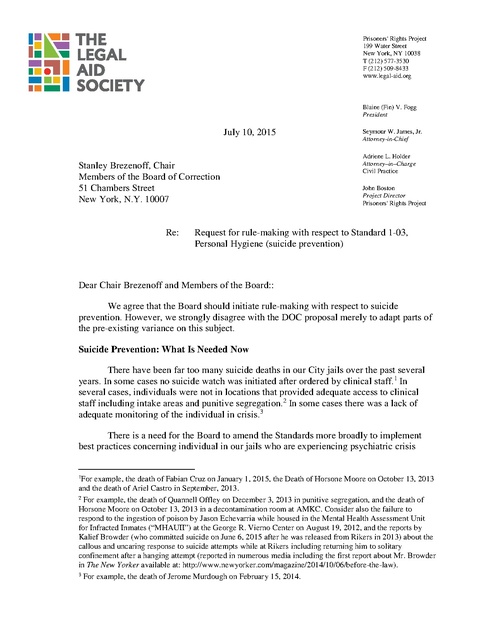
Letter to BOC, Request for rule-making with respect to suicide prevention, Prisoners' Rights Project, 2015
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
Prisoners' Rights Project 199 Water Street New York, NY 10038 T (212) 577-3530 F (212) 509-8433 www.legal-aid.org Blaine (Fin) V. Fogg President July 10, 2015 Stanley Brezenoff, Chair Members of the Board of Correction 51 Chambers Street New York, N.Y. 10007 Re: Seymour W. James, Jr. Attorney-in-Chief Adriene L. Holder Attorney–in–Charge Civil Practice John Boston Project Director Prisoners' Rights Project Request for rule-making with respect to Standard 1-03, Personal Hygiene (suicide prevention) Dear Chair Brezenoff and Members of the Board:: We agree that the Board should initiate rule-making with respect to suicide prevention. However, we strongly disagree with the DOC proposal merely to adapt parts of the pre-existing variance on this subject. Suicide Prevention: What Is Needed Now There have been far too many suicide deaths in our City jails over the past several years. In some cases no suicide watch was initiated after ordered by clinical staff.1 In several cases, individuals were not in locations that provided adequate access to clinical staff including intake areas and punitive segregation.2 In some cases there was a lack of adequate monitoring of the individual in crisis.3 There is a need for the Board to amend the Standards more broadly to implement best practices concerning individual in our jails who are experiencing psychiatric crisis 1 For example, the death of Fabian Cruz on January 1, 2015, the Death of Horsone Moore on October 13, 2013 and the death of Ariel Castro in September, 2013. 2 For example, the death of Quannell Offley on December 3, 2013 in punitive segregation, and the death of Horsone Moore on October 13, 2013 in a decontamination room at AMKC. Consider also the failure to respond to the ingestion of poison by Jason Echevarria while housed in the Mental Health Assessment Unit for Infracted Inmates (“MHAUII”) at the George R. Vierno Center on August 19, 2012, and the reports by Kalief Browder (who committed suicide on June 6, 2015 after he was released from Rikers in 2013) about the callous and uncaring response to suicide attempts while at Rikers including returning him to solitary confinement after a hanging attempt (reported in numerous media including the first report about Mr. Browder in The New Yorker available at: http://www.newyorker.com/magazine/2014/10/06/before-the-law). 3 For example, the death of Jerome Murdough on February 15, 2014. _______ Stanley Brezenoff, Chair, Board of Correction Members of the Board of Correction Page 2 including suicidality. The current DOC proposal lacks the necessary substance and consideration that this topic requires. Limiting hygiene items and providing special clothing and bedding to persons on suicide watch are not sufficient. If the Board is going to take up the question of suicide prevention, it should do so much more broadly. The Consensus Project of the Council of State Governments identifies eight essential steps for an institutional suicide prevention plan: 1. Training of correctional staff, who are the primary observers of behavior when mental health staff are unavailable; 2. Immediate screening at intake and ongoing assessment; 3. Communication between transport officer and corrections officer, facility staff and mental health staff, and facility staff and inmate; 4. Placement in housing appropriate to the situation, emphasizing use of general population settings instead of isolation; 5. Establishing appropriate levels of supervision, including close and constant observation; 6. Rapid and correct response to suicide attempts; 7. Reporting of suicide attempts throughout the chain of command; and 8. Follow-up and administrative review, including attending to the effects of critical incidents on staff stress. The problem of suicide prevention is for the most part not adequately addressed in the existing Standards in light of current knowledge. The Mental Health Minimum Standards (MH Standards) require that DOHMH establish a mental health program that provides for suicide prevention. MH Standard § 2-01(b). Training of correction and clinical staff on suicide prevention is required. MH Standard § 2-02(c)(vii). There is a required program of “observation aides.”4 MH Standard § 2-02(d). And MH Standard § 2-04 designates that appropriate treatment environments which reduce the risk of suicide need to be available. This section of the MH Minimum Standards includes language about special housing, appropriate space, trained steady staff and individualized treatment planning. However, although it mentions “facilities appropriate for the observation, evaluation and treatment of acute psychiatric episodes,” it does not make a connection to suicide watch or suicide prevention. MH Standards § 2-04(c)(4).5 4 Current best practices emphasize that incarcerated persons should not be used as a substitute for staff monitoring. (Standards for Health Services in Jails, National Commission on Correctional Health Care, 2008, p. 102) Observation aides should only be used in addition to trained staff. 5 Research indicates that suicidal individuals should be housed in general population, mental health units or infirmary in the closest proximity to clinical staff. The intention is to maximize the ability of staff to interact with the individual and minimize isolation and confinement. Correction Officers should be trained on how to interact with incarcerated individuals who are suicidal. Emphasis should be placed on listening to the person, _______ Stanley Brezenoff, Chair, Board of Correction Members of the Board of Correction Page 3 The language of the MH Standards should be improved to require suicide screening at intake, and periodic assessments (at least every 90 days).6 The Standards should reflect requirements for communication channels between correction staff and clinical staff, including through the chain of command to some designated Central Office level. The requirements for levels of suicide supervision (periodic watch, constant watch), and requirements of clinical staff oversight at each level should be spelled out.7 These are some of the steps that would bring the Standards in line with the current best practices. We do not propose specific language or other detail at this early point because more thought and research will be required. However, we urge the Board to commence rulemaking on the subject of suicide prevention as a whole, and we will certainly contribute to such an effort. The Department’s Proposed Amendments DOC’s proposed amendments are grossly inadequate even in their own terms—in part because they omit some of the essential conditions the Board imposed in granting the variance in the first place. DOC’s proposed amendments to the Standards would authorize DOC to require individuals on suicide watch to wear suicide resistant smocks and remaining with him or her if there is a change in behavior or indication of immediate danger and maintaining constant contact with the individual. (Hayes, Lindsay M., “Guide to Developing and Revising Suicide Prevention Protocols Within Jails and Prisons.” National Center on Institutions and Alternatives, 2011, p. 1-2, http://www.ncianet.org/services/suicide-prevention-in-custody/publications/guide-to-developing-and-revisingsuicide-prevention-protocols-within-jails-and-prisons/) 6 An initial screening is not sufficient. “The intake screening process should be viewed as similar to taking your temperature, it can identify a current fever, but not a future cold. Therefore, following the intake screening process, should any staff hear an inmate verbalize a desire or intent to commit suicide, observe an inmate engaging in any self-harm, or otherwise believe an inmate is at risk for suicide, a procedure should be in place that requires staff to take immediate action to ensure that the individual is constantly observed until appropriate medical, mental health, and/or supervisory assistance is obtained.” Hayes, Lindsay M., “Guide to Developing and Revising Suicide Prevention Protocols Within Jails and Prisons.” National Center on Institutions and Alternatives, 2011, p.1 available at: http://www.ncianet.org/services/suicide-prevention-incustody/publications/guide-to-developing-and-revising-suicide-prevention-protocols-within-jails-and-prisons/. See also, Standards for Health Services in Jails, National Commission on Correctional Health Care, 2008, p. 102 (Patients are reassessed regularly to identify any change in condition indicating need for a change in supervision level or required transfer or commitment. The evaluation includes procedures for periodic followup assessment after the individual is discharged from suicide precautions); and STIPULATED SETTLEMENT AGREEMENT AND ORDER CONCERNING SUICIDE PREVENTION AND RELATED MENTAL HEALTH ISSUES, U.S. v. Erie County, NY, 09-CV-0849 (W.D.N.Y 2010) at p. 5 (requiring reassessment post sentencing), available at: http://www.justice.gov/crt/about/spl/documents/erie_suicide_mh_settlement_06-18-2010.pdf. 7 An effective policy would require that mental health professionals have daily interactions with suicidal individuals as well as that they complete daily evaluations of the person’s behavior and disposition. Furthermore, the policy should include an individualized plan for each person placed on suicide watch. Hayes, Lindsay M., “Guide to Developing and Revising Suicide Prevention Protocols Within Jails and Prisons.” National Center on Institutions and Alternatives, 2011, p 3 available at: http://www.ncianet.org/services/suicide-prevention-in-custody/publications/guide-to-developing-and-revisingsuicide-prevention-protocols-within-jails-and-prisons/) _______ Stanley Brezenoff, Chair, Board of Correction Members of the Board of Correction Page 4 undergarments inside their housing area and uniforms outside except for court, and substitute suicide resistant bedding. However, according to the Board website, the above variances from §1-03(g) and (i) were granted starting in September 2003 subject to conditions. The conditions are as follows, with the bold lettering indicating whether or not the DOC petition includes the condition that was in place for the grant of the variance: • • • • • • Only mental health providers may place a prisoner on suicide watch and require the use of a suicide smock and bedding; The petition does not indicate that only mental health providers may place an incarcerated person on suicide watch. The language “with the approval of a mental health provider” does not address how the prisoner was placed on suicide watch or by whom. Officers assigned to areas where prisoners are on suicide watch must make frequent, irregular observations of these prisoners (at least four per hour). The petition does not require irregular observations at a rate of at least 4 per hour.8 Unless inappropriate for compelling security or medical reasons, prisoners on suicide watch should be housed in dormitories. Dormitory prisoners may be required to wear smocks only in dormitories where all other prisoners are clothed in suicide smocks. The petition is silent as to location (dormitories) and is silent as to “all prisoners” in like circumstances. Unless prohibited in writing by the provider, prisoners on suicide watch must be permitted personal hygiene items and personal items, including reading materials and photographs. The petition is silent about personal hygiene items, personal items, reading materials and photographs. Prisoners wearing suicide smocks shall be provided with daily exchanges of clean smocks and undergarments. Disposable undergarments will be provided with a uniform whenever prisoners leave their cell. The petition includes this condition. Suicide watch prisoners shall be permitted to wear civilian clothing when inside a court room for trial. The petition includes this condition. All of the conditions imposed by the BOC for the grant of the variance are reasonable and in line with suicide prevention protocols. Yet DOC left out the necessity that clinical staff be involved in the decision-making about whether to implement a suicide watch and what deprivations are required for maintaining safety of a particular individual. 8 Checking four times per hour may not be in line with current standards. The National Center on Institutions and Alternatives (NCIA) recommends two levels of suicide watch, close observation and constant observation. Close observation is for individuals on suicide watch who have suicidal tendencies or a past history of self-destructive behavior. These inmates should be observed at staggered intervals not to exceed ten minutes. Constant observation is for inmates who are actively suicidal and need to be continuously monitored. Moreover, the NCIA indicates that it is essential that the monitoring is completed by trained individuals. See Hayes, Lindsay M., “Guide to Developing and Revising Suicide Prevention Protocols Within Jails and Prisons.” National Center on Institutions and Alternatives, 2011, p. 1-2, p. 3, available at: http://www.ncianet.org/services/suicide-prevention-in-custody/publications/guide-to-developing-and-revisingsuicide-prevention-protocols-within-jails-and-prisons/) _______ Stanley Brezenoff, Chair, Board of Correction Members of the Board of Correction Page 5 The Standards must incorporate the need for mental health staff to be involved in determining the deprivations and in assuring that the smallest amount of deprivations are in place that will maintain the safety of the individual. Best practices include increasing access to amenities as quickly as possible – including personal items, regular clothing and regular bedding, and such judgment can only properly be made by mental health professionals.9 Equally disturbing is the fact that there is no requirement in the rulemaking petition that the location of suicide watches should be in a location where “all” are held under similar circumstances as is required by the Board in the existing variance condition. Suicide prevention smocks and bedding are methods of dealing with a crisis, they are not pleasant conditions and should not be public (and thereby a possible source of ridicule by others). Someone in crisis and required to wear a suicide prevention smock should not be housed in an area where others are able unnecessarily to observe their experience.10 For these reasons, at a minimum the conditions promulgated initially by the Board should be included in any conversion of this variance to an amendment. There should also be some enhancement of those conditions. Not only should there be specified areas for persons on suicide watch, it should be specified that the area should have suicide proof fixtures.11 Suicide watch should also be held in a clinical setting that provides a high-level of care and presence of clinical staff such as in the CAPS and PACE units. This need is a real and present one. At an earlier Board meeting Dr. Venters indicated that suicide watches would occur in the Restricted Housing Units (RHU). The RHU, where individuals with mental illness who are not deemed to be in need of the CAPS level of care, serve punitive segregation time, should never have someone on suicide watch. If an individual is in a 9 See Standards for Health Services in Jails, National Commission on Correctional Health Care, 2008, p. 102 (Patients are reassessed regularly to identify any change in condition indicating need for a change in supervision level or required transfer or commitment. The evaluation includes procedures for periodic followup assessment after the individual is discharged from suicide precautions); Hayes, Lindsay M., “Guide to Developing and Revising Suicide Prevention Protocols Within Jails and Prisons.” National Center on Institutions and Alternatives, 2011, p.3 available at: http://www.ncianet.org/services/suicide-prevention-incustody/publications/guide-to-developing-and-revising-suicide-prevention-protocols-within-jails-and-prisons/ (“To every extent possible, suicidal inmates should be housed in the general population, mental health unit, or medical infirmary, located close to staff. Further, removal of an inmate’s clothing (excluding belts and shoelaces) and the use of physical restraints (e.g., restraint chairs or boards, leather straps, handcuffs, straitjackets) should be avoided whenever possible, and used only as a last resort when the inmate is physically engaging in self-destructive behavior. Housing assignments should be based on the ability to maximize staff interaction with the inmate, not on decisions that heighten depersonalizing aspects of confinement.”). 10 Despite the current Board condition on the location of suicide watches, the current practice does not require that suicide watches be only conducted in specified areas in our jails. 11 Current research suggest that incarcerated persons who require suicide watch should be housed in suicideresistant housing with clear visibility and free of protrusions that would enable hanging. Ideally, the cell should also be free of devices or objects that could serve as an anchor for hanging. Hayes, Lindsay M., “Guide to Developing and Revising Suicide Prevention Protocols Within Jails and Prisons.” National Center on Institutions and Alternatives, 2011, p.3 available at: http://www.ncianet.org/services/suicide-prevention-incustody/publications/guide-to-developing-and-revising-suicide-prevention-protocols-within-jails-andprisons/) _______ Stanley Brezenoff, Chair, Board of Correction Members of the Board of Correction Page 6 psychiatric crisis – requiring implementation of a suicide watch – they do require a high level of care, removal from a restricted housing area such as RHU, and placement in a designated area in close proximity to clinical staff. As we stated initially, reform of suicide prevention practices should not be limited to tinkering with the existing variance and conditions; it should be approached from scratch with the benefit of all that has been learned in the more than two decades since the MH Minimum Standards were promulgated. Very Truly Yours, SARAH KERR Staff Attorney JOHN BOSTON Director The Legal Aid Society Prisoners’ Rights Project (212) 577-3530 ELLEN YAROSHEFSKY Clinical Professor Director-Youth Justice Clinic Cardozo School of Law 55 Fifth Ave New York, NY 10003 (212) 790-0386 JENNIFER J. PARISH Director of Criminal Justice Advocacy Mental Health Project Urban Justice Center 40 Rector Street, 9th Floor New York, NY 10006 (646) 602-5644 LISA SCHREIBERSDORF Executive Director Brooklyn Defender Services 177 Livingston Street, 7th Fl. Brooklyn, NY 11201 NYC JAILS ACTION COALITION c/o Urban Justice Center 40 Rector Street, 9th Floor New York, NY 10006 www.nycjac.org MIK KINKEAD Director of Prisoner Justice Project Sylvia Rivera Law Project 147 West 24th St., 5th floor New York, NY 10011 BETH HAROULES Senior Staff Attorney New York Civil Liberties Union 125 Broad St. New York, NY 10004 (212) 607-3325