seen as of 6/12/08. Patient 13 The triage nurse saw the patient on 3/13/08. The nurse noted that he had a large cavity with significant dental decay and no signs of acute infection. The nurse referred him to the dentist as a priority appointment. The triage nurse re-evaluated the patient on 3/28/08. At that time, the patient stated that his tooth was broken, bloody, and pussy, and that it was causing a lot of pain. The nurse's assessment was that the patient had a probable abscess for which she referred him to the dentist. The patient had not been seen by the . dentist as of 4/10/08, when he was transferred to state prison. 13 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 16 of 28 Patient 14 The triage nurse saw the patient on 11/19/07, in response to a kite stating that he had "terrible pain" in his teeth. The nurse noted that the patient had "huge cavities" without any signs or symptoms of infection. The nurse placed the patient on the dental list. The triage nurse saw the patient again on 11/27/07, because he was complaining of continued dental pain. The nurse noted that the patient had multiple caries that were sensitive to temperature changes. On 1/2/08, the triage nurse saw the patient in response to a kite in which the patient stated that his teeth really hurt and he thought he might have developed an abscess. The nurse noted that the patient had been on the dental list for 45 days at that time. The triage nurse saw the patient again on 1/4/08, and noted that his left back molar and right lower molar had "huge" cavities. The nurse noted that at that time the patient had been on the dental list for 47 days. On 1/13/08, the patient submitted another kite stating that he was having excruciating pain from his teeth and difficulty eating. On 1/14/08, a nurse saw the patient and noted that he was complaining of "bad dental pain." The nurse also noted that a dental soft diet was not helpful and that he had huge cavities in two of his molars. The nurse further noted that the patient was reassured that he had no signs or symptoms of infection. On January 25, a nurse noted that the patient was complaining of pain and pus from his tooth. The nurse's assessment was that a dental abscess was probable. (The patient had been on the dental list for 68 days at that time.) The dentist finally saw the patient on 2/9/08 and extracted one of his teeth. (This was 83 days after the patient had been placed on the dental list.) The dentist saw the patient again on 2/16/08, and extracted the second tooth. (This was 90 days after the patient had been placed on the dental list.) Vince Goldsmith, the Health Care Manager, informed me that he was in the process of finalizing an agreement with a dental group to come to the jail on a daily basis for 3 weeks to clear the dental backlog. There were no plans to increase the amount of time that a dentist is available in the jail on an ongoing basis. As noted in our prior report, the current schedule is totally insufficient to meet the dental needs of the jail population. A facility the size of the peDe requires a dentist at a minimum of 3 to 5 days per week. Chronic Disease Management peDe has not developed a system for identifying and tracking patients with chronic medical problems. Dr. Balderrama stated that they were waiting for the services of a computer programmer to help them develop a system using their electronic .medical record. In addition, as noted above, many chronic illnesses are not currently noted on the problem list. Dr. Balderamma has distributed copies of the chronic care guidelines from the National 14 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 17 of 28 Commission on Correctional Health Care to the medical staff. Review of records revealed that in many cases the guidelines are not being followed. This was discussed with Dr. Balderamma. He stated that he would monitor the medical staff to ensure that they were following the guidelines. Specialty Care The jail has arrangements for providing specialized ambulatory. care for those patients who require consultations with an outside specialist. There is a system in place to track the appointments, including receipt of the consultation reports. One concern that came up during this visit is that the PCDC providers are not consistently seeing the patients and/or reviewing the consultation reports when patients return from a visit to a specialist. This was discussed with Dr. Baldarrama "ypo stated that he would address this issue. MedicationslPharmacy As discussed in our first report, PCDC has a Keep on Person (KOP) medication program in the Main Jail. Medical administrative staff has decided not to expand the program to the New Jail. Ouality Improvement As noted in our first report Continuous Quality Improvement (CQI) is the development and implementation of a procedure for reviewing the quality of care provided at an institution and, as such, is an essential component of the health care delivery system. Processes and performance must be routinely evaluated and analyzed. Based on the findings of these studies, steps must be taken to improve the outcomes if they fall short of desired goals. At the time of our prior visit, PCDC had begun to implement a CQI program. Medical staff was monitoring certain aspects of the health care program such as segregation rounds, tuberculosis skin testing, and booking refusals. Staff was also conducting death reviews. Since our last visit, Dr. Balderrama has begun to perform monthly chart reviews of at least 5% of patient-inmate health encounters with a provider. Other necessary aspects of a comprehensive CQI program, however, have not been implemented. The types of CQI studies described in·our first report have not been initiated by either the medical or mental health programs. PCDC needs to develop a more comprehensive CQI program with both outcome (i.e., the number of diabetic patients whose disease is well controlled) and process (i.e., whether patients who submit health care requests are being seen within the required time frame) oriented studies being performed. 15 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 18 of 28 Policies and Procedures The policies and procedures on Nursing Assessment Protocols (J-E-ll) and Health Records G-H-Ol) still need to be revised and updated. Mental health policy and procedures still need to be updated and a system still needs to be in place for review and approval of shared policies. REQUESTS We request that peDe provide us with updates on the following areas on October IS, 2008: 1. Revision of policy on Special Housing Revision of policy on Health Records Revision of policy on Nursing Assessment Protocols Progress of studies to evaluate need for additional weekend coverage Progress on filling vacant positions and any changes to the hiring process Nursing skills assessment training Audits of segregation check~. Study on access to care for patients in segregation Study on how long it takes for patients to be ordered critical medications upon entry into the jail 10. Progress on obtaining the services of a computer programmer to address issues with the electronic medical record 11. Revisions to Mental Health policies and procedures 12. Plan to improve Mental Health kite system 13. Development an approval protocol for involve policies involving both mental health and medical 14. Policy for follow-up checks for patients released from suicide watch 15. Policy on continuation of psychiatric medication by a PA 16. Addition of mental health questions to nursing intake questions. 2. 3. 4. 5. 6. 7. 8. 9. 16 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 19 of 28 NCCHCSTANDARDS We are using the NCCHC Standards as the framework for our opinions. Only the NCCHC Board ofAccreditation can officially determine if NCCHe standards have or have not been met. Governance and Administration J-A-O! Access to Care This standard is not being met. See the discussions of access to care, staffing, and mental health services above. J-A-02 Responsible Health Authority This standard is met. PCDC has a qualified full time Health Authority and a full-time Medical Director. J-A-03 Medical Autonomy This standard is met. Decisions and actions regarding health care services provided to inmates are the sole responsibility of qualified health care persOImel and are not compromised for security reasons. J-A-04 Administrative Meetings and Reports This standard is met. Administrative meetings are being held. Monthly statistical reports are being produced that include data on areas such as the number of bookings; medical, nursing, mental health, and dental encounters; emergency room and specialty referrals; prescriptions; the number and types of medical grievances; the results of skin testing for tuberculosis; and deaths. J-A-OS Policies and Procedures This standard is not met. See the discussion of policies and procedures above. J-A-06 Continuous Quality Improvement Program This standard is not being met. See the discussion of CQI above. J-A-07 Emergency Response Plan This standard was not evaluated. J-A-OS Communication on Special Needs Patients This standard was not evaluated during this visit. 17 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 20 of 28 J-A-09 Privacy of care This standard is met. J-A-IO Procedure in the Event of an Inmate Death This standard is met. Physician review of each death is occurring. In addition, a review. of each death is being done by a committee that includes the appropriate individuals. Issues that represent possible systems errors are being identified and addressed. In addition there is a system for notifying an inmate's family in case of emergency such as serious illness or injury. J-A-ll Grievance Mechanism for Health Complaints This standard is met. There is a mechanism in place for allowing inmate grievances and then for reviewing and responding to these grievances both on an individual and an aggregate basis to look for patterns of complaints. Managing a Safe and Healthy Environment J-B-Ol Infection Control Program This standard is being met. peDe has developed a policy for the use of the airborne isolation rooms that includes procedures and logs for monitoring the pressure. In future visits, we will review the logs to ensure that the necessary monitoring is occurring. J-B-02 Environmental Health and Safety This standard was not evaluated during this visit. J-B-03 Kitchen Sanitation and Food Handlers This standard was not evaluated during this visit. J-B-04 Ectoparasite control This standard is met. peDe has written a policy and procedure to establish active parasite (lice, scabies) control that is appropriate in that it is applied only_to infected patients, and not to all inmates upon entering jail. Qualified Health staff is used to identify infection and authorize treatment. Pregnant women are referred to a providerfor further evaluation and treatment. Personnel and Training J-C-Ol Credentialing This standard was not evaluated during this viSIt. 18 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 21 of 28 J-C-02 Clinical Performance Enhancement This standard was not evaluated during this visit. J-C-03 Continuing Education for Qualified Health Services Professionals This standard was not evaluated during this visit. J-C-04 Training for Correctional Officers This standard is being met. Mental health advised us that they have reinstated their training of peDes officers on the identification of mental health problems and suicide prevention. We will review the training records during this visit. J-C-05 Medication Administration Training This standard is met. Permanent and agency nurses receive adequate training and orientation before they are given responsibility for administering medications. J-C-06 Inmate workers This standard is met. J-C-07 Staffing Plan This standard is not being met. See the staffing discussion above. I-C-OS Health Care Liaison This standard does not apply. J-C-09 Orientation Health Staff This standard is met. Health Care Services and Support J-D-01 Pharmaceutical Operations This standard is met. The current contracted off-site pharmacy is doing well to fill the needs of the patients of peDe. There is a stock of "emergency" medications for off-hours and there is 24 hour availability from local pharmacies or the hospitai if medications are needed that are not kept on site. J-D-02 Medication Services This standard is met. J-D-03 Clinic Space, Equipment and Supplies This standard is not beinfj met. This standard requires that there is sufficient and suitable 19 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 22 of 28 space, equipment, and medical supplies for the adequate delivery of health care. At this time, the clinic area in the booking area is not adequately equipped. J~D-04 Diagnostic Services This standard is met. J-D-05 Hospital and Specialty Care .This standard is met. The jail has arrangements for providing hospital and specialized ambulatory care for medical and mental illnesses. Inmate Care and Treatment J~E-01 Information on Health Services This standard is being met. J-E-02 Receiving Screening This standard is not being met. See the discussion of receiving screening above. J-E-03 Transfer Screening This standard is not applicable. J-E-04 Health assessment This standard is not being met. Required medical and mental health assessments are not being done. J-E-05 Mental Health Screening and Evaluation This standard is not being met. A screening tool, in addition to the correctional officer's intake screen and the community reference list, needs to be utilized to assure inmates with mental health needs are referred to mental health. To satisfy this requirement, a series of approved mental health questions could be asked by nursing staff. J-E-06 Oral Care This standard is not being met. See the discussion of dental care above. J-E-07 Non-Emergency Health Care Requests and Services This standard is not being met. See the discussions of access to care, mental health services, and dental care above. In addition, we recommend that different forms or colors be used to distinguish medical from other kites. 20 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 23 of 28 J-E-08 Emergency Services This standard is being met. J-E-09 Segregated Inmates This standard is not being met. While there has been improvement in this area, required rounds in the segregation units are not consistently occurring 3 times per week. In addition, staff reported that access to care is delayed for inmates in segregation. J-E-IO Patient Escort This standard was not evaluated. J-E-ll Nursing Assessment Protocols This standard will be met when revisions to the protocols and policy are completed. J-E-12: Continuity of Care during Incarceration This standard is not being met. Continuity of essential medications for newly arrived inmates needs to be improved. See the discussion of receiving screening above. This standard is being met for mental health. Continuity care is a priority for the PCDC mental health staff. An electronic list is generated daily advising both jail mental health of new arrestees' community mental health history as well as providing a list to community mental health centers advising the center of their client arrest. Jail mental health continues verified community psychiatric medication upon admission to the jaiL J-E-13 Discharge Planning This standard is being met. Mental health begins planning for re-entry from the beginning of. incarceration and reviews the client's community resources with each inmate contact. Discharge medication is provided until a follow-up appointment is made in the community. The mental health staff works with the mentally ill client to inform them of housing options if homelessness is an issue. Discharge planning for patients with medical problems is also occurring, although in a less organized manner. Mental healh has reinstate the court diversion specialist. Health Promotion and Disease Prevention J-F-OI Health Education and Promotion This standard was not evaluated during this visit. J-F-02 Nutrition and Medical Diets 21 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 24 of 28 This standard is being met. J-F-03 Exercise This standard is being met. Discussions with staff revealed that all inmates were allowed at least the minimum number of hours for recreation. J-F-04 Personal Hygiene This standard met. peDe has changed its practice of having inmates in segregation take showers while in restraints. J-F-05 Use of Tobacco This standard is being met. peDe is a non-smoking facility. Special Needs and Services J-G-Ol Special Needs Treatment Plans This standard is not being met. Inmates identified with special needs requiring close medical supervision or multi-disciplinary care including the chronically ill, those with communicable diseases, physically handicapped, frail, elderly inmates, the terminally ill, inmates with special mental health needs, and the developmentally disabled, should have special treatment plans listed in their medical charts. The treatment plan should include instructions about diet, exercise, medication, type and frequency of diagnostic testing, and frequency of follow up for medical evaluation. These patients are being identified on a case-by-case basis by the practitioners, and appropriate medical care ordered. There is no automatic system for insuring on-going and timely follow up on a regular and routine basis for patients with identified special needs. Mental health has improved there in custody treatment plans. We will continue to review on future visits. J-G-02 Management of Chronic Disease This standard is not being met. See the discussion of chronic disease management above. J-G-03 Infinnary Care This standard is not applicable. J-G-04 Mental Health Services This standard is not being met. See the discussions of mental health services and staffing above. 22 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 25 of 28 J-G-05 Suicide Prevention Program This standard is not being met. PCDC has a system for identification, referral, evaluation, housing, monitoring, and reviewing of suicides or serious attempts. The PCDe's initial Jail Health Receiving Screen Form asks, "Suicide Attempt in Last 2 Months. Past suicide attempts are the best predictor of suicide attempts both in and out of jail. Two months is a low standard for a referral for a mental health assessment. Any inmate that has a history of in-custody suicide attempts should be referred to mental health for evaluation. Mental health's computer system will pick up inmates that have made attempts in peDe; however, it will not advise of suicide attempts made in other detention centers or mental health system outside of Pierce County mental health. Additional, there is no policy for followup check for patient discharged from suicide watch. 11 J-G-06 Intoxication and Withdrawal This standard is being met. See the discussion of intoxication and withdrawal above. J-G-07 Care of the Pregnant Inmate" This standard is being met. J-G-08 Inmates with Alcohol and Other Drug Problems This standard was not evaluated during the recent visit. J-G-09 Procedure in the Event of Sexual Assault This standard was not evaluated during the recent visit. J-G-10 Pregnancy Counseling This standard was not evaluated during the recent visit. J-G-l1 Orthotics, Prostheses, and Other Aids to Impairment The standard is being met. J-G-12 Care for the Terminally III This standard does not apply. Terminally ill patients are transferred to the local hospital. Health Records J-H-Ol Health Record Format and Contents This standard is not being met. See discussion of health records above. J-H-02 Confidentiality of Health Records and Information This standard is being met. 23 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 26 of 28 J-H-03 Access to Custody Information This standard is being met. J-H-04 Availability and Use of Health Records The standard is being met. J-H-OS Transfer of Health Records This does not apply to peDe as they have only one facility and a shared electronic health record. J-H-06 Retention of Health Records This standard is being met. Medical-Legal Issues J-I-01 Use of Restraint and Seclusion in Correctional Facilities This standard is being met. Staff advised us that restraint, as part of a treatment program, is not used for medical or mental health patients. peDe sends patients with this type of medical need to the hospital. The custody staff solely orders restraints at PCDe. The PCDe policy on Use of Restraint and Seclusion in Corrections Facility (J-I-01) has a confusing statement that needs correcting. In the statement, "Medical staff will do a health assessment no more than two hours after initial placement, ""no more" needs to be replaced with "within". In future visits, we will monitor the use of the restraint chair and the "bolts" in the DTO and DTS cells that are used by custody staff to restrain inmates. J-I-02 Emergency Psychotropic Medication This standard is not being met. The policy for involuntary medications is unclear and ambiguous. The requirement of the second practitioner's endorsement is written in a confused manner and needs clarification. This policy must also clearly spell out at what point the first dose of forced, longer-term, on-emergency medications are administered. It is likely that the practice meets the standard, but the policy needs to be clarified. J-I-03 Forensic information This standard is being met. J-I-04 End-of-life Decision Making Not applicable to peDe. J-I-05 Informed Consent 24 Case 3:95-cv-05025-FDB-JKA Document 157 Filed 08/12/2008 Page 27 of 28 This standard is being met. J-1-06 Right to Refuse Treatment This standard is not being met. The policy on Medical Refusal 0-1-06) states that patients with emergent or urgent problems who refuse care will be brought to the clinic and the practitioner will explain the consequences of refusing. If the patient continues to refuse, "s/he must sign a refusal form..." Staff stated that this often does not occur and "refused per CO" is written in the chart. As noted above, this is a particular problem for patientinmates housed in segregation. J-1-07 Medical and Other Research This standard is being met. PCDC does not use inmates for medical research. (Inmates may stay on an appropriately established research protocol if they were placed on it while in the community prior to incarceration.) Summary The following NCCHC accreditation standards are not being met: J-A-Ol Access to Care J-A-05 Policies arid Procedures J-A-06 Continuous Quality Improvement Program J-C-07 Staffing Plan J-D-03 Clinic space, Equipment and Supplies J-E-02 Receiving Screening J-E-04 Health assessment J-E-05 Mental Health Screening and Evaluation J-E-06 Oral Care J-E-07 Non-Emergency medical requests J-E-09 Segregation Inmates J-E-12: Continuity of Care J-G-Ol Special treatm.ent plans J-G-02 Management of Chronic Disease J-G-05 Suicide prevention program J-H-Ql Health Record Format and Contents J-I-02 Emergency Psychotropic Medication J-I-06 Right to Refuse Treatment The following NCCHC accreditation standards were not fully evaluated: 25 Case 3:95-cv-05025-FDB-JKA J~A-07 Document 157 Filed 08/12/2008 Emergency Plan J~A-08 Communication on Special Needs Patients J~B-02 Environmental health and safety J~B-03 Kitchen Sanitation and Food Handlers J-C-Ol Credentialing J-C-02 Clinical Performance Enhancement J-C-03 Continuing Education for Qualified Health Services Professionals J-E-IO Patient Escort J-F-Ol Health Education and Promotion J-F-02 Nutrition and Medical Diets J-G-04 Mental Health Services J-G-OB Inmates with Alcohol and Other Drug Problems J-G-09 Procedure in the Event of Sexual Assault J-G-l0 Pregnancy Counseling 26 Page 28 of 28