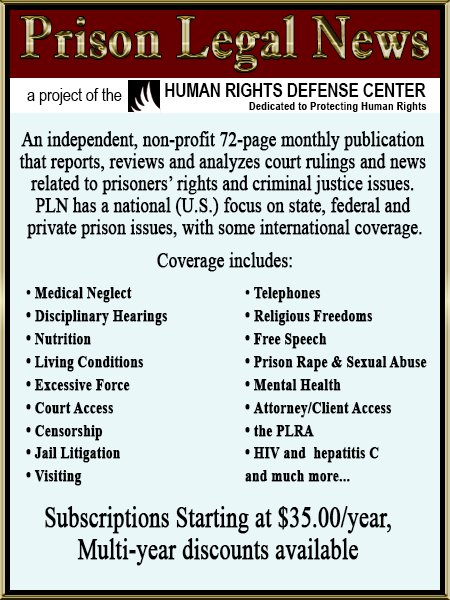
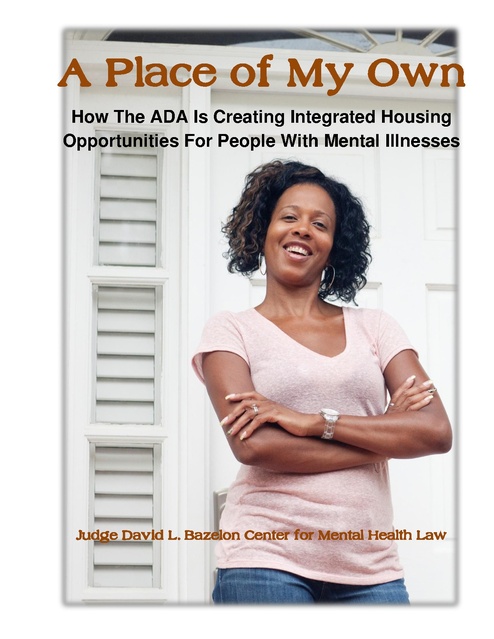
A Place of My Own - How The ADA Is Creating Integrated Housing Opportunities For People With Mental Illnesses, Bazelon Center, 2014
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
A Place of My Own How The ADA Is Creating Integrated Housing Opportunities For People With Mental Illnesses Judge David L. Bazelon Center for Mental Health Law A Place of My Own How The ADA Is Creating Integrated Housing Opportunities For People With Mental Illnesses A Place of My Own is a publication of the Judge David L. Bazelon Center for Mental Health Law, developed by Jennifer Mathis, the center’s Director of Programs, with assistance from Robert Bernstein, the center’s President and CEO. The Bazelon Center gratefully acknowledges the essential support provided by Copies of this report will be available to download via: www.bazelon.org/portals/0/Where We Stand/Community Integration/Olmstead/A Place of My Own. Bazelon Center for Mental Health Law.pdf March 2014 JUDGE DAVID L. BAZELON CENTER FOR MENTAL HEALTH LAW 1101 Fifteenth Street NW Suite 1212 Washington DC 20005-5002 202.467.5730 (voice) 202-223-0409 (fax) www.bazelon.org Introduction Over the past several years, the Americans with Disabilities Act (ADA) has been used to create supported housing for tens of thousands of individuals with mental illnesses who are needlessly institutionalized or at risk of needless institutionalization. The ADA’s “integration mandate” requires public entities to administer their services to individuals with disabilities in the most integrated setting appropriate to their needs. In 1999, the Supreme Court clarified that the integration mandate prohibits states from administering their service systems in a way that needlessly institutionalizes individuals with disabilities, and requires them to offer these individuals services in integrated settings unless doing so would fundamentally alter disability service systems. For virtually all people with disabilities, the most integrated setting appropriate is their own apartment or home, with the supports that they need to live there. Thus, as the law has developed, it has become clear that states must develop more supported housing—an apartment or home with a flexible package of supportive services individually tailored to the person’s needs—to enable individuals with disabilities to avoid needless segregation. Almost 24 years after passage of the ADA, hundreds of thousands of individuals with disabilities remain needlessly segregated across the country in psychiatric hospitals, institutions for individuals with intellectual and other developmental disabilities, nursing homes, board and care homes, and other similar facilities. The political power of the private industries that serve individuals with disabilities in segregated settings has blocked states from offering these individuals integrated alternatives. By offering individuals with disabilities only segregated settings, however, states place themselves at risk of liability under the ADA. In addition to private lawsuits, the United States Department of Justice has been actively pursuing litigation against states to enforce the rights of individuals with disabilities to live, work and receive services in the most integrated setting appropriate to their needs. 1 History of Deinstitutionalization Advocacy seeking supported housing is the latest chapter in a decadeslong movement to promote the integration of individuals with disabilities into their communities. Large-scale deinstitutionalization of individuals with disabilities began occurring in the 1960’s and 1970’s, in large part in response to a civil rights movement on behalf of individuals with psychiatric and intellectual disabilities confined in massive public institutions. Between 1955 and 1980, the census of public psychiatric institutions decreased from 559,000 to 154,000. 1 By 2000, it had decreased to less than 50,000.2 The community services that were supposed to be developed for individuals leaving institutions, however, did not materialize on the scale initially envisioned, as federal and state dollars for these programs dried up. While the deinstitutionalization of the 1970’s and 1980’s was successful in shutting and downsizing institutions, Advocacy seeking “it was less successful in promoting investments in supported housing the kind of community service infrastructure that enables people with psychiatric disabilities to thrive is the latest in the community.”3 chapter in a decades-long movement to promote the integration of individuals with disabilities into their communities. When Congress enacted Medicaid in the 1960’s, it excluded coverage for people in state psychiatric facilities because such care had traditionally been a state responsibility. However, Medicaid does cover nursing home care, providing federal dollars to pay for at least half of such costs. Taking advantage of this coverage, states moved many people from state psychiatric hospitals into nursing homes. By 1980, 750,000 people with 1 Chris Koyanagi, Learning from History: Deinstitutionalization of People with Mental Illness as Precursor to Long-Term Care Reform 6 (2007), http://www.nami.org/template.cfm?Section=about_the_issue&template=/contentmanagement/con tentdisplay.cfm&contentid=137545. 2 Ronald W. Manderscheid et al., Changing Trends in State Psychiatric Hospital Use from 2002 to 2005, 60 Psychiatric Services 29 (Jan. 2009). 3 Samuel R. Bagenstos, The Past and Future of Deinstitutionalization Litigation, 34 Cardozo Law Review 1 (2012). 2 serious mental illnesses lived in nursing homes, representing approximately 44% of the nursing home population.4 Over the years, many other people who left state psychiatric hospitals went to large board and care homes or other, similar institutional facilities.5 Others went to congregate group homes. These congregate living models were state-of-the-art technology many decades ago; they pre-date the ADA and reflect an era when the standard of practice consisted largely of discharging people from state hospitals to programs and Congregate living models housing arrangements that would were state-of-the-art prevent recidivism. In many ways, technology many decades nursing homes and other congregate ago; they pre-date the ADA settings fulfilled that goal. and reflect an era when the But newer technologies such standard of practice consisted as supported housing have enabled largely of discharging people people with mental illnesses to live from state hospitals to the same kinds of lives as people programs and housing without disabilities, rather than living arrangements that would in special facilities designed for prevent recidivism. individuals with disabilities. Moreover, the ADA includes a legal mandate to promote integration, recovery and participation in the mainstream of community life. Congregate housing models persist today largely because of public systems’ inertia and vested financial interests among program operators. They are outmoded and segregated in comparison to supported housing, where individuals live in ordinary housing with assistance tailored to their specific needs. 4 Koyanagi, supra note 1, at 6. 5 See, e.g., Disability Advocates, Inc. v. Paterson, 653 F.Supp.2d 184, 197 (E.D.N.Y. Sept. 8, 2009), vacated on other grounds, Disability Advocates, Inc. v. New York Coalition for Quality Assisted Living, Inc., 675 F.3d 149 (2012) (describing transinstitutionalization of individuals from state psychiatric hospitals in New York to large, institutional “adult homes”). 3 Key Principles of Community Integration There is widespread consensus in the disability community concerning what community integration should look like. Twenty-eight national disability organizations, including the state mental health directors and the state directors of developmental disabilities services, have embraced a set of principles that include the following: Individuals with disabilities should have the opportunity to live like people without disabilities. They should have the opportunity to be employed, have a place to call home, and be engaged in the community with family and friends. Individuals with disabilities should have control over where and how they live, including the opportunity to live in their own apartment or home. Living situations that require conformity to a collective schedule or that restrict personal activities limit the right to choose. Virtually all individuals with disabilities can live in their own home with supports. Like people without disabilities, they should get to decide where they live, with whom they live, when and what they eat, who visits and when, etc. To this end, individuals with disabilities should have access to housing other than group homes, other congregate arrangements, and multi-unit buildings or complexes that are primarily for people with disabilities. They should have access to “scattered site” housing, with ownership or control of a lease. Housing should not be conditioned on compliance with treatment or with a service plan. 6 6 Community Integration for People with Disabilities: Key Principles (2013), http://www.bazelon.org/portals/0/ADA/7.30.13%20Key%20Principles%20%20Community%20Integration%20for%20People%20with%20Disabilities.pdf?utm_source=7.3 1.13Key+Principles+PR&utm_campaign=7.31.13KeyPrinciples&utm_medium=email. These principles have been embraced by ADAPT, American Association of People with Disabilities, 4 Housing programs that reflect the Key Principles of community integration align with states’ obligations under the Olmstead decision and promote the ADA’s vision that people with disabilities—including serious mental illness—move from the social sidelines and live their lives as full members of the community. Virtually all individuals with disabilities can live in their own home with supports. Like people without disabilities, they should get to decide where they live, with whom they live, when and what they eat, who visits and when, etc. American Diabetes Association, Association of University Centers on Disabilities, The Arc of the United States, Autistic Self-Advocacy Network, Bazelon Center for Mental Health Law, Depression and Bipolar Support Alliance, Disability Rights Education and Defense Fund, Easter Seals, Little People of America, Mental Health America, National Alliance on Mental Illness, National Association of Rights Protection and Advocacy, National Association of State Directors of Developmental Disabilities Services, National Association of State Mental Health Program Directors, National Coalition for Mental Health Recovery, National Council for Community Behavioral Healthcare, National Council on Independent Living, National Disability Rights Network, National Federation of the Blind, National Mental Health Consumers’ Self-Help Clearinghouse, National Organization on Disability, Paralyzed Veterans of America, TASH, United Spinal Association. 5 Supported Housing for People with Mental Illness Supported housing has developed over the last couple of decades, and has been widely demonstrated to have successful outcomes for people with mental illnesses, including those with significant levels of disability. In addition, supported housing comports with the choices of most people: studies have consistently shown that people with mental illnesses overwhelmingly prefer living in their own homes than living in congregate settings Studies have with other people with mental illnesses.7 consistently shown Moreover, supported housing is less costly that people with than other forms of government-financed housing for people with disabilities. mental illnesses overwhelmingly prefer living in their own homes than living in congregate settings with other people with mental illnesses. Supported housing leads to more housing stability, improvement in mental health symptoms, reduced hospitalization and increased satisfaction with quality of life, including for participants with significant impairments, when compared to other types of housing for people with mental illnesses.8 Supported housing has been endorsed by the federal government, including the U.S. Department of Housing and Urban Development,9 the Surgeon General,10 the U.S. See, e.g., Ann O’Hara, Housing for People with Mental Illness: Update of a Report to the President’s New Freedom Commission, 58 Psychiatric Services 907, 909 (July 2007). 7 8 Bazelon Center, Supportive Housing: The Most Effective and Integrated Housing for People with Mental Disabilities 1 (2010), http://www.bazelon.org/LinkClick.aspx?fileticket=eRwzUzZdIXs%3d&tabid=126. 9 U.S Dept. of Housing and Urban Dev. Office of Policy Dev. and Research. The Applicability of Housing First Models to Homeless Persons with Serious Mental Illness 102-03 (July 2007), http://www.huduser.org/publications/homeless/hsgfirst.html. 6 Department of Health and Human Services11 and the National Council on Disability.12 Supported housing operates in accordance with several core tenets: First, participants receive immediate, permanent housing in their own apartments or homes, with the rights and responsibilities of tenants. The housing is not conditioned on the resident’s compliance with his or her treatment regimen; this is known as a “housing first” approach. Stable housing is a prerequisite for people with mental illnesses to be able to focus on recovery, and a powerful motivator for people to engage in treatment.13 Providing immediate, permanent housing results in greater longterm housing stability than providing housing that is conditioned on treatment.14 Second, supported housing residents are afforded access to a comprehensive array of services needed for them to succeed, including help learning independent living skills, help maintaining housing, help securing and maintaining employment, help coordinating medical treatment, and other services. All services are voluntary. 10 U.S. Surgeon General. Mental Health: A Report of the Surgeon General (1999), chapter 4, http://www.surgeongeneral.gov/library/mentalhealth/chapter4/sec6.html#human_services. 11 U.S. Dept. of Health and Human Services, Substance Abuse and Mental Health Services Administration, Transforming Housing for People with Psychiatric Disabilities: Report (2006), http://research.policyarchive.org/17617.pdf. 12 National Council on Disability, Inclusive Livable Communities for People with Psychiatric Disabilities 17-26 (March 2008), http://www.ncd.gov/newsroom/publications/index.htm. 13 Sam Tsemberis et al., Housing First, Consumer Choice, and Harm Reduction for Homeless Individuals With a Dual Diagnosis, American Journal of Public Health, vol. 94, issue 4, at 655 (2004). 14 Tsemberis, Sam & Ronda F. Eisenberg, Pathways to Housing: Housing for Street-Dwelling Homeless Individuals with Psychiatric Disabilities, 51 Psychiatric Services 487 (Apr. 2000); Martha R. Burt & Jacquelyn Anderson, Corporation for Supportive Housing, AB2034 Program Experiences in Housing Homeless People with Serious Mental Illness 3 (2005), http://www.csh.org/index.cfm/?fuseaction=Page.viewPage&pageID=3621. 7 Third, supported housing facilitates full integration of individuals into their communities. Residents are encouraged and assisted to seek employment, volunteer work, and social activities.15 Supported housing may be financed through Medicaid and state and federal housing funds. States can use Medicaid to fund virtually all of the services provided to individuals in supported housing. While Medicaid funds may not be used to fund rental subsidies, states may use certain Medicaid authorities to pay for start-up costs including security deposits, utility start-up costs, and furniture. Many states have rental subsidy programs that may be used for individuals with mental illnesses in supported housing. Often state rental subsidies are used until an individual is able to secure a federal rental subsidy— for example, under the Section 8 housing program. Typically individuals pay no more than 30 percent of their income (including SSI benefits) toward rent, with a rental subsidy covering the remainder. Supported housing is significantly less expensive than institutional care. States that reallocate funds from institutional settings to supported housing as they downsize or close institutions have been able to realize substantial cost savings. 15 Bazelon Center, supra note 7, at 1-2. 8 The ADA’s Integration Mandate and the Olmstead Decision The ADA, enacted in 1990, was intended “to provide a clear and comprehensive national mandate for the elimination of discrimination against individuals with disabilities.”16 Title II of the ADA prohibits discrimination based on disability by state and local government entities.17 In the ADA’s findings, Congress recognized the longstanding problem of isolation and segregation of people with disabilities, stating that: “historically, society has tended to isolate and segregate individuals with disabilities, and, despite some improvements, such forms of discrimination against individuals with disabilities continue to be a serious and pervasive social problem; “discrimination against individuals with disabilities persists in such critical areas as . . . institutionalization . . . ; “individuals with disabilities continually encounter various forms of discrimination, including outright intentional exclusion, . . . failure to make modifications to existing facilities and practices, . . . 18 [and] segregation . . . .” Congress’s findings apply to all people with disabilities, including people with mental illnesses. The ADA’s application to segregation is particularly relevant to individuals with serious mental illnesses, who have a long history of being physically segregated in state hospitals and other congregate facilities, resulting in negative stereotypes and social isolation. 16 §12101(b)(1). 17 42 U.S.C. § 12132. 18 42 U. S. C. §§12101(a)(2), (3), (5). 9 In 1999, the Supreme Court interpreted the ADA’s integration mandate in Olmstead v. L.C.,19 a case brought by two women with mental illnesses and intellectual disabilities who challenged their continued confinement in a state psychiatric hospital after they had been determined The ADA’s application ready for discharge. The Court held that needless institutionalization was a form of to segregation is discrimination prohibited by the ADA. particularly relevant to According to the Court, this holding reflected individuals with serious two evident judgments. First, needlessly institutionalizing individuals with disabilities mental illnesses, who “perpetuates unwarranted assumptions that have a long history of persons so isolated are incapable or being physically unworthy of participating in community life.”20 Second, “confinement in an institution segregated in state severely diminishes the everyday life hospitals and other activities of individuals, including family congregate facilities, relations, social contacts, work options, economic independence, educational resulting in negative advancement, and cultural enrichment.”21 stereotypes and social States must offer services in community isolation. settings to interested individuals who are needlessly institutionalized unless doing so would fundamentally alter their service systems.22 In Disability Advocates Inc. v. Paterson,23 later vacated on other grounds, a federal district court considered ADA integration claims brought by approximately 4,000 individuals with mental illnesses living in large, segregated board and care homes called “adult homes.” These are among the outdated facilities that, many decades ago, had been used by states to downsize their state psychiatric hospitals. The lawsuit involved adult homes with at least 120 beds and where at least 25 percent of the residents had a mental illness (individuals with mental illnesses constituted about 80 percent of the overall population of the homes in question). The court held that New York was violating 19 527 U.S. 581 (1999). 20 Id. at 600. 21 Id. at 601. 22 Id. at 604-07. 23 Disability Advocates, Inc. v. Paterson, supra note 5. 10 the ADA’s integration mandate by administering, planning and funding its mental health system in such a way that, for thousands of individuals with mental illness, adult homes were the only residential option available. While the adult homes are not operated by the state, the state is “responsible for determining what services to provide, in what settings to provide them, and how to allocate funds for each program.”24 The State “plan[s] how and where services for individuals with mental illnesses will be provided, and . . . allocate[s] the State’s resources accordingly.”25 The State licenses, monitors, inspects, and regulates adult homes, and has the power to determine their availability.26 Applying the principles set forth in Olmstead, the district court found that adult homes are institutions that segregate people with mental illnesses from the community, that supported housing is a more integrated setting than adult homes (and the most integrated setting for virtually all adult home residents with mental illness), that virtually all adult home residents with mental illnesses are qualified to live in supported housing, and that many of these residents would choose to live in supported housing if afforded a meaningful choice.27 Accordingly, the district court held that New York discriminated against DAI’s constituents by needlessly institutionalizing them in adult homes. While a federal appeals court vacated the decision based on a finding that the plaintiff, Disability Advocates, Inc., did not have standing to bring the case, it left untouched all of the findings of fact and conclusions of law concerning the merits of the case.28 The adult homes case was ultimately refiled as a class action case, and the United States Justice Department brought its own action against the state based on the same facts—New York’s continued needless segregation of individuals with mental illnesses in adult homes. The two cases were filed together with a settlement agreement between the class of adult home residents, the Justice Department, and New York. That settlement was approved by the court and requires the state to develop supported housing for thousands of adult home residents with serious mental illness. It is described in the section below concerning Olmstead settlement agreements. 24 Disability Advocates, Inc. v. Paterson, 598 F. Supp.2d 289, 319 (E.D.N.Y. Feb. 19, 2009). 25 Disability Advocates, Inc. v. Paterson, supra note 5, at 192. 26 Id. at 194. 27 Id. at 198-265. 28 Disability Advocates, Inc. v. New York Coalition for Quality Assisted Living, Inc., 675 F.3d 149 (2d Cir. 2012). 11 The case has been cited by many other courts, and the reasoning of the decision has been reflected in many subsequent community integration lawsuits and court decisions. Needlessly institutionalizing individuals with disabilities “perpetuates unwarranted assumptions that persons so isolated are incapable or unworthy of participating in community life.” 12 Justice Department Guidance In 2011, the Justice Department issued guidance concerning the ADA’s integration mandate and the Olmstead decision.29 The guidance defines the “most integrated setting” as “a setting that enables individuals with disabilities to interact with non-disabled persons to the fullest extent possible,” and makes clear The guidance specifies that: “Integrated settings are those that provide individuals with disabilities opportunities to live, work, and receive services in the greater community, like individuals without disabilities. Integrated settings are located in mainstream society; offer access to community activities and opportunities at times, frequencies and with persons of an individual’s choosing; afford individuals choice in their daily life activities . . . .”30 The guidance describes scatteredsite housing with supportive services as an example of an integrated setting. By contrast, the guidance states that segregated settings include: that remedies for the segregation of individuals in institutions or large congregate facilities should include providing these individuals with “opportunities to live in their own apartments or family homes, with necessary supports” congregate settings populated exclusively or primarily with individuals with disabilities; congregate settings characterized by regimentation in daily activities, lack of privacy or autonomy, policies limiting visitors, or limits on 29 See Statement of the Department of Justice on Enforcement of the Integration Mandate of Title II of the Americans with Disabilities Act and Olmstead v. L.C., and Questions and Answers on the ADA’s Integration Mandate and Olmstead Enforcement, http://www.ada.gov/olmstead/q&a_olmstead.pdf. 30 Id. at 3, Question 1. 13 individuals’ ability to engage freely in community activities and to manage their own activities of daily living; or settings that provide for daytime activities primarily with other individuals with disabilities.31 The guidance states that the ADA’s integration mandate applies not just to a state’s use of public institutions, but also to a state’s administration of a service system that relies on privately operated institutions. A state may violate the ADA when it “finances the segregation of individuals with disabilities in private facilities” or “through its planning, service system design, funding choices, or service implementation practices, promotes or relies upon the segregation of individuals with disabilities in private facilities or programs.”32 In addition, the guidance clarifies that, as many courts have ruled, the integration mandate also applies to people with disabilities who are at serious risk of institutionalization. Thus, individuals who are homeless and have a mental illness may have a right to receive supported housing if they are at serious risk of institutionalization. In addition, individuals who are living in their own homes and receiving services may be able to prevent cuts to those services if they can show that these cuts will place them at serious risk of institutionalization.33 The guidance states that the ADA’s integration mandate applies not just to a state’s use of public institutions, but also to a state’s administration of a service system that relies on privately operated institutions. The guidance specifies that remedies for the segregation of individuals in institutions or large congregate facilities should include providing these individuals with “opportunities to live in their own apartments or family homes, with necessary supports” and “expanding the services and supports necessary for individuals’ successful community tenure,” including supported housing, crisis services, assertive community treatment (“ACT”) teams, case management, peer support services, supported employment, and other services.34 31 Id. 32 Id. at 3, Question 2. 33 Id. at 5, Question 6. 34 Id. at 8, Question 15. 14 HUD Guidance The Department of Housing and Urban Development (HUD) has issued guidance concerning the integration mandate’s applicability to federally funded housing programs. Programs and activities that receive federal financial assistance, including HUD-financed housing programs, must comply with Section 504 of the Rehabilitation Act. Section 504 imposes obligations on covered entities that are largely the same as the ADA’s requirements, including the requirement to administer services to individuals with disabilities in the most integrated setting appropriate to their needs.35 HUD’s guidance observes that as states “rebalance” their service systems to shift away from providing long-term services to individuals with disabilities in hospitals, nursing homes, adult care facilities and other institutions, these efforts are frustrated in many states by a lack of integrated housing options. “As a For communities that result, there is a great need for affordable, integrated housing have historically relied opportunities where individuals with heavily on institutional disabilities are able to live and interact settings and housing with individuals without disabilities, while receiving the health care and built exclusively or long-term services and supports they primarily for individuals need.”36 The HUD guidance notes that “[f]or communities that have historically relied heavily on institutional settings and housing built exclusively or primarily for individuals with disabilities, the need for additional integrated housing options scattered throughout 35 with disabilities, the need for additional integrated housing options scattered throughout the community becomes more acute. 29 U.S.C. § 794. 36 Statement of the Department of Housing and Urban Development on the Role of Housing in Accomplishing the Goals of Olmstead, at 1, http://portal.hud.gov/hudportal/documents/huddoc?id=OlmsteadGuidnc060413.pdf. 15 the community becomes more acute.”37 HUD reiterated much of what the Justice Department said about integrated and segregated settings, and listed as examples of integrated settings: “scattered-site apartments providing permanent supportive housing, tenant-based rental assistance that enables individuals with disabilities to lease housing in integrated developments, and apartments for individuals with various disabilities scattered throughout public and multifamily housing developments.”38 37 Id. at 2. 38 Id. at 6. 16 Olmstead Settlement Agreements The vast majority of Olmstead cases involving individuals with mental illnesses have resolved through settlement agreements rather than court rulings. Most settlement agreements that states have entered with the Justice Department and/or private litigants focus on the development of supported housing for individuals with mental illnesses who are needlessly institutionalized. Other settlements have included similar relief for individuals with intellectual or developmental disabilities, though the terminology of “supported housing” is not used. Below we describe how some of the key settlement agreements have promoted, or will promote, the development of supported housing. Presumption that Supported Housing is the Most Integrated Setting The Olmstead settlements entered by the Justice Department and by private litigants typically obligate states to establish a process to assess institutional residents to determine what is the most integrated setting appropriate to their needs and what services would be needed for them to succeed in that setting. These settlements generally require that the assessments operate with the presumption that scattered-site supported housing is the most integrated setting appropriate and that individuals with disabilities are capable of living in that setting. Some of the settlements set forth the narrow circumstances in which that presumption can be overcome. For example, the settlement between adult home residents, New York, and the United States provides that adult home residents will be eligible for supported housing unless they (a) have significant dementia, (b) would be a danger to self or others in supported housing, even if receiving needed services, (c) need skilled nursing care that cannot be provided outside of a nursing home or hospital, or (d) need services that are not available through any publicly or privately financed program.39 Settlement Agreement in O’Toole v. Cuomo, United States v. New York, Nos. 13-CV-4165, 13CV-4156 (proposed settlement agreement filed July 23, 2013), at F.5, http://www.bazelon.org/portals/0/In%20Court/Current%20Cases/Current%20Cases/DAI/Court% 20Documents/7.23.13DAI%20settlement%20(1).pdf. See also Williams v. Quinn, at par. 9, http://www.bazelon.org/LinkClick.aspx?fileticket=FCDIyZfA5jk%3d&tabid=195 (permanent supportive housing considered the most integrated setting appropriate for Class Members except where institutional residents (i) have severe dementia or other severe cognitive impairments 39 17 Ensuring Informed Choice of Living Settings Many of the settlements require states to have supported housing providers or individuals with mental illnesses who are living in supported housing conduct ongoing efforts to engage institutional residents, educate them about supported housing (including the services and financial benefits available to residents of supported housing), and explore and address any concerns that residents may have about living in supported housing. This process, sometimes known as “in-reach,” typically includes facilitating visits by institutional residents to supported housing, providing photographs or virtual tours of supported housing units, and identifying supported housing residents willing to speak with institutional residents.40 Such a process is important to ensure that individuals can exercise informed choice about where to live. Many individuals have the experience of being told where they will live. Many are unfamiliar with supported housing, or are unaware that they would receive a rental subsidy or how much of their SSI benefits they would keep. Many have been told that they are incapable of living outside of an institution and thus have difficulty believing that they can. Others have had negative experiences when living in their own apartments or homes in the past, in situations where they did not receive services or a rental subsidy. Educating individuals about their options and exploring their concerns will help ensure that they can make meaningful choices. Ensuring that Individuals Receive Needed Services Another critical aspect of most recent Olmstead settlements is a requirement that states provide the services that individuals need in order to live successfully in supported housing. These services, determined through an individualized planning process, may include case management, assertive community treatment, supported employment, peer support, crisis services, and/or other services. requiring such a high level of staffing to assist with activities of daily living or self-care management that they cannot effectively be served in supportive housing, (ii) have medical needs requiring a high level of skilled nursing care that may not safely be provided in supportive housing, or (iii) present an imminent danger to themselves or others). See, e.g., O’Toole v. Cuomo settlement, supra note 38, at par. E (“In-Reach”); Williams v. Quinn consent decree, supra note 38, at pars. 6(d) and 10. 40 18 Supported Housing Generated Under Olmstead Settlements Below are descriptions of some of the key Olmstead settlement agreements that expand supported housing for people with mental illnesses: United States v. New York, O’Toole v. Cuomo (adult homes in New York; settlement preliminarily approved 2014): New York will develop at least 2000 units of scattered-site supported housing for adult home residents with serious mental illness, and as many as needed to afford all residents with serious mental illnesses the opportunity to live in supported housing if they are qualified for it and want it. There are approximately 4000 adult home residents with serious mental illnesses in the homes These settlements that are the subject of the settlement generally require agreement. This is the refiled adult homes case discussed earlier. that the assessments operate with the presumption that scattered-site supported housing is the most integrated setting appropriate and that individuals with disabilities are capable of living in that setting. United States v. New Hampshire, Amanda D. v. Hassan (state psychiatric hospital and state nursing home for individuals with serious mental illnesses in New Hampshire; settlement approved 2014): New Hampshire will develop more than 600 units of scattered-site supported housing for residents of New Hampshire Hospital and the Glencliff Home, as well as individuals who, within the last two years, have been admitted multiple times to New Hampshire Hospital, have used crisis or emergency services for mental health reasons, have had criminal justice involvement as a result of a mental illness, or have been unable to access needed community services. United States v. North Carolina (privately operated adult care homes for individuals with psychiatric disabilities in North Carolina; settlement approved 2012): North Carolina will develop 3000 units of 19 scattered-site supported housing for individuals with serious mental illnesses who reside in, or are at risk of admission to, large adult care homes. United States v. Delaware (state psychiatric hospital; settlement approved 2011): Delaware will develop 650 units of scattered-site supported housing for individuals with serious and persistent mental illnesses served in, or at risk of admission to, Delaware Psychiatric Center or private psychiatric hospitals that are paid for with state funds. United States v. Georgia (state psychiatric hospitals; settlement approved 2010): Georgia will develop approximately 9000 supported housing for state psychiatric hospital residents who are qualified for and want it. Half of the units must be scattered-site. Williams v. Quinn (privately operated “Institutions for Mental Diseases” in Illinois; settlement approved 2010): Illinois will develop 646 units of scattered-site supported housing for IMD residents over the first two years, and then a sufficient amount of additional units to ensure that all IMD residents with mental illnesses who are qualified for supported housing and want it have the opportunity to transition to supported housing. There are more than 4000 individuals with mental illnesses in IMDs. These settlement agreements vary in their terms based upon the circumstances under which each was negotiated. Accordingly, they differ somewhat in the numbers of new housing units to be developed and how the state will demonstrate that the individuals are integrated within the community. Collectively, however, they reflect the goal of providing individuals with mental illnesses opportunities to live successfully in the community mainstream, and they should result in the development of supported housing and services for many thousands of such individuals across the country. 20 Medicaid Rules Promoting Supported Housing Recent revisions to the federal Medicaid rules concerning services in “home and community-based settings” will promote the expansion of supported housing for individuals with disabilities. These rules, which became effective on March 17, 2014, provide that such home and community-based settings must be chosen by the individual, from among various options including settings that are not disability-specific (i.e. a home or apartment in mainstream housing). 41 These settings must be integrated in and support full access to the greater community (including opportunities to seek employment, work in competitive integrated settings, engage in community life, control personal resources, and receive services in the community), ensure a person’s rights of privacy, dignity, respect, and freedom from coercion and restraint, optimize autonomy and independence in conducting daily activities and making life choices, and facilitate choice regarding Many of the settings services and who provides them.42 Certain in which individuals settings are presumed not to be home and with mental illnesses community-based, including settings in a publicly or privately-owned facility that currently live and provides inpatient treatment, settings on the receive Medicaidgrounds of or adjacent to a public funded home and institution, and settings that have the effect community-based of isolating individuals from the broader services do not meet community.43 the requirements of the new regulations. These rules are expected to create significant changes in how disability service systems operate. Many of the settings in which individuals with mental illnesses currently live and receive Medicaid-funded 41 42 C.F.R. §§ 441.301(c), 441.530(a), 441.710(a). 42 Id. 43 Id. 21 home and community-based services do not meet the requirements of the new regulations. Moreover, most individuals with mental illnesses who live in congregate settings—or in apartment buildings occupied primarily or exclusively by other people with disabilities—have not been given the choice of living in their own home in mainstream housing, as required by the new regulations. These regulations, which allow states a transition period to come into compliance, create incentives for states to invest more heavily in supported housing settings for individuals with mental illnesses. 22 Taking Advantage of the Changed Landscape The ADA and Section 504 have created tremendous opportunities for the development of supported housing. These laws include an “integration mandate” requiring that services for people with disabilities be administered in the most integrated setting appropriate to their needs. For virtually all people with mental illnesses, the most integrated setting is their own home or apartment, with the services (if any) that they need to succeed there. Accordingly, the federal government has made clear that developing scattered-site supported housing, with a housing subsidy and the individualized services that an individual needs to succeed, should be the focus of states’ efforts to comply with the integration mandate. New Medicaid rules also create significant incentives for states to expand supported housing and reallocate dollars from institutional settings to finance this expansion. These developments provide an excellent opportunity for the development of additional supported housing for individuals with mental illnesses. As states make efforts to comply with the ADA’s integration mandate, the development of supported housing is becoming an important priority, and one that holds the promise of improving the lives of individuals with mental illnesses as well as enabling states to realize cost savings. 23