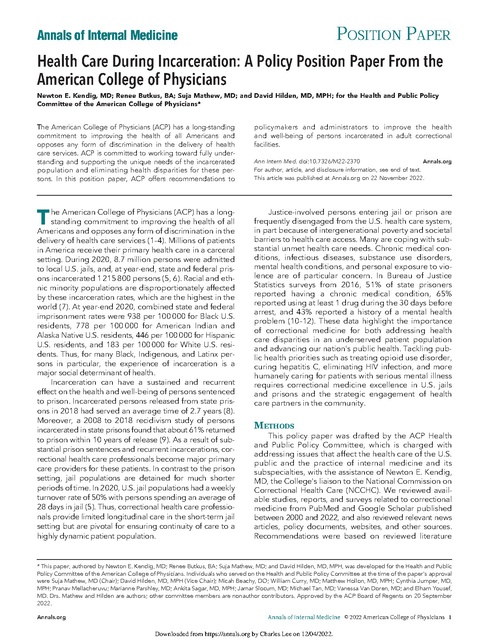
Healthcare During Incarceration-A Policy Position Paper From the American College of Physicians-Nov. 2022
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
POSITION PAPER Annals of Internal Medicine Health Care During Incarceration: A Policy Position Paper From the American College of Physicians Newton E. Kendig, MD; Renee Butkus, BA; Suja Mathew, MD; and David Hilden, MD, MPH; for the Health and Public Policy Committee of the American College of Physicians* The American College of Physicians (ACP) has a long-standing commitment to improving the health of all Americans and opposes any form of discrimination in the delivery of health care services. ACP is committed to working toward fully understanding and supporting the unique needs of the incarcerated population and eliminating health disparities for these persons. In this position paper, ACP offers recommendations to T he American College of Physicians (ACP) has a longstanding commitment to improving the health of all Americans and opposes any form of discrimination in the delivery of health care services (1–4). Millions of patients in America receive their primary health care in a carceral setting. During 2020, 8.7 million persons were admitted to local U.S. jails, and, at year-end, state and federal prisons incarcerated 1 215 800 persons (5, 6). Racial and ethnic minority populations are disproportionately affected by these incarceration rates, which are the highest in the world (7). At year-end 2020, combined state and federal imprisonment rates were 938 per 100 000 for Black U.S. residents, 778 per 100 000 for American Indian and Alaska Native U.S. residents, 446 per 100 000 for Hispanic U.S. residents, and 183 per 100 000 for White U.S. residents. Thus, for many Black, Indigenous, and Latinx persons in particular, the experience of incarceration is a major social determinant of health. Incarceration can have a sustained and recurrent effect on the health and well-being of persons sentenced to prison. Incarcerated persons released from state prisons in 2018 had served an average time of 2.7 years (8). Moreover, a 2008 to 2018 recidivism study of persons incarcerated in state prisons found that about 61% returned to prison within 10 years of release (9). As a result of substantial prison sentences and recurrent incarcerations, correctional health care professionals become major primary care providers for these patients. In contrast to the prison setting, jail populations are detained for much shorter periods of time. In 2020, U.S. jail populations had a weekly turnover rate of 50% with persons spending an average of 28 days in jail (5). Thus, correctional health care professionals provide limited longitudinal care in the short-term jail setting but are pivotal for ensuring continuity of care to a highly dynamic patient population. policymakers and administrators to improve the health and well-being of persons incarcerated in adult correctional facilities. Ann Intern Med. doi:10.7326/M22-2370 Annals.org For author, article, and disclosure information, see end of text. This article was published at Annals.org on 22 November 2022. Justice-involved persons entering jail or prison are frequently disengaged from the U.S. health care system, in part because of intergenerational poverty and societal barriers to health care access. Many are coping with substantial unmet health care needs. Chronic medical conditions, infectious diseases, substance use disorders, mental health conditions, and personal exposure to violence are of particular concern. In Bureau of Justice Statistics surveys from 2016, 51% of state prisoners reported having a chronic medical condition, 65% reported using at least 1 drug during the 30 days before arrest, and 43% reported a history of a mental health problem (10–12). These data highlight the importance of correctional medicine for both addressing health care disparities in an underserved patient population and advancing our nation's public health. Tackling public health priorities such as treating opioid use disorder, curing hepatitis C, eliminating HIV infection, and more humanely caring for patients with serious mental illness requires correctional medicine excellence in U.S. jails and prisons and the strategic engagement of health care partners in the community. METHODS This policy paper was drafted by the ACP Health and Public Policy Committee, which is charged with addressing issues that affect the health care of the U.S. public and the practice of internal medicine and its subspecialties, with the assistance of Newton E. Kendig, MD, the College's liaison to the National Commission on Correctional Health Care (NCCHC). We reviewed available studies, reports, and surveys related to correctional medicine from PubMed and Google Scholar published between 2000 and 2022, and also reviewed relevant news articles, policy documents, websites, and other sources. Recommendations were based on reviewed literature * This paper, authored by Newton E. Kendig, MD; Renee Butkus, BA; Suja Mathew, MD; and David Hilden, MD, MPH, was developed for the Health and Public Policy Committee of the American College of Physicians. Individuals who served on the Health and Public Policy Committee at the time of the paper's approval were Suja Mathew, MD (Chair); David Hilden, MD, MPH (Vice Chair); Micah Beachy, DO; William Curry, MD; Matthew Hollon, MD, MPH; Cynthia Jumper, MD, MPH; Pranav Mellacheruvu; Marianne Parshley, MD; Ankita Sagar, MD, MPH; Jamar Slocum, MD; Michael Tan, MD; Vanessa Van Doren, MD; and Elham Yousef, MD. Drs. Mathew and Hilden are authors; other committee members are nonauthor contributors. Approved by the ACP Board of Regents on 20 September 2022. Annals.org Annals of Internal Medicine © 2022 American College of Physicians 1 Downloaded from https://annals.org by Charles Lee on 12/04/2022. POSITION PAPER Health Care During Incarceration and input from ACP's Board of Governors; Board of Regents; Ethics, Professionalism and Human Rights Committee; Council of Early Career Physicians; Council of Resident/Fellow Members; Council of Student Members; and Council of Subspecialty Societies. The policy paper and related recommendations were reviewed and approved by the ACP Board of Regents on 20 September 2022. This executive summary provides a synopsis of the position paper. The full background and rationale are provided in the Appendix (available at Annals.org). POLICY RECOMMENDATIONS Correctional Medicine and Clinician Engagement Position 1: ACP recommends that U.S. jails and prisons and policymakers adopt adequately funded policies and procedures to promote the engagement of dynamic clinical care teams. a. The quality of care and ethical principles of professional engagement must be consistent with that provided to community-based patient populations. b. U.S. jails and prisons must ensure that clinicians meet credentialing requirements and are granted privileges in accordance with standards required for community-based clinicians. Administration of Correctional Medicine Position 2: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that U.S. jails and prisons provide patients timely access to necessary health care services that are based on evidence-based medicine and meet prevailing community standards. a. Local, state, and federal entities contracting to private entities for correctional health care services must provide the necessary oversight to evaluate the medical care provided to incarcerated patients to ensure quality, evidence-based medicine that meets prevailing community standards. b. U.S jails and prisons should forge strong partnerships with local and state public health and emergency response authorities including developing pandemic response plans for emerging pathogens and planning for potential natural disasters. Nutrition, Physical Activity, and Preventive Health Care Position 3: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure U.S. jails and prisons provide incarcerated persons nutritious, safe, medically appropriate, and appetizing food and beverages. Position 4: ACP recommends that policymakers and administrators ensure that U.S. jails and prisons offer incarcerated persons regular opportunities for healthy exercise as recommended by federal Physical Activity Guidelines. Position 5: ACP recommends that policymakers and administrators enact and enforce smoke-free policies in U.S. jails and prisons and provide access to smoking cessation interventions for those with tobacco use disorder. Position 6: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure incarcerated persons have access to preventive health services recommended by the U.S. Preventive Services Task Force (USPSTF) and the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP). Chronic Noncommunicable Diseases Position 7: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure incarcerated patients with chronic noncommunicable diseases are provided quality medical care in accordance with evidence-based treatment guidelines. Infectious Diseases Position 8: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that U.S. jails and prisons adopt infection prevention and control programs to promote the prevention, detection, containment, and treatment of communicable diseases. These programs should be developed in coordination and consultation with local and state public health authorities. Substance Use Disorders Position 9: ACP reaffirms its support for public policies that promote the treatment of patients with substance use disorders as an alternative to incarceration. Position 10: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures that require screening of all persons entering U.S. jails and prisons for a history of substance use disorders and provide voluntary access to evidence-based treatments for substance use disorders, including behavioral counseling services and U.S. Food and Drug Administration (FDA)-approved medications for the treatment of opioid use disorder. Behavioral Health Care Position 11: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure screening of all persons entering U.S. jails for behavioral health conditions—including suicide risk, history of serious mental illness, need for prescribed psychotropic medications, exposure to emotional or physical trauma, and co-occurring substance use disorder—and institute evidence-based policies to provide appropriate care, treatment, housing, and support to incarcerated persons with behavioral health conditions. Women's Health Care Position 12: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure U.S. jails and prisons provide comprehensive reproductive health services and trauma-informed care strategies when counseling, treating, and providing programs to incarcerated women. Position 13: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that menstruating women and transgender 2 Annals of Internal Medicine Annals.org Downloaded from https://annals.org by Charles Lee on 12/04/2022. POSITION PAPER Health Care During Incarceration men in U.S. jails and prisons have free and timely access to an adequate supply of menstrual products. Position 14: ACP recommends prohibiting the use of custody restraints on incarcerated pregnant women during labor and delivery and avoiding the use of restraints during postpartum recovery and throughout pregnancy. Position 15: ACP believes that incarcerated women should have sufficient access to evidence-based family planning and sexual health information and to pregnancy care services, and should have the ability to continue and initiate the full range of FDA-approved forms of reversible contraception. LGBTQ+ Patient Care Position 16: ACP recommends that policymakers and administrators ensure all incarcerated persons who identify as lesbian, gay, bisexual, transgender, queer, and others (LGBTQ+) be treated with dignity and respect in a correctional environment that is safe, nondiscriminatory, and gender-affirming. Aging Patients and Those Living With Disabilities and Life-Limiting Illnesses Position 17: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that aging incarcerated patients and those living with disabilities and life-limiting illnesses are treated with respect in a correctional environment that is safe, accommodates their special needs, and provides evidence-based geriatric, palliative, and end-of-life care. Immigrant Populations Position 18: ACP recommends policymakers and administrators adopt adequately funded policies and procedures to ensure immigrant detainees are treated with dignity and respect in an environment that is safe, nondiscriminatory, and culturally sensitive, including the provision of language translation and interpretation services, as needed, to promote health literacy. Position 19: ACP reaffirms its opposition to the forced separation of children from their family members held in immigrant detention facilities. ACP reaffirms its opposition to the indefinite holding of children with their parents or adult caregivers in immigrant detention facilities. Position 20: ACP supports efforts to enhance governmental oversight of health care services provided to immigrant detainees, including compliance with National Detention Standards. Community Reentry Planning Position 21: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure all U.S. jails and prisons provide reentry planning that helps ensure the continuity of health care and social services for incarcerated patients returning to the community. Position 22: ACP recommends that state Medicaid authorities adopt policies that suspend rather than terminate enrollees who become incarcerated, and support electronic, automated data exchange with correctional Annals.org systems that facilitates state Medicaid enrollment or reinstatement. ACP supports public policy discussions for expanding Medicaid coverage for incarcerated populations. CONCLUSION ACP recognizes that reducing health disparities in the quality of or access to health care for incarcerated populations will take concerted efforts by policymakers, administrators, legislative authorities, the medical community, and society as a whole. Achieving this goal will require funding and implementation of a national public policy agenda that recognizes the vital importance of correctional health care toward achieving health equity for all and promoting the public health of our communities. From School of Medicine and Health Sciences, George Washington University, Washington, DC (N.E.K.); American College of Physicians, Washington, DC (R.B.); Atlantic Health System, Morristown, New Jersey (S.M.); and Hennepin Healthcare, Minneapolis, Minnesota (D.H.). Note: Dr. Kendig's contributions to the paper are his own and are not necessarily those of the NCCHC. Financial Support: Financial support for the development of this position paper came exclusively from the ACP operating budget. Disclosures: Disclosures can be viewed at www.acponline.org/ authors/icmje/ConflictOfInterestForms.do?msNum=M22-2370. Corresponding Author: Renee Butkus, BA, American College of Physicians, 25 Massachusetts Avenue NW, Suite 700, Washington, DC 20001. Author contributions are available at Annals.org. References 1. Serchen J, Doherty R, Atiq O, et al; Health and Public Policy Committee of the American College of Physicians. A comprehensive policy framework to understand and address disparities and discrimination in health and health care: a policy paper from the American College of Physicians. Ann Intern Med. 2021;174:529-32. [PMID: 33428444] doi:10.7326/M20-7219 2. Butkus R, Rapp K, Cooney TG, et al; Health and Public Policy Committee of the American College of Physicians. Envisioning a better U.S. health care system for all: reducing barriers to care and addressing social determinants of health. Ann Intern Med. 2020;172: S50-9. [PMID: 31958803] doi:10.7326/M19-2410 3. Serchen J, Doherty R, Atiq O, et al; Health and Public Policy Committee of the American College of Physicians. Racism and health in the United States: a policy statement from the American College of Physicians. Ann Intern Med. 2020;173:556-7. [PMID: 32559145] doi:10.7326/M20-4195 4. American College of Physicians. Understanding and Addressing Disparities and Discrimination in Law Enforcement and Criminal Justice Affecting the Health of At-Risk Persons and Populations. ACP Position Paper; 2021. Accessed at www.acponline.org/acp_ policy/policies/understanding_discrimination_law_enforcement_ Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. 3 POSITION PAPER Health Care During Incarceration criminal_justice_affecting_health_at-risk_persons_populations_2021. pdf on 1 May 2022. 5. Minton TD, Zeng Z. Jail Inmates in 2020—Statistical Tables. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; December 2021. Publication no. NCJ 303308. 6. Carson EA. Prisoners in 2020—Statistical Tables. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; December 2021. Publication no. NCJ 302776. 7. Institute for Crime & Justice Policy Research. World Prison Brief data. Accessed at www.prisonstudies.org/world-prison-brief-data on 14 September 2022. 8. Kaeble D. Time Served in State Prisons, 2018. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; March 2021. Publication no. NCJ 255662. 9. Antenangeli L, Durose MR. Recidivism of Prisoners Released in 24 States in 2008: A 10-Year Follow-Up Period (2008–2018). U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; September 2021. Publication no. NCJ 256094. 10. Maruschak LM, Bronson J, Alper M. Medical Problems Reported by Prisoners: Survey of Prison Inmates, 2016. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; June 2021. Publication no. NCJ 252644. 11. Maruschak LM, Bronson J, Alper M. Alcohol and Drug Use and Treatment Reported by Prisoners: Survey of Prison Inmates, 2016. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; July 2021. Publication no. NCJ 252641. 12. Maruschak LM, Bronson J, Alper M. Indicators of Mental Health Problems Reported by Prisoners: Survey of Prison Inmates, 2016. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; June 2021. Publication no. NCJ 252643. 4 Annals of Internal Medicine Annals.org Downloaded from https://annals.org by Charles Lee on 12/04/2022. Author Contributions: Conception and design: N.E. Kendig, R. Butkus, D. Hilden. Drafting of the article: N.E. Kendig, R. Butkus, S. Mathew. Critical revision of the article for important intellectual content: N.E. Kendig, R. Butkus, D. Hilden. Final approval of the article: N.E. Kendig, R. Butkus, S. Mathew, D. Hilden. Administrative, technical, or logistic support: R. Butkus. APPENDIX Correctional Medicine and Clinician Engagement Position 1: ACP recommends that U.S. jails and prisons and policymakers adopt adequately funded policies and procedures to promote the engagement of dynamic clinical care teams. a. The quality of care and ethical principles of professional engagement must be consistent with that provided to community-based patient populations. b. U.S. jails and prisons must ensure that clinicians meet credentialing requirements and are granted privileges in accordance with standards required for community-based clinicians. ACP endorses correctional medicine excellence as an important U.S. strategy for reducing health care disparities, addressing social determinants of health, and promoting the public health of our communities. Given the frequency of complex medical conditions in this patient population, the expertise of internal medicine specialists and subspecialists plays a pivotal role in clinical care teams. Administration of Correctional Medicine Position 2: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that U.S. jails and prisons provide patients timely access to necessary health care services that are based on evidenced-based medicine and meet prevailing community standards. a. Local, state, and federal entities contracting to private entities for correctional health care services must provide the necessary oversight to evaluate the medical care provided to incarcerated patients to ensure quality, evidence-based medicine that meets prevailing community standards. b. U.S jails and prisons should forge strong partnerships with local and state public health and emergency response authorities including developing pandemic response plans for emerging pathogens and planning for potential natural disasters. The 1976 landmark Supreme Court decision, Estelle v Gamble, granted incarcerated persons a constitutional right to health care (13). The ruling affirmed that deliberate indifference to the serious medical needs of prisoners was a violation of the Eighth Amendment and served as a major impetus for prison health care reform (14). Subsequent advances in correctional health care have included the establishment of national accreditation standards, the increasing adoption of evidence-based clinical practice guidelines, and the broader engagement of academic Annals.org medicine in some settings (15, 16). Despite these notable gains, more recent court rulings, such as Brown v Plata, highlight ongoing concerns with correctional health care in some jurisdictions (17). Many factors contribute to the divergence of health care quality provided to patients experiencing incarceration. Correctional facilities are often located in remote locations with limited access to local health care services, patients may have complex medical and mental health conditions that present management challenges, financial requirements may serve as an additional barrier to health care access, staffing shortages and budgetary restraints may impact health care operations, and jails and prisons may not seek health care accreditation or have other external assessments of health care quality. These challenges highlight the need for capable correctional health care administration, sufficiently supported by the public and private sectors; broader correctional engagement with community health partners; and continued community advocacy for incarcerated persons. Specific priorities for correctional health care administrators should include ensuring health care staffing is sufficient to meet the medical and behavioral health needs of their patients; providing patients unimpeded access to necessary health care services; adopting a trauma-informed approach for all patient care; implementing evidence-based clinical practice guidelines; pursuing health care accreditation from national bodies, such as the National Commission on Correctional Health Care (NCCHC) and the American Correctional Association (ACA); providing effective contractual oversight of privatized correctional health care services; building academic partnerships to support patient care; and partnering with public health and emergency response authorities to plan for potential natural disasters and emerging pandemics. Nutrition, Physical Activity, and Preventive Health Care Position 3: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure U.S. jails and prisons provide incarcerated persons nutritious, safe, medically appropriate, and appetizing food and beverages. Providing a nutritious and appealing diet to incarcerated persons is fundamental to their personal wellbeing and important for chronic disease prevention and maintenance of a healthy weight (18–20). Incarcerated persons may have reduced opportunities to make healthy food choices. Correctional menus may be quite restrictive in their food offerings, may rely largely on processed foods, may be high in sodium and caloric content, may be lacking in fresh fruits and vegetables, and may be unappetizing. Access to nutritious food and beverages in jail and prison commissaries may also be quite limited. Barriers to providing healthier meals to incarcerated persons include budget limitations, security concerns, lack of skilled food service staff, and the adoption of menus that do not meet federal nutrition guidelines (21, 22). Correctional health care professionals can promote the health of their patients by adopting health care policies that consider access to a healthy diet a medical Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. necessity; evaluating institutional menus for nutritional adequacy through dietitian review; counseling patients on healthy dietary choices; promoting a heart-healthy diet as a standard menu option; providing medically appropriate diets for patients with temporary or permanent health conditions; providing access to labeled, healthy commissary selections; and addressing food insecurity concerns as a core component of reentry planning (23, 24). Limiting access to food and providing certain types of food should never be disciplinary in nature. Position 4: ACP recommends that policymakers and administrators ensure that U.S. jails and prisons offer incarcerated persons regular opportunities for healthy exercise as recommended by federal Physical Activity Guidelines. The Physical Activity Guidelines for Americans recommend that adults engage in regular aerobic and muscle strengthening physical activities (25). The health benefits of exercise include chronic disease prevention, assistance with weight maintenance, improvements in functional capacity, and enhanced emotional well-being. Physical exercise can also favorably impact substance use disorder treatment, a key health concern for many incarcerated persons (26). Many U.S. jails and prisons provide a wide range of indoor and outdoor supervised recreational activities. Active participation in these exercise opportunities may be affected by security constraints, such as lockdowns, or lack of patient engagement (27). Correctional health care professionals can promote physical activity opportunities for their patients by adopting health care policies that consider access to physical activity a medically necessary treatment option; counseling patients to engage in healthy exercise, particularly those patients with cardiovascular disease risk factors and obesity; and providing physical and recreational therapist services to implement physical activity recommendations for specific patient populations (28). Position 5: ACP recommends that policymakers and administrators enact and enforce smoke-free policies in U.S. jails and prisons and provide access to smoking cessation interventions for those with tobacco use disorder. Providing a smoke-free environment for incarcerated persons is a critical preventive health measure. Permitting smoking in state prisons contributes significantly to excess mortality from diseases related to smoking such as lung cancer, ischemic heart disease, and chronic obstructive lung disease (29). Smoking bans have been adopted in most state prisons and many jails, however, these policies are not universal and policy noncompliance is a concern in some jurisdictions (30). Correctional administrators should support incarcerated persons coping with tobacco smoking cessation through the provision of evidence-based interventions (31). Position 6: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure incarcerated persons have access to preventive health services recommended by the U.S. Preventive Services Task Force (USPSTF) and the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP). Annals.org Incarcerated persons should be provided equitable access to recommended immunizations, as they both protect individual patients and reduce infectious disease transmission within the correctional setting and surrounding communities. Vaccinating incarcerated persons has been an effective public health strategy for preventing and containing COVID-19, influenza, mumps, measles, and hepatitis B virus (HBV) infections (32–35). Screening for cancer types and chronic diseases, such as hypertension and diabetes, is also a recommended preventive health strategy, particularly for those incarcerated persons who are priority candidates for screening based on risk. Early detection and treatment of chronic diseases and cancer types can be life sustaining for these persons as well as a value-based intervention for the health care system. Chronic Noncommunicable Diseases Position 7: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure incarcerated patients with chronic noncommunicable diseases are provided quality medical care in accordance with evidence-based treatment guidelines. Incarcerated populations have a higher burden of certain chronic health conditions compared with the noninstitutionalized U.S. population (36). In a Bureau of Justice Statistics 2011 to 2012 survey, state and federal prisoners were about 1.5 times more likely to report ever having high blood pressure, diabetes, or asthma (37). Effectively managing these patients can be challenging within a public safety environment. Potential concerns include the institutional limitations on the frequency and timing of medication administration, security restrictions that may prohibit access to personal equipment and devices, the variable timing of meals and snack availability for patients with diabetes, patient financial requirements in some jurisdictions, and the potential lack of internal medicine and subspecialty medicine expertise (38). Conversely, the highly structured environment of U.S. prisons can provide an opportunity for closely monitoring patients with chronic diseases, including, as needed, the direct observation of medication administration. Correctional medicine can further advance chronic disease management by removing financial barriers for accessing care; adopting patient education strategies that promote health care literacy and foster shared decision making; adopting evidence-based clinical practice guidelines; deploying a physician-led multidisciplinary care team that includes nurse educators, advanced practice clinicians, and clinical pharmacists; providing the expertise of internists and subspecialists to guide care, including telehealth services; and measuring clinical outcomes to drive improvements in health care quality. Infectious Diseases Position 8: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that U.S. jails and prisons adopt infection prevention and control programs to promote Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. the prevention, detection, containment, and treatment of communicable diseases. These programs should be developed in coordination and consultation with local and state public health authorities. U.S. jails and prisons can be instrumental in detecting and treating communicable diseases in affected patient populations that may elude traditional health care networks (39, 40). CDC-recommended screening strategies for newly incarcerated persons include optout testing for HIV, hepatitis B virus (HBV), and hepatitis C virus (HCV) infections, and disease-specific screening approaches for other sexually transmitted infections and tuberculosis (41–45). In addition, newly incarcerated persons should have a thorough skin examination for communicable bacterial and ectoparasite infections. Patients diagnosed with infectious diseases on intake, or thereafter during incarceration, should have timely access to evidence-based antimicrobial regimens with follow-up assessments as clinically warranted. The effective treatment of communicable diseases, such as tuberculosis, syphilis, HIV infection, and hepatitis C, is achievable in the carceral setting and benefits both patients and the public health at-large (46–49). U.S. jails and prisons also require tailored infection prevention and control measures to help ensure the health and safety of incarcerated persons and correctional workers. Correctional administrators must, for example, develop a facility-specific exposure control plan for preventing and managing exposures to bloodborne pathogens in compliance with federal regulations; implement a tuberculosis control plan in accordance with CDC guidelines; adopt measures for safely isolating potentially contagious incarcerated persons in accordance with transmission-based precautions; and institute procedures for monitoring hand hygiene adherence and facility sanitation (50, 51). The COVID-19 pandemic, which resulted in SARSCoV-2 outbreaks in correctional settings nationwide, highlighted the vulnerability of carceral populations to communicable diseases and the potential public health consequences (52, 53). Experience from 1 large urban jail demonstrated how COVID-19 outbreaks in congregate settings could spread to the local community or be significantly controlled through recommended infection control and prevention interventions (54–56). The unprecedented impact of COVID-19 on U.S. jails and prisons further reinforces the critical importance of partnerships between correctional systems and public health authorities for implementing effective infection prevention and control programs and planning for future pandemics. Substance Use Disorders Position 9: ACP reaffirms its support for public policies that promote the treatment of patients with substance use disorders as an alternative to incarceration. Position 10: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures that require screening of all persons entering U.S. jails and prisons for a history of substance use disorders and provide voluntary access to evidenceAnnals.org based treatments for substance use disorders, including behavioral counseling services and U.S. Food and Drug Administration (FDA)-approved medications for the treatment of opioid use disorder. Substance use disorders are a chronic health condition for many incarcerated patients. In a 2016 survey of state prisoners, 40% met the criteria for having a drug use disorder and 21% met the criteria for having an alcohol use disorder in the 12 months before prison admission (11). In an earlier jail survey, 63% of sentenced jail inmates met the criteria for drug dependence or misuse (57). Key strategies for managing these patients include screening for substance use disorders on incarceration using validated tools, carefully managing clinically indicated drug withdrawal using evidence-based protocols, and providing behavioral counseling services and medical treatment options (58). An array of interventions for substance use disorders has proven efficacy, including treatments for alcohol use disorder, tobacco smoking cessation, and medications for the treatment of opioid use disorder (MOUDs) (31, 59–62). MOUDs can prevent relapse, overdose, and death, yet access to MOUDs in U.S. jails and prisons has been historically quite limited. One simulation model estimates that 4400 patient lives would be saved if MOUDs were provided to incarcerated persons when clinically indicated and continued postrelease (63). Broader provision of MOUDs in correctional settings has been limited by several factors, including regulatory and logistic hurdles, the need for more qualified primary care physicians, the cost and availability of medications, and diversion concerns. Despite these challenges, MOUDs are a medically necessary treatment intervention that should be continued on entry to jail or prison and made available to persons during incarceration when clinically indicated (64). In 2021, U.S. drug overdose deaths exceeded 100 000 over a 12-month period for the first time (65). Correctional medicine's broader commitment to substance use prevention and treatment can be instrumental in reversing this lethal trajectory. Behavioral Health Care Position 11: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure screening of all persons entering U.S. jails for behavioral health conditions—including suicide risk, history of serious mental illness, need for prescribed psychotropic medications, exposure to emotional or physical trauma, and co-occurring substance use disorder—and institute evidence-based policies to provide appropriate care, treatment, housing, and support to incarcerated persons with behavioral health conditions. In Bureau of Justice Statistics surveys, 43% of state prisoners and 44% of jail inmates self-report being told they had a mental health problem by a mental health professional (12, 66). Caring for these patients in the carceral setting should include screening for mental health conditions and co-occurring substance use disorders at intake using validated screening tools, conducting comprehensive intake mental health appraisals, and implementing individual treatment plans for patients Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. with serious mental illness that provide access to psychiatric and behavioral counseling services (58, 67). The intensity of treatment interventions for serious mental illness should match patient needs, including appropriately assigned housing in outpatient settings, residential units (such as modified therapeutic communities), or inpatient mental health units. Reentry planning should begin soon after incarceration because patients with serious mental illness often face substantial hurdles when transitioning to the community. Challenges may include linking to psychiatric services, which are often unavailable; coping with psychotic symptoms that thwart social reintegration; encountering programmatic barriers to accessing substance use disorder treatment; and experiencing discrimination when seeking housing and employment opportunities. Correctional health care professionals can provide vital support to these patients by stabilizing their psychiatric illness before release and providing cognitive–behavioral interventions that promote selfsufficiency in medication adherence and problem solving with activities of community living. Discharge planning should include patient linkages to behavioral health care clinicians, a sufficient supply of medications to bridge care, assistance with needed housing, and arrangements for essential social services. More structured reentry support is available for patients with serious mental illnesses in some jurisdictions. For example, the forensic assertive community treatment (FACT) model provides patients intensive, continuous support from a multidisciplinary team in close therapeutic coordination with the criminal justice system (68). Correctional health care professionals are also key to mitigating mental health risk management concerns such as suicide prevention, an ongoing concern for all U.S. jails and prisons. In the 2 decades preceding 2020, 6217 suicides occurred in local jails and 4523 suicides occurred in state and federal prisons (69). Most suicides occur within the first 30 days of incarceration in jails and after at least 1 year of incarceration in prisons. Recommended suicide prevention program elements include thoroughly assessing suicide risk at intake and thereafter as indicated; monitoring of high-risk persons in housing that is suicide resistant with visibility that allows constant observation; having individualized treatment plans made by qualified mental health professionals; assessing suicides and serious attempts to identify opportunities for future prevention; and annual training for all correctional staff on recognizing suicidality in incarcerated persons and responding appropriately (70). Identifying the negative psychological effects of restrictive housing or solitary confinement on incarcerated persons is also a risk management priority for correctional health care (71). Behavioral health care professionals are pivotal for evaluating persons placed in restrictive housing units and closely monitoring them for psychological distress and suicidality so that alternative housing and medically indicated treatments can be provided. Importantly, more and more U.S. jails and prisons are adopting policies that more broadly limit the placement of incarcerated persons in restrictive housing units. Correctional behavioral health professionals can be instrumental in therapeutically addressing maladaptive behaviors in these patients to facilitate their safe integration into stepdown or general housing units. Annals.org Women's Health Care Position 12: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure U.S. jails and prisons provide comprehensive reproductive health services and traumainformed care strategies when counseling, treating, and providing programs to incarcerated women. Position 13: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that menstruating women and transgender men in U.S. jails and prisons have free and timely access to an adequate supply of menstrual products. Position 14: ACP recommends prohibiting the use of custody restraints on incarcerated pregnant women during labor and delivery and avoiding the use of restraints during postpartum recovery and throughout pregnancy. Position 15: ACP believes that incarcerated women should have sufficient access to evidence-based family planning and sexual health information and to pregnancy care services, and should have the ability to continue and initiate the full range of FDA-approved forms of reversible contraception. Women residing in U.S. jails and prisons have substantial health care needs. In a survey of state prisoners from 2016, 60% reported having chronic medical conditions, 59% met criteria for having substance use disorders, and 69% reported a history of mental health problems (10–12). Even greater percentages of incarcerated women report past trauma and abuse, including intimate partner violence (72). Most incarcerated women are also of childbearing age with reproductive health needs that can be difficult to meet within the carceral setting. These observations highlight the importance of adopting correctional policies that support the genderspecific health care needs of incarcerated women (73). Fundamental to caring for women in the carceral setting is the adoption of a trauma-informed care philosophy that recognizes the high prevalence of prior trauma for justice-involved women, the potential for retraumatization during incarceration, and the impact of trauma on physical and emotional well-being (74). Adopting this philosophy is essential for building trust as a correctional health care practitioner and capably caring for incarcerated women. This includes practices such as avoiding unnecessary pelvic examinations and maintaining patient privacy from correctional officers during pelvic and breast examinations or during childbirth. Correctional medicine must also be responsive to the reproductive health needs of incarcerated women who may have had limited access to family planning services in the community and may have high rates of unplanned pregnancies (75). Correctional policies should ensure ready access to the full range of FDA-approved forms of reversible contraception. Incarcerated women who are pregnant may experience serious health-related consequences, including the lack of access to adequate obstetric care; the insufficient availability of MOUDs in pregnancy; shackling before, during, and after delivery; inability to provide breast milk to their infants; and a lack of emotional support when separated from their newborns (76). Correctional health care professionals Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. should ensure that newly incarcerated women of reproductive age are screened for pregnancy and that pregnant women have ready access to comprehensive pregnancy care services. Due to the medical risks of restraints in pregnancy, they should be prohibited during labor and delivery and avoided throughout pregnancy and postpartum recovery. If custody restraints are deemed absolutely necessary, they should be the least restrictive means that do not interfere with leg movement or ability to break a fall and should never be used during labor and delivery (77). Policies and programs to better support pregnant women and their infants should be considered, including providing one-on-one doula support of incarcerated pregnant women, before, during, and after delivery; facilitating frequent contact visits of mothers with their newborns; supporting lactation programs that provide newborn access to pumped breastmilk; proactively screening new mothers for postpartum depression; and enacting legislation that allows alternatives to incarceration for sentenced women who are pregnant or who have newborn children. primary care physicians through ongoing continuing medical education, establishing on-site or virtual clinician mentoring programs, and through LGBTQ+ consultative services, via direct patient care or telehealth. The provision of gender-affirming care to incarcerated transgender patients presents its own unique challenges. Correctional health administrators must determine the approved scope of health services for a wide variety of transition-related services for transgender patients in the midst of ongoing litigation in some jurisdictions. Comprehensive genderaffirming care, supported by evidence-based treatment guidelines, is increasingly covered by public and private payers and should also be available to incarcerated transgender patients. Treatment plans should be individualized and include, as clinically indicated, behavioral health interventions, the continuation and initiation of hormonal therapies, and access to gender-affirming surgeries and other transition-related services as warranted (82). LGBTQ+ Patient Care Position 16: ACP recommends that policymakers and administrators ensure all incarcerated persons who identify as lesbian, gay, bisexual, transgender, queer, and others (LGBTQ+) be treated with dignity and respect in a correctional environment that is safe, nondiscriminatory, and gender-affirming. Ensuring the safety, respectful treatment, and health of incarcerated LGBTQ+ persons should be a priority, supported by correctional policies, for U.S. jails and prisons (78). LGBTQ+ persons frequently face substantial health care challenges, including discrimination, stigma, and lack of access to culturally competent care. These concerns may be more acute for incarcerated LGBTQ+ persons and extend to fear for personal safety. National surveys of incarcerated populations have consistently found that LGBTQ+ persons have the highest rates of sexual victimization (79). Standards implementing the Prison Rape Elimination Act (PREA) afford some protections to incarcerated LGBTQ+ persons. These include screening newly incarcerated persons for risk for victimization based on LGBTQ+ identity, training staff on the respectful treatment of LGBTQ+ persons, and housing transgender persons based on an individualized assessment of health and safety concerns, including careful consideration of the person's own views (80). LGBTQ+ persons, however, remain vulnerable to sexual victimization during incarceration, in part because not all U.S. jails and prisons seek or achieve compliance with PREA standards. Beyond concerns for personal safety, LGBTQ+ persons have unique medical and behavioral health care needs that may not be adequately addressed during incarceration (81). Providing culturally sensitive and clinically competent care can be challenging in the correctional setting. Correctional health care practitioners may have limited personal experience caring for LGBTQ+ patients. Moreover, clinical expertise in LGBTQ+ care may not be readily available in the local community. Clinical competencies can be augmented through several strategies, including training correctional Aging Patients and Those Living With Disabilities and Life-Limiting Illnesses Position 17: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure that aging incarcerated patients and those living with disabilities and life-limiting illnesses are treated with respect in a correctional environment that is safe, accommodates their special needs, and provides evidence-based geriatric, palliative, and end-of-life care. Between 1993 and 2013, the number of state prisoners, aged 55 years or older, sentenced to 1 year or more increased 400% from 26 000 to 131 000 (83). In 2016, 38% of state and federal prisoners self-reported at least 1 disability compared with 15% in the adult U.S. general population. The most reported types of disabilities were cognitive (23%), ambulatory (12%), and vision (11%) disabilities (84). The correctional setting can pose substantial challenges for these patients with special needs. Institutional activities of daily living may include sleeping in an upper bunk bed, taking long walks to access medical care or the dining hall, physically coping with security devices, and hearing, understanding, and obeying correctional orders. Within this highly structured and restrictive environment, correctional health care professionals are instrumental in supporting persons who are aging or who are living with disabilities. Key responsibilities include the early identification of the physical and cognitive limitations of their patients; the provision of evidence-based geriatric, rehabilitative, and palliative care medicine; the determination of needed durable equipment, adaptive devices, and living accommodations; and reentry plans that address unique patient limitations and needs. Correctional health care professionals can also provide training to correctional officers to recognize normative age-associated conditions in incarcerated persons that might require correctional accommodations, vulnerability assessments, or medical evaluations (85). Annals.org Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. Correctional administrators are also responsible for the end-of-life care for patients with life-limiting illnesses. They should therefore adopt policies that require the discussion and documentation of advance directives and medical orders for life-sustaining treatment (MOLSTs) for all persons soon after their incarceration (86). Between 2001 and 2019, more than 72 000 persons died in state and federal prisons predominantly from natural causes (87). A portion of these patients died after long illnesses and were candidates for palliative care and hospice care services. Optimally, correctional systems should integrate best practices from community-based hospice care, such as adopting interdisciplinary patient care teams that include psychosocial and spiritual services; implementing evidence-based palliative care guidelines; and providing bereavement support for incarcerated persons, volunteers, and correctional staff. Correctional hospice programs may also include elements unique to the carceral setting, such as round-the-clock bedside support provided by peer caretakers, and patient contact visits with family and friends within a confined setting (88, 89). Early release from prison for medical reasons may also be an option for incarcerated patients with life-limiting illnesses or those who are otherwise incapacitated. Some eligible patients, however, are never released despite supportive policies and regulations. Barriers to early medical release include limited patient self-advocacy due to cognitive impairments and health literacy limitations, time-consuming logistic hurdles, difficulties arranging viable reentry plans, and political opposition. The advocacy of correctional health care professionals can be critical in providing timely and accurate diagnostic information that meets early medical release eligibility criteria and securing community-based medical and psychosocial services to help ensure continuity of care on release (90). Immigrant Populations Position 18: ACP recommends policymakers and administrators adopt adequately funded policies and procedures to ensure immigrant detainees are treated with dignity and respect in an environment that is safe, nondiscriminatory, and culturally sensitive, including the provision of language translation and interpretation services, as needed, to promote health literacy. Position 19: ACP reaffirms its opposition to the forced separation of children from their family members held in immigrant detention facilities. ACP reaffirms its opposition to the indefinite holding of children with their parents or adult caregivers in immigrant detention facilities. Position 20: ACP supports efforts to enhance governmental oversight of health care services provided to immigrant detainees, including compliance with National Detention Standards. Detained immigrant populations in the United States are managed by the Immigration and Customs Enforcement (ICE) Health Service Corps (IHSC). In fiscal year 2020, the IHSC provided health care to nearly 100 000 detainees in 20 IHSC-staffed facilities and provided administrative oversight to more than 169 000 Annals.org detainees in 148 non-IHSC–staffed detention facilities (91). Health care provided to detained immigrants is governed by ICE National Detention Standards (92). Caring for immigrant detainees poses many challenges for correctional medicine. Promoting the health care literacy of patients is especially difficult. Detained immigrants originate from more than 180 countries and have a wide variety of first languages and cultural backgrounds. Patient communication can be enhanced by employing a multilingual health care workforce and using language translation and interpretation services for patient encounters. International populations also have a higher prevalence of certain communicable diseases, such as tuberculosis, mumps, and measles, which are highly transmissible in congregate settings and pose substantial public health threats. Containment strategies have included universal chest radiograph screening for tuberculosis in IHSCstaffed facilities and the immunization of detainees to prevent and control mumps and measles outbreaks (35, 93, 94). COVID-19 outbreaks have also affected detained immigrant populations. Recommended containment measures have included adapting CDC infection prevention and control recommendations to the immigrant detention setting, decreasing the detainee population to reduce overcrowding and increase physical distancing, and offering COVID-19 vaccinations to all non–fully vaccinated immigrants soon after detention (56, 95). The public health importance of identifying, preventing, and containing communicable diseases in immigrant detention facilities cannot be overstated. Emerging infectious diseases are occurring globally and often first become evident in congregate settings. Behavioral health concerns affect nearly all immigrant detainees and are thus a major priority for correctional health care. Posttraumatic stress syndrome and depressive symptoms are especially prevalent due to traumatic exposures to physical, emotional, and sexual violence; family separations; and histories of extreme poverty (96, 97). Immigrant families should not be further traumatized by the forced separation of children from their parents or caregivers, or by forced family detentions that indefinitely confine adult parents or caregivers with their children (98). Providing quality health care to immigrant detainees is complicated by their frequent movement in and out of detention facilities, the seriousness of their medical and psychosocial needs, and their health literacy concerns. These challenges highlight the importance of governmental oversight of health care services provided to immigrant detainees, including ensuring compliance with National Detention Standards, expanding requirements for NCCHC accreditation, and promoting greater transparency. Community Reentry Planning Position 21: ACP recommends that policymakers and administrators adopt adequately funded policies and procedures to ensure all U.S. jails and prisons provide Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. reentry planning that helps ensure the continuity of health care and social services for incarcerated patients returning to the community. State and federal prisons released 549 600 persons in 2020 while millions more persons were released from local jails (6). Many persons leaving jail or prison have serious medical or behavioral health conditions that warrant individualized reentry plans to help ensure continuity of care. Linkages to community physicians and other clinicians are particularly important for patients with chronic noncommunicable diseases, infectious diseases, serious mental illness, and substance use disorders. Patients returning to the community often face substantial barriers to health care access that may result in preventable and sometimes serious health consequences. Reported concerns include relapse to substance use, potentially resulting in drug overdoses and death; preventable emergency department visits and hospitalizations from untreated chronic medical conditions and serious mental illnesses; lapses in antiretroviral medications and loss of viral suppression for patients with HIV infection; and acquisition of sexually transmitted infections (47, 99–104). Providing patient-centered reentry plans can help prevent these poor clinical outcomes. Reentry plans should be created soon after incarceration and regularly updated in close coordination with community practitioners and social service organizations (105). The plans should ensure patient linkages with community-based physicians and other clinicians. Key elements of the plans should include summarizing pertinent health information; conducting medication reconciliation and providing a sufficient supply of prescription medications at the time of release to bridge care; continuing prescribed MOUDs and making referrals for treatment of substance use disorder as indicated; providing overdose education and naloxone distribution; securing and updating personal identification documents; assisting with health benefit applications, such as Medicaid enrollment; and coordinating with social service organizations to secure safe housing, provide employment opportunities, and address food insecurity (106, 107). Other community transition strategies should be considered, such as referrals to “health homes” that have co-located community health care services; pairing peer navigators with incarcerated persons as part of the reentry process; staffing social workers with parole and probation offices; and providing HIV preexposure prophylaxis (PrEP) medications for at-risk persons returning to their communities (108–111). Position 22: ACP recommends that state Medicaid authorities adopt policies that suspend rather than terminate enrollees who become incarcerated, and support electronic, automated data exchange with correctional systems that facilitates state Medicaid enrollment or reinstatement. ACP supports public policy discussions for expanding Medicaid coverage for incarcerated populations. Many persons who are incarcerated are Medicaid eligible, however, federal law precludes Medicaid coverage of ambulatory health care services provided to persons in jails or prisons. Public policy initiatives can be instrumental in providing Medicaid coverage for these persons Annals.org returning to the community. State Medicaid policies that suspend rather than terminate Medicaid benefits during incarceration will facilitate Medicaid reinstatement for incarcerated persons soon after their release. Similarly, policies that promote the electronic exchange of data between correctional systems and a state's Medicaid authorities will facilitate state Medicaid enrollment or reinstatement for incarcerated persons soon after release (112). Many incarcerated persons return to their communities with limited social support while facing insurmountable barriers for accessing essential health care services. A coordinated reentry plan with engaged community partners and ready access to Medicaid benefits can be lifesaving and life changing for these persons. Web References 13. Estelle v Gamble, 429 U.S. 97 (1976). 14. Rold WJ. Thirty years after Estelle v. Gamble: a legal retrospective. J Correct Health Care. 2008;14:11-20. doi:10.1177/ 1078345807309616 15. Raimer BG, Stobo JD. Health care delivery in the Texas prison system: the role of academic medicine. JAMA. 2004;292:485-9. [PMID: 15280346] doi:10.1001/jama.292.4.485 16. Trestman RL, Ferguson W, Dickert J. Behind bars: the compelling case for academic health centers partnering with correctional facilities [Editorial]. Acad Med. 2015;90:16-19. [PMID: 25054416] doi:10.1097/ ACM.0000000000000431 17. Brown v Plata, 563 U.S. 493 (2011). 18. Juraschek SP, Kovell LC, Appel LJ, et al. Associations between dietary patterns and subclinical cardiac injury: an observational analysis from the DASH trial. Ann Intern Med. 2020;172:786-94. [PMID: 32423348] doi:10.7326/M20-0336 19. Bondolfi C, Taffe P, Augsburger A, et al. Impact of incarceration on cardiovascular disease risk factors: a systematic review and metaregression on weight and BMI change. BMJ Open. 2020;10: e039278. [PMID: 33067292] doi:10.1136/bmjopen-2020-039278 20. Clarke JG, Waring ME. Overweight, obesity, and weight change among incarcerated women. J Correct Health Care. 2012;18:285-92. [PMID: 22899812] doi:10.1177/1078345812456010 21. Center for Science in the Public Interest. Strategies to Optimize Food and Nutrition in Correctional Facilities. 2020. Accessed at www.cspinet.org/sites/default/files/2022-09/Strategies%20to% 20Optimize%20Food%20and%20Nutrition%20in%20Correctional% 20Facilities.pdf on 14 September 2022. 22. U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans. 2020-2025. 89th ed. December 2020. Accessed at DietaryGuidelines.gov on 1 May 2022. 23. Testa A, Jackson DB. Food insecurity among formerly incarcerated adults. Crim Justice Behav. 2019;46:1493-511. 24. Serchen J, Atiq O, Hilden D; Health and Public Policy Committee of the American College of Physicians. Strengthening food and nutrition security to promote public health in the United States: a position paper from the American College of Physicians. Ann Intern Med. 2022;175:1170-1. [PMID: 35759767] doi:10.7326/ M22-0390 25. U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. U.S. Department of Health and Human Services; 2018. 26. Wang D, Wang Y, Wang Y, et al. Impact of physical exercise on substance use disorders: a meta-analysis. PLoS One. 2014;9: e110728. [PMID: 25330437] doi:10.1371/journal.pone.0110728 27. Camplain R, Pinn TA, Becenti L, et al. Patterns of physical activity among women incarcerated in jail. J Correct Health Care. 2022;28:6-11. [PMID: 34846925] doi:10.1089/jchc.20.05.0041 Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. 28. Krist AH, Davidson KW, Mangione CM, et al; US Preventive Services Task Force. Behavioral counseling interventions to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force recommendation statement. JAMA. 2020;324:2069-75. [PMID: 33231670] doi:10.1001/jama.2020.21749 29. Binswanger IA, Carson EA, Krueger PM, et al. Prison tobacco control policies and deaths from smoking in United States prisons: population based retrospective analysis. BMJ. 2014;349:g4542. [PMID: 25097186] doi:10.1136/bmj.g4542 30. Kennedy SM, Davis SP, Thorne SL. Smoke-free policies in U.S. prisons and jails: a review of the literature. Nicotine Tob Res. 2015;17:629-35. [PMID: 25475088] doi:10.1093/ntr/ntu225 31. Krist AH, Davidson KW, Mangione CM, et al; US Preventive Services Task Force. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA. 2021;325:265-79. [PMID: 33464343] doi:10.1001/jama.2020.25019 32. American College of Physicians. ACP Statement on Global COVID-19 Vaccine Distribution and Allocation: On Being Ethical and Practical. 8 June 2021. Accessed at www.acponline.org/acp_ policy/policies/acp_statement_on_global_covid-19_vaccine_distribution_ and_allocation_on_being_ethical_and_practical_2021.pdf on 1 May 2022. 33. Centers for Disease Control and Prevention (CDC). Influenza outbreaks at two correctional facilities — Maine, March 2011. MMWR Morb Mortal Wkly Rep. 2012;61:229-32. [PMID: 22475851] 34. Centers for Disease Control and Prevention (CDC). Transmission of hepatitis B virus in correctional facilities—Georgia, January 1999-June 2002. MMWR Morb Mortal Wkly Rep. 2004; 53:678-81. [PMID: 15295311] 35. Leung J, Elson D, Sanders K, et al. Notes from the field: mumps in detention facilities that house detained migrants - United States, September 2018-August 2019. MMWR Morb Mortal Wkly Rep. 2019;68:749-50. [PMID: 31465321] doi:10.15585/mmwr.mm6834a4 36. Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health. 2009;63: 912-9. [PMID: 19648129] doi:10.1136/jech.2009.090662 37. Maruschak LM, Berzofsky M, Unangst J. Medical Problems of State and Federal Prisoners and Jail Inmates, 2011–12. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; February 2015. Publication no. NCJ 248491. 38. American Diabetes Association. Diabetes management in correctional institutions. Diabetes Care. 2014;37 Suppl 1:S104-11. [PMID: 24357205] doi:10.2337/dc14-S104 39. Harmon JL, Dhaliwal SK, Burghardt NO, et al. Routine screening in a California jail: effect of local policy on identification of syphilis in a high-incidence area, 2016-2017. Public Health Rep. 2020;135:57S-64S. [PMID: 32735188] doi:10.1177/0033354920928454 40. Javanbakht M, Boudov M, Anderson LJ, et al. Sexually transmitted infections among incarcerated women: findings from a decade of screening in a Los Angeles County Jail, 2002-2012. Am J Public Health. 2014;104:e103-9. [PMID: 25211762] doi:10.2105/ AJPH.2014.302186 41. MacGowan RJ. HIV Testing Implementation Guidance for Correctional Settings. Centers for Disease Control and Prevention; January 2009:1-38. CDC Stacks ID #5279. 42. Schillie S, Wester C, Osborne M, et al. CDC recommendations for hepatitis C screening among adults - United States, 2020. MMWR Recomm Rep. 2020;69:1-17. [PMID: 32271723] doi: 10.15585/mmwr.rr6902a1 43. Centers for Disease Control and Prevention (CDC), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Prevention and control of tuberculosis in correctional and detention facilities: recommendations from CDC. Endorsed by the Advisory Council for the Elimination of Tuberculosis, the National Annals.org Commission on Correctional Health Care, and the American Correctional Association. MMWR Recomm Rep. 2006;55:1-44. [PMID: 16826161] 44. Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1187. [PMID: 34292926] doi:10.15585/mmwr.rr7004a1 45. Spaulding AC, Rabeeah Z, Del Mar González-Montalvo M, et al; Rollins Investigational Team on STIs in Corrections. Prevalence and management of sexually transmitted infections in correctional settings: a systematic review. Clin Infect Dis. 2022;74:S193-217. [PMID: 35416974] doi:10.1093/cid/ciac122 46. Schmit KM, Lobato MN, Lang SG, et al. High completion rate for 12 weekly doses of isoniazid and rifapentine as treatment for latent Mycobacterium tuberculosis infection in the Federal Bureau of Prisons. J Public Health Manag Pract. 2019;25:E1-6. [PMID: 30024493] doi:10.1097/PHH.0000000000000822 47. Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: a systematic review and data synthesis. Am J Public Health. 2015;105:e5-16. [PMID: 25973818] doi:10.2105/AJPH.2015.302635 48. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-207. [PMID: 21631316] doi:10.1056/NEJMoa1009370 49. Sterling RK, Cherian R, Lewis S, et al. Treatment of HCV in the Department of Corrections in the era of oral medications. J Correct Health Care. 2018;24:127-36. [PMID: 29566611] doi:10.1177/ 1078345818762591 50. U.S. Department of Labor Occupational Safety and Health Administration. 29 CFR Part 1910.1030. Occupational Exposure to Blood Borne Pathogens: Final Rule. Fed Regist. 1991;56:64004182. 51. Bick JA. Infection control in jails and prisons. Clin Infect Dis. 2007;45:1047-55. [PMID: 17879924] doi:10.1086/521910 52. Hershow RB, Segaloff HE, Shockey AC, et al. Rapid spread of SARS-CoV-2 in a state prison after introduction by newly transferred incarcerated persons - Wisconsin, August 14-October 22, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:478-82. [PMID: 33793462] doi:10.15585/mmwr.mm7013a4 53. Hagan LM, McCormick DW, Lee C, et al. Outbreak of SARSCoV-2 B.1.617.2 (Delta) variant infections among incarcerated persons in a federal prison - Texas, July-August 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1349-54. [PMID: 34555009] doi: 10.15585/mmwr.mm7038e3 54. Reinhart E, Chen DL. Incarceration and its disseminations: COVID-19 pandemic lessons from Chicago's Cook County Jail. Health Aff (Millwood). 2020;39:1412-8. [PMID: 32496864] doi: 10.1377/hlthaff.2020.00652 55. Zawitz C, Welbel S, Ghinai I, et al. Outbreak of COVID-19 and interventions in a large jail - Cook County, IL, United States, 2020. Am J Infect Control. 2021;49:1129-35. [PMID: 33813042] doi: 10.1016/j.ajic.2021.03.020 56. Centers for Disease Control and Prevention. Guidance on Prevention and Management of Coronavirus Disease 2019 (COVID19) in Correctional and Detention Facilities. CDC; updated 3 May 2022. 57. Bronson J, Stroop J, Zimmer S, et al. Drug Use, Dependence, and Abuse Among State Prisoners and Jail Inmates, 2007-2009. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; June 2017. Publication no. NCJ 250546. 58. U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration. Screening and Assessment of Co-Occurring Disorders in the Justice System. Substance Abuse and Mental Health Services Administration; 2015. HHS publication no. PEP19-SCREEN-CODIS. 59. Witkiewitz K, Litten RZ, Leggio L. Advances in the science and treatment of alcohol use disorder. Sci Adv. 2019;5:eaax4043. [PMID: 31579824] doi:10.1126/sciadv.aax4043 Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. 60. Crowley R, Kirschner N, Dunn AS, et al; Health and Public Policy Committee of the American College of Physicians. Health and public policy to facilitate effective prevention and treatment of substance use disorders involving illicit and prescription drugs: an American College of Physicians position paper. Ann Intern Med. 2017;166:733-6. [PMID: 28346947] doi:10.7326/M16-2953 61. Moore KE, Roberts W, Reid HH, et al. Effectiveness of medication assisted treatment for opioid use in prison and jail settings: a metaanalysis and systematic review. J Subst Abuse Treat. 2019;99:32-43. [PMID: 30797392] doi:10.1016/j.jsat.2018.12.003 62. Kinlock TW, Gordon MS, Schwartz RP, et al. A randomized clinical trial of methadone maintenance for prisoners: results at 12 months postrelease. J Subst Abuse Treat. 2009;37:277-85. [PMID: 19339140] doi:10.1016/j.jsat.2009.03.002 63. Macmadu A, Goedel WC, Adams JW, et al. Estimating the impact of wide scale uptake of screening and medications for opioid use disorder in US prisons and jails. Drug Alcohol Depend. 2020;208: 107858. [PMID: 32050112] doi:10.1016/j.drugalcdep.2020.107858 64. National Commission on Correctional Health Care (NCCHC). Opioid Use Disorder Treatment in Correctional Settings (2021), Position Statement. Accessed at www.ncchc.org/opioid-use-disorder-treatmentin-correctional-settings-2021 on 14 September 2022. 65. Centers for Disease Control and Prevention. Provisional Drug Overdose Death Counts. 2021. Accessed at www.cdc.gov/nchs/ nvss/vsrr/drug-overdose-data.htm on 1 May 2022. 66. Bronson J, Berzofsky MB. Indicators of Mental Health Problems Reported by Prisoners and Jail Inmates, 2011-12. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; June 2017. Publication no. NCJ 250612. 67. Blandford AM, Osher FC, McLeod M, et al. Guidelines for the Successful Transition of Individuals with Behavioral Health Disorders from Jail and Prison. 2nd ed. Policy Research Associates; 2019. 68. Galletta E, Fagan TJ, Shapiro D, et al. Societal reentry of prison inmates with mental illness: obstacles, programs, and best practices. J Correct Health Care. 2021;27:58-65. [PMID: 34232765] doi:10.1089/jchc.19.04.0032 69. Carson EA. Suicide in Local Jails and State and Federal Prisons, 2000–2019—Statistical Tables. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; October 2021. Publication no. NCJ 300731. 70. Cramer RJ, Wechsler HJ, Miller SL, et al. Suicide prevention in correctional settings: current standards and recommendations for research, prevention, and training. J Correct Health Care. 2017;23: 313-28. [PMID: 28656789] doi:10.1177/1078345817716162 71. Luigi M, Dellazizzo L, Giguère CÉ, et al. Shedding light on “the hole”: a systematic review and meta-analysis on adverse psychological effects and mortality following solitary confinement in correctional settings. Front Psychiatry. 2020;11:840. [PMID: 32973582] doi:10.3389/ fpsyt.2020.00840 72. Lynch SM, Fritch A, Heath NM. Looking beneath the surface: the nature of incarcerated women's experiences of interpersonal violence, treatment needs, and mental health. Fem Criminol. 2012;7:381-400. 73. Daniel H, Erickson SM, Bornstein SS, et al; Health and Public Policy Committee of the American College of Physicians. Women's health policy in the United States: an American College of Physicians position paper. Ann Intern Med. 2018;168:874-5. [PMID: 29809243] doi:10.7326/M17-3344 74. Harner H, Burgess AW. Using a trauma-informed framework to care for incarcerated women. J Obstet Gynecol Neonatal Nurs. 2011;40: 469-75. [PMID: 21894637] doi:10.1111/j.1552-6909.2011.01259.x 75. Clarke JG, Hebert MR, Rosengard C, et al. Reproductive health care and family planning needs among incarcerated women. Am J Public Health. 2006;96:834-9. [PMID: 16571701] doi:10.2105/ AJPH.2004.060236 76. Sufrin C, Kramer CT, Terplan M, et al. Availability of medications for the treatment of opioid use disorder among pregnant and postpartum Annals.org individuals in US jails. JAMA Netw Open. 2022;5:e2144369. [PMID: 35050354] doi:10.1001/jamanetworkopen.2021.44369 77. National Commission on Correctional Health Care (NCCHC). Nonuse of Restraints for Pregnant and Postpartum Incarcerated Individuals (2020). Position Statement. Accessed at www.ncchc.org/ nonuse-of-restraints-for-pregnant-and-postpartum-incarceratedindividuals-2020 on 14 September 2022. 78. Daniel H, Butkus R; Health and Public Policy Committee of American College of Physicians. Lesbian, gay, bisexual, and transgender health disparities: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;163:135-7. [PMID: 25961598] doi:10.7326/M142482 79. Beck AJ, Berzofsky M, Caspar R, et al. Sexual victimization in prison and jails reported by inmates, 2011-12. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; May 2013. Publication no. NCJ 241399. 80. U.S. Department of Justice. 28 CFR Part 115. National Standards to Prevent, Detect, and Respond to Prison Rape. Fed Regist. 2012;77:37106. 81. Bacak V, Thurman K, Eyer K, et al. Incarceration as a health determinant for sexual orientation and gender minority persons. Am J Public Health. 2018;108:994-9. [PMID: 29927654] doi: 10.2105/AJPH.2018.304500 82. Kendig NE, Cubitt A, Moss A, et al. Developing correctional policy, practice, and clinical care considerations for incarcerated transgender patients through collaborative stakeholder engagement. J Correct Health Care. 2019;25:277-86. [PMID: 31242806] doi:10.1177/ 1078345819857113 83. Carson EA, Sabol WJ. Aging of the State Prison Population, 1993–2013. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; May 2016. Publication no. NCJ 248766. 84. Maruschak LM, Bronson J. Disabilities Reported by Prisoners: Survey of Prison Inmates, 2016. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; March 2021. Publication no. NCJ 252642. 85. Williams BA, Stern MF, Mellow J, et al. Aging in correctional custody: setting a policy agenda for older prisoner health care. Am J Public Health. 2012;102:1475-81. [PMID: 22698042] doi:10.2105/ AJPH.2012.300704 86. National Commission on Correctional Health Care (NCCHC). Medical Orders for Life-Sustaining Treatment (2022). Position Statement. Accessed at www.ncchc.org/medical-orders-for-lifesustaining-treatment-2022-2 on 14 September 2022. 87. Carson EA. Mortality in State and Federal Prisons, 2001–2019— Statistical Tables. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; December 2021. Publication no. NCJ 300953. 88. Linder JF, Meyers FJ. Palliative care for prison inmates: “don't let me die in prison”. JAMA. 2007;298:894-901. [PMID: 17712073] doi:10.1001/jama.298.8.894 89. Prost SG, Holland MM, Hoffmann HC, et al. Characteristics of hospice and palliative care programs in US prisons: an update and 5-year reflection. Am J Hosp Palliat Care. 2020;37:514-20. [PMID: 31808349] doi:10.1177/1049909119893090 90. Williams BA, Sudore RL, Greifinger R, et al. Balancing punishment and compassion for seriously ill prisoners. Ann Intern Med. 2011;155:122-6. [PMID: 21628351] doi:10.7326/0003-4819155-2-201107190-00348 91. U.S. Immigration and Customs Enforcement. The U.S. Immigration and Customs Enforcement (ICE) Health Service Corps (IHSC) Annual Report, Fiscal Year 2020. ICE; 2020. Accessed at www.ice.gov/news/releases/ice-releases-first-health-service-corpsannual-report on 1 May 2022. 92. U.S. Immigration and Customs Enforcement. ICE National Detention Standards. 9 November 2021. Accessed at www.ice.gov/ factsheets/facilities-pbnds on 1 May 2022. Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022. 93. Boardman NJ, Moore T, Freiman J, et al. Pulmonary tuberculosis disease among immigrant detainees: rapid disease detection, high prevalence of asymptomatic disease, and implications for tuberculosis prevention. Clin Infect Dis. 2021;73:115-20. [PMID: 32296830] doi: 10.1093/cid/ciaa434 94. Venkat H, Kassem AM, Su CP, et al; Measles Investigation Team. Notes from the field: measles outbreak at a United States Immigration and Customs Enforcement facility - Arizona, May-June 2016. MMWR Morb Mortal Wkly Rep. 2017;66:543-4. [PMID: 28542125] doi:10.15585/mmwr.mm6620a5 95. U.S. Immigration and Customs Enforcement. Immigration and Customs Enforcement (ICE), Enforcement and Removal Operations (ERO) COVID-19 Pandemic Response Requirements. Version 8.0. ICE; 4 April 2022. Accessed at www.ice.gov/coronavirus/prr on 1 May 2022. 96. Ornelas IJ, Yamanis TJ, Ruiz RA. The health of undocumented Latinx immigrants: what we know and future directions. Annu Rev Public Health. 2020;41:289-308. [PMID: 32237989] doi:10.1146/ annurev-publhealth-040119-094211 97. Ornelas IJ, Perreira KM. The role of migration in the development of depressive symptoms among Latino immigrant parents in the USA. Soc Sci Med. 2011;73:1169-77. [PMID: 21908089] doi:10.1016/j.socscimed.2011.07.002 98. American College of Physicians. The Health Impact of Family Detentions in Immigration Cases. ACP Policy Statement. 3 July 2018. Accessed at www.acponline.org/acp_policy/policies/family_ detention_position_statement_2018.pdf on 1 May 2022. 99. Binswanger IA, Stern MF, Deyo RA, et al. Release from prison— a high risk of death for former inmates. N Engl J Med. 2007;356: 157-65. [PMID: 17215533] doi:10.1056/NEJMsa064115 100. Ranapurwala SI, Shanahan ME, Alexandridis AA, et al. Opioid overdose mortality among former North Carolina inmates: 20002015. Am J Public Health. 2018;108:1207-13. [PMID: 30024795] doi:10.2105/AJPH.2018.304514 101. Wang EA, Wang Y, Krumholz HM. A high risk of hospitalization following release from correctional facilities in Medicare beneficiaries: a retrospective matched cohort study, 2002 to 2010. JAMA Intern Med. 2013;173:1621-8. [PMID: 23877707] doi:10.1001/jamainternmed.2013.9008 102. Frank JW, Linder JA, Becker WC, et al. Increased hospital and emergency department utilization by individuals with recent criminal justice involvement: results of a national survey. J Gen Intern Med. 2014;29:1226-33. [PMID: 24817280] doi:10.1007/ s11606-014-2877-y Annals.org 103. Baillargeon J, Giordano TP, Rich JD, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301:848-57. [PMID: 19244192] doi:10.1001/jama.2009.202 104. Wiehe SE, Rosenman MB, Aalsma MC, et al. Epidemiology of sexually transmitted infections among offenders following arrest or incarceration. Am J Public Health. 2015;105:e26-32. [PMID: 26469659] doi:10.2105/AJPH.2015.302852 105. U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration. Guidelines for Successful Transition of People with Mental or Substance Use Disorders from Jail or Prison: Implementation Guide. Substance Abuse and Mental Health Services Administration; 2017. SMA164998. 106. Wenger LD, Showalter D, Lambdin B, et al. Overdose education and naloxone distribution in the San Francisco County Jail. J Correct Health Care. 2019;25:394-404. [PMID: 31672075] doi:10.1177/1078345819882771 107. Leung TC, Colyer S, Zehireva S. An outcome study on the Naloxone Education/Dispensing Program for departure patients at Cermak Health Services of Cook County. J Correct Health Care. 2021;27:11-13. [PMID: 34232768] doi:10.1089/jchc.19.02.0013 108. Wang EA, Hong CS, Shavit S, et al. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012;102:e22-9. [PMID: 22813476] doi: 10.2105/AJPH.2012.300894 109. Shavit S, Aminawung JA, Birnbaum N, et al. Transitions clinic network: challenges and lessons in primary care for people released from prison. Health Aff (Millwood). 2017;36:1006-15. [PMID: 28583958] doi:10.1377/hlthaff.2017.0089 110. Cunningham WE, Weiss RE, Nakazono T, et al. Effectiveness of a peer navigation intervention to sustain viral suppression among HIV-positive men and transgender women released from jail: the LINK LA randomized clinical trial. JAMA Intern Med. 2018;178:54253. [PMID: 29532059] doi:10.1001/jamainternmed.2018.0150 111. Woznica DM, Fernando NB, Bonomo EJ, et al. Interventions to improve HIV care continuum outcomes among individuals released from prison or jail: systematic literature review. J Acquir Immune Defic Syndr. 2021;86:271-85. [PMID: 33079904] doi: 10.1097/QAI.0000000000002523 112. The Commonwealth Fund. Medicaid's Evolving Role in Advancing the Health of People Involved in the Justice System. Issue Brief. 18 November 2020. Accessed at www.commonwealthfund.org/publications/ issue-briefs/2020/nov/medicaid-role-health-people-involved-justice-system on 1 May 2022. Annals of Internal Medicine Downloaded from https://annals.org by Charles Lee on 12/04/2022.