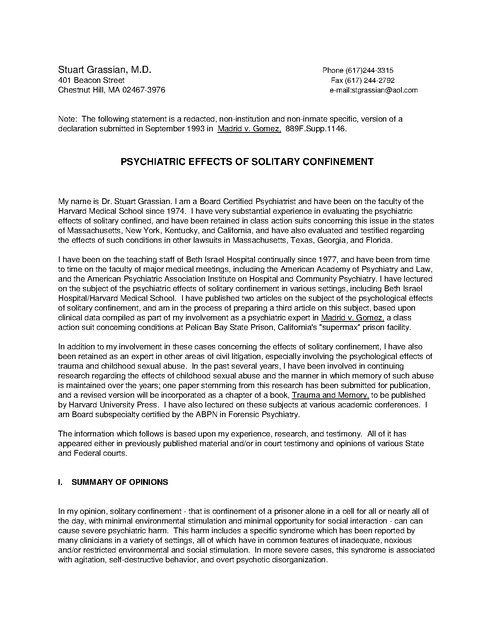
Psychiatric Effects of Solitary Confinement, Grassian Declaration, 1993
Download original document:
Document text
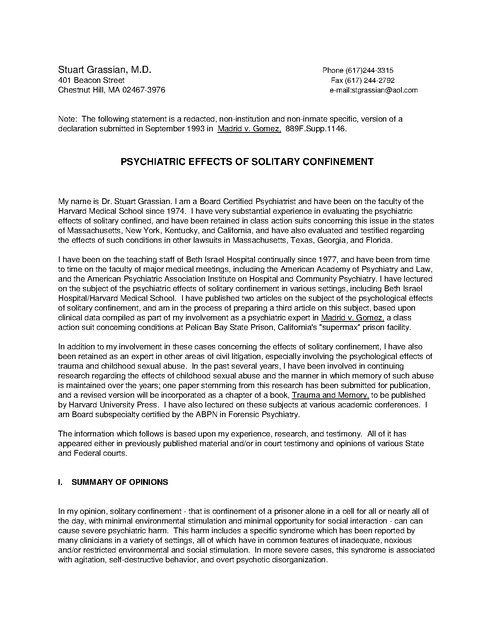
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
Stuart Grassian, M.D. 401 Beacon Street Chestnut Hill, MA 02467-3976 Phone (617)244-3315 Fax (617) 244-2792 e-mail:stgrassian@aol.com Note: The following statement is a redacted, non-institution and non-inmate specific, version of a declaration submitted in September 1993 in Madrid v. Gomez, 889F.Supp.1146. PSYCHIATRIC EFFECTS OF SOLITARY CONFINEMENT My name is Dr. Stuart Grassian. I am a Board Certified Psychiatrist and have been on the faculty of the Harvard Medical School since 1974. I have very substantial experience in evaluating the psychiatric effects of solitary confined, and have been retained in class action suits concerning this issue in the states of Massachusetts, New York, Kentucky, and California, and have also evaluated and testified regarding the effects of such conditions in other lawsuits in Massachusetts, Texas, Georgia, and Florida. I have been on the teaching staff of Beth Israel Hospital continually since 1977, and have been from time to time on the faculty of major medical meetings, including the American Academy of Psychiatry and Law, and the American Psychiatric Association Institute on Hospital and Community Psychiatry. I have lectured on the subject of the psychiatric effects of solitary confinement in various settings, including Beth Israel Hospital/Harvard Medical School. I have published two articles on the subject of the psychological effects of solitary confinement, and am in the process of preparing a third article on this subject, based upon clinical data compiled as part of my involvement as a psychiatric expert in Madrid v. Gomez, a class action suit concerning conditions at Pelican Bay State Prison, California's "supermax" prison facility. In addition to my involvement in these cases concerning the effects of solitary confinement, I have also been retained as an expert in other areas of civil litigation, especially involving the psychological effects of trauma and childhood sexual abuse. In the past several years, I have been involved in continuing research regarding the effects of childhood sexual abuse and the manner in which memory of such abuse is maintained over the years; one paper stemming from this research has been submitted for publication, and a revised version will be incorporated as a chapter of a book, Trauma and Memory, to be published by Harvard University Press. I have also lectured on these subjects at various academic conferences. I am Board subspecialty certified by the ABPN in Forensic Psychiatry. The information which follows is based upon my experience, research, and testimony. All of it has appeared either in previously published material and/or in court testimony and opinions of various State and Federal courts. I. SUMMARY OF OPINIONS In my opinion, solitary confinement - that is confinement of a prisoner alone in a cell for all or nearly all of the day, with minimal environmental stimulation and minimal opportunity for social interaction - can can cause severe psychiatric harm. This harm includes a specific syndrome which has been reported by many clinicians in a variety of settings, all of which have in common features of inadequate, noxious and/or restricted environmental and social stimulation. In more severe cases, this syndrome is associated with agitation, self-destructive behavior, and overt psychotic disorganization. In addition, solitary confinement often results in severe exacerbation of a previously existing mental condition, or in the appearance of a mental illness where none had been observed before. Even among inmates who do not develop overt psychiatric illness as a result of confinement in in solitary, such confinement almost inevitably imposes significant psychological pain during the period of isolated confinement and often significantly impairs the inmate's capacity to adapt successfully to the broader prison environment. Moreover, although many of the acute symptoms suffered by these inmates are likely to subside upon termination of solitary confinement, many -- including some who did not become overtly psychiatrically ill during their confinement in solitary -- will likely suffer permanent harm as a result of such confinement. This harm is most commonly manifested by a continued intolerance of social interaction, a handicap which often prevents the inmate from successfully readjusting to the broader social environment of general population in prison and, perhaps more significantly, often severely impairs the inmate's capacity to reintegrate into the broader community upon release from imprisonment. In my experience, many inmates housed in such stringent conditions are extremely fearful of acknowledging the psychological harm or stress they are experiencing as a result of such confinement. This reluctance of inmates in solitary confinement is in substantial measure a response to the perception that such confinement is an overt attempt by authorities to "break them down" psychologically, and in my experience, tends to be more severe when the inmate experiences the stringencies of his confinement as being the product of an arbitrary exercise of power, rather than the fair result of an inherently reasonable process. Furthermore, in solitary confinement settings, mental health screening interviews are often conducted at the cell front, rather than in a private setting, and inmates are generally quite reluctant to disclose psychological distress in the context of such an interview, since such conversation would inevitably be heard by other inmates in adjacent cells, exposing them to possible stigma and humiliation in front of their fellow inmates. Lastly, the adverse impact of punitively imposed solitary confinement will often be more severe than the effect of such confinement when it is imposed for administrative purposes, since by intent, punitive solitary confinement imposes stringencies and deprivations which are in excess of those which are minimally required to maintain an inmate in segregated confinement; such stringencies often include limitations on programming, occupational and education opportunities, visitation, use of telephone, television and radio access, and access to reading materials, among others. Conversely, inmates housed in segregation for administrative reasons - such as for the protection of the inmate himself from possible harm by other inmates - will often retain access to many of the same opportunities and privileges which are provided to inmates in congregate housing. Indeed,the institutional policies which create different conditions in administrative segregation, as opposed to punitive segregation, reflect an important underlying reality - that "institutional security" actually is employed to mean two very different things. The narrower usage of the terms reflects concerns about the safety of the individual inmate being housed, as well as the safety of those with whom he has contact. The broader use of the term, however, is fundamentally unbounded - or at least, has boundaries which are not really distinguishable from the broad purposes of any system of criminal justice. The harsh stringencies which are employed in punitive segregation reflect institutional assumptions that the harshly painful deprivations associated with a sentence to punitive solitary confinement, will serve as a deterrence to other in mates who might be tempted to break institutional rules. This rationale for imposing pain on an offender - the rationale that the punishment of this offender might deter other possible offenders - is simply a rationale for any system of criminal justice and punishment. A multiyear sentence of punitive solitary confinement is an imposition of pain of staggering proportions, and it is imposed without the due process safeguards which anchor our system of criminal justice. DECLARATION OF DR. STUART GRASSIAN 2 II. SOLITARY CONFINEMENT CAN CAUSE SEVERE PSYCHIATRIC HARM A. Solitary Confinement Can Cause a Specific Psychiatric Syndrome During the course of my involvement as an expert, I have had the opportunity to evaluate the psychiatric effects of solitary confinement in well over 100 prisoners in various state and federal penitentiaries. I have observed that for many of the inmates so housed, incarceration in solitary caused either severe exacerbation or recurrence of preexisting illness, or caused the appearance of an acute mental illness in individuals who had previously been free of any such illness. I became aware of the particular toxicity of solitary confinement when I first had the opportunity to evaluate prisoners in solitary confinement as a result of my involvement in a class action lawsuit in Massachusetts, Libby v. Hogan, which challenged conditions in solitary confinement at the maximum security State Penitentiary in Walpole, Massachusetts. The clinical observations I made in the course of my involvement in that lawsuit, coupled with my research into the medical literature concerning this issue, have formed the basis of two articles I have since published on this topic in peer-reviewed journals. These are: 1. Grassian, S. (1983). "Psychopathological Effects of Solitary Confinement." American Journal of Psychiatry, 140, 1450-1454. 2. Grassian, S., & Friedman, N. (1986). "Effects of Sensory Deprivation in Psychiatric Seclusion and Solitary Confinement." International Journal of Law and Psychiatry, 8, 49-65. My subsequent professional experience has included observations of similar phenomena in many other solitary confinement settings. When I initially agreed to evaluate the Walpole prisoners, I had not yet reviewed the literature on the psychiatric effects of solitary confinement and, indeed, I was somewhat skeptical; I expected that inmates would feign illness and exaggerate whatever psychiatric symptomatology they suffered. I discovered, however, something very different. Contrary to my expectations, the prisoners appeared to be extremely defensive about the psychiatric problems they were suffering in SHU; they tended to rationalize away their symptoms, avoid talking about them, or deny or distort their existence, all in an apparent effort to minimize the significance of their reactions to isolation. Numerous interviews began with statements such as "solitary doesn't bother me" or "some of the guys can't take it -- not me", or even with the mention of a symptom and a simultaneous denial of its significance: "As soon as I got in I started cutting my wrists. I figured it was the only way to get out of here." As my interviews progressed, these facile accounts gave way to descriptions of experiences which were very worrisome. For example, one inmate was unable to describe the events of the several days surrounding his wrist-slashing, nor could he describe his thoughts or feelings at the time. Similarly, the prisoner who said he could "take it" eventually came to describe panic, fears of suffocation, and paranoid distortions which he suffered while in isolation. Moreover, the specific psychiatric symptoms reported were strikingly consistent among the inmates: 1. The Specific Psychiatric Syndrome Associated With Solitary Confinement. a.. Hyperresponsivity to External Stimuli More than half the prisoners reported a progressive inability to tolerate ordinary stimuli. For example, "You get sensitive to noise -- the plumbing system. Someone in the tier above me pushes the button on the faucet . ... It's too loud, gets on your nerves. I can't stand it. I start to holler." b. Perceptual Distortions, Illusions, and Hallucinations DECLARATION OF DR. STUART GRASSIAN 3 Almost a third of the prisoners described hearing voices, often in whispers, often saying frightening things to them. There were also reports of noises taking on increasing meaning and frightening significance. For example, "I hear noises, can't identify them -- starts to sound like sticks beating men, but I'm pretty sure no one is being beaten . . . I'm not sure." These perceptual changes at times became more complex and personalized: "They come by with four trays; the first has big pancakes. I think I am going to get them. Then someone comes up and gives me tiny ones -- they get real small, like silver dollars. I seem to see movements -- real fast motions in front of me. Then seems like they are doing things behind your back -- can't quite see them. Did someone just hit me? I dwell on it for hours." c. Panic Attacks Well over half the inmates interviewed described severe panic attacks while in SHU. d. Difficulties With Thinking, Concentration and Memory Many reported symptoms of difficulty in concentration and memory; for example, "I can't concentrate, can't read . . . Your mind's narcotized. Sometimes can't grasp words in my mind that I know. Get stuck, have to think of another word. Memory's going. You feel like you are losing something you might not get back." In some cases this problem was far more severe, leading to acute psychotic, confusional states. One prisoner had slashed his wrists during such a state and his confusion and disorientation had actually been noted in his medical record. e. Intrusive Obsessional Thoughts: Emergence of Primitive Aggressive Ruminations Almost half the prisoners reported the emergence of primitive aggressive fantasies of revenge, torture, and mutilation of the prison guards. In each case, the fantasies were described as entirely unwelcome, frightening and uncontrollable. For example, "I try to sleep 16 hours a day, block out my thoughts -muscles tense -- think of torturing and killing the guards -- lasts a couple of hours. I can't stop it. Bothers me. Have to keep control. This makes me think I'm flipping my mind . . . I get panicky -- thoughts come back -- pictured throwing a guard in lime -- eats away at his skin, his flesh -- torture him -- try to block it out, but I can't." f. Overt Paranoia Almost half the prisoners interviewed reported paranoid and persecutory fears. Some of these persecutory fears were short of overt psychotic disorganization. For example: "Sometimes get paranoid -think they meant something else. Like a remark about Italians. Dwell on it for hours. Get frantic. Like when they push buttons on the sink. Think they did it just to annoy me." In other cases this paranoia deteriorated into overt psychosis: "Spaced out. Hear singing, people's voices, 'Cut your wrists and go to Bridgewater and the Celtics are playing tonight.' I doubt myself. Is it real? . . . I suspect they are putting drugs in my food, they are putting drugs in my cell . . . The Reverend, the priest -- even you -- you're all in cahoots in the Scared Straight Program." g. Problems With Impulse Control Slightly less than half of the prisoners reported episodes of loss of impulse control with random violence: "I snap off the handle over absolutely nothing. Have torn up mail and pictures, throw things around. Try to control it. Know it only hurts myself." Several of these prisoners reported impulsive self-mutilation; "I cut my wrists many times in isolation. Now it seems crazy. But every time I did it, I wasn't thinking -- lost control -- cut myself without knowing what I was doing." DECLARATION OF DR. STUART GRASSIAN 4 2. This Syndrome has the Characteristics of an Acute Organic Brain Syndrome -- a Delirium. Clearly, these symptoms were very dramatic, and they moreover appeared to form a discreet syndrome -that is, a constellation of symptoms occurring together and with a characteristic course over time, thus suggestive of a discreet illness. Moreover, this syndrome was strikingly unique -- some of the symptoms described above are found in virtually no other psychiatric illness: Acute dissociative, confusional psychoses are a rare phenomenon in psychiatry; random, impulsive violence in the context of such confusional state is exceedingly rare. But the most unique symptoms in this cluster are the striking and dramatically extensive perceptual disturbances experienced by the isolated person. Indeed, these disturbances are almost pathognomonic of the syndrome, meaning they are symptoms virtually found nowhere else. For example, loss of perceptual constancy (objects becoming larger and smaller, seeming to "melt" or change form, sounds becoming louder and softer, etc.) is very rare, and when found is far more commonly associated with neurologic illness (especially seizure disorders and brain tumors affecting sensory integration areas of the brain) then with primary psychiatric illness. (When seen in primary psychiatric illness, it is basically only seen in especially severe, insidious, early onset schizophrenia -- the kind of schizophrenic illness which has always been thought to clinically "feel" like a fundamentally biological/neurologic disease.) In addition, functional psychiatric illness very rarely presents with such severe and florid perceptual distortions, illusions, and hallucinations simultaneously affecting multiple perceptual modalities -- auditory, visual, olfactory, tactile, kinesthetic. (In fact, in the more common psychotic illnesses such as schizophrenia and psychotic depression, auditory hallucinations are by far the most common type, visual hallucinations come a distant second, and hallucinations in all other modalities are actually very uncommon; moreover, combined modality hallucinations -- other than the combination of auditory with visual -- are exceedingly rare.) Similarly, hyperresponsivity to external stimuli with a dysesthetic (subjectively painful) response to such stimuli, is likewise rare; in fact it is exceedingly rare, so rare that appearance of this symptom also might suggest an organic -- brain dysfunction -- etiology. (This symptom is similar, for example, to the experience many people have during a febrile illness of finding any touching of their body exceedingly unpleasant or the inability of a patient with a headache to tolerate an even ordinary volume of sound, or the inability of some pregnant women to tolerate even ordinary smells without becoming nauseated.) Thus, the fact that all of these quite unusual symptoms ran together in the same syndrome was itself a clear confirmation of the distinct nature of this syndrome. While this syndrome is strikingly atypical for the functional psychiatric illnesses, it is in fact quite characteristic of an acute organic brain syndrome -- that is, delirium, a syndrome characterized by a decreased level of alertness, EEG abnormalities, and by the same perceptual and cognitive disturbances, fearfulness, paranoia, and the same agitation and random, impulsive and self-destructive behavior which I observed in the Walpole population. Moreover, delirium is a syndrome which is known to result from the type of conditions -- including restricted environmental stimulation -- which are characteristic of solitary confinement; even the EEG abnormalities characteristic of delirium have been observed in individuals exposed to conditions of sensory deprivation. By now, the potentially catastrophic effects of restricted environmental stimulation have been the subject of a voluminous medical literature; annual international symposia are being held on the subject, and the issue has even found its way into the popular media. (The literature is summarized in the appendices to this statement.) B. Psychiatric Disturbances Occurring in Other Settings of Restricted Environmental Stimulation. DECLARATION OF DR. STUART GRASSIAN 5 My involvement in class-action lawsuits in New York State, California and Kentucky has yielded observation of the effects of solitary confinement which are quite parallel to my observations at Walpole. (These findings are discussed later in this statement.) In addition, Earlier published reports on the effects of solitary confinement describe findings which are quite similar to my observations at Walpole. In addition, a pattern of psychiatric disturbances similar to those I found at Walpole have been seen in a variety of other -- non-prison -- settings, all of which, however, share in common features of restricted environmental stimulation: These latter have included observations of prisoners of war, of hostages, of patients with impairment of their sensory apparatus (for example, hearing or visually impaired patients), of patients confined in the intensive care unit, of patients undergoing long term immobilization in hospital (e.g. spinal traction patients), of observations of psychiatric difficulties suffered by explorers (for example, Arctic and Antarctic exploration by individuals and small groups) and of observations of difficulties encountered by pilots during solo jet flight. In all of these situations, despite the multiple differences which exist between them, the very same syndrome emerges. The literature documenting this fact is well-known, rich and detailed. It is reviewed in the Appendices to this declaration. C. The Historical Experience With Solitary Confinement: The Nineteenth Century Experience. 1. The Origin of the American Penitentiary and the Nineteenth Century German Experience Preindustrial societies had often not made any fundamental distinction between deviant behavior seen as the product of "criminal intent" as opposed to behavior seen as stemming from "mental illness." For such societies, deviant behavior -- whatever its origins -- was a social evil that was deeply feared and cruelly punished. In Colonial America, the Salem witch trials were but one example of a continuing tendency to equate "lunacy" with "demonic possession" and, ultimately, with "evil." Deviant behavior was naturally feared and hated; the instinctive response was to punish it cruelly, lock it away, banish it, or kill its perpetrator. Thus, in Colonial America generally, the social response to deviant behavior was relatively simple: the protection of the larger society was paramount, while the distinction between "illness" and "evil" was far less critical. Indeed, the social response to deviance largely stemmed from the severe puritanical belief in innate human evil that deserved violent retaliation such as whipping, pillories, stockades, brandings, and, ultimately, the gallows. At times, when there was a more "humane" response to persons viewed as suffering from lunacy, this response consisted simply of keeping the individual caged under lock and key, often for the rest of his life. But in the early nineteenth century, a surge of great social optimism swept over America, and along with this grew a belief in the possibility of social reform, perhaps an overly optimistic faith in the possibility of rehabilitation of persons whose behavior was deviant. Not coincidentally, this spirit gave rise virtually simultaneously to two great social reform movements in the United States: the development of large mental hospitals and the construction of the first large penitentiaries. Both of these institutions were founded upon a similar premise -- namely, that psychological and social deviance was largely a result of the evils and stresses of "modern society", and both held a fundamental belief that healing would naturally occur if the deviant individual was removed from the evils of the larger society, and thus enabled to know his own true nature. DECLARATION OF DR. STUART GRASSIAN 6 In the case of the mental hospital, this belief gave rise to the concept of a healing, pastoral, therapeutic community. But in the case of the penitentiary, an additional safeguard was obviously required; the inmates clearly had to be protected, not only from the evil influences of the broader society, but also from the evil influences of each other. The proper approach thus appeared to be to give each inmate the opportunity to live a life alone, like a penitent monk in his own monastic cell. Thus, the earliest American penitentiaries were, generally, systems of rigid solitary confinement. Extravagant attention was paid to the design of these institutions, to ensure the absolute and total isolation of the offender from any "evil and corrupting influences." The Philadelphia Prison, completed in 1829, was particularly conscientious in this regard: The arrangements . . . guaranteed that convicts would avoid all contamination and follow a path to reform. Inmates remained in solitary cells for eating, sleeping and working. ... No precaution against contamination was excessive. Officials placed a hood over the head of a new prisoner when marching him to his cell so he would not see or be seen by other inmates . ... Thrown upon his own innate sentiments, with no evil example to lead him astray, ... the criminal would start his rehabilitation. Then, after a period of total isolation, without companions, books, or tools, ... (he) would return to the community cured of vice and idleness, to take his place as a responsible citizen. (Rothman, pp 86-87) The American penitentiary, and the Philadelphia System, became world-famous; no important visitor to the United States neglected to tour its penitentiaries and to bring back their principles for emulation in Europe. Some such as de Tocqueville of France and Nicholas Julius from Prussia came specifically for that purpose (Rothman p. 91). de Tocqueville wrote of the utter, "perfect" desolation of the American penitentiary, of the "profound silence" within its "vast walls," likening it to the silence of death. (Rothman, p. 97) 2. Psychological Effects of Severe Isolation The openness with which these institutions were held up to public scrutiny led in time to open concern about the psychological effects of such confinement. During a tour of the United States in 1842, Charles Dickens wrote with pathos of the Philadelphia Prison: The system here is rigid, strict and hopeless solitary confinement. ... Over the head and face of every prisoner who comes into this melancholy house, a black hood is drawn, and in this dark shroud, ... he is led to the cell from which he never again comes forth, until his whole term of imprisonment had expired. He is a man buried alive . ... dead to everything but torturing anxieties and horrible despair . . . . The first man I saw ... answered ... always with a strange kind of pause ... he gazed about him and in the act of doing so fell into a strange stare as if he had forgotten something. In another cell was a German ... a more dejected, brokenhearted, wretched creature, it would be difficult to imagine. There was a sailor . ... Why does he stare at his hands and pick the flesh open, upon the fingers, and raise his eyes for an instant ... to those bare walls ... ? (quoted in Liederman, p. 66) American concern about the effects of rigid solitary confinement began as early as the 1830's. Statistical comparisons began to be made between the Philadelphia system and its chief competitor -- the Auburn system prevailing in New York State at Auburn and Sing-Sing penitentiaries. The latter system also utilized solitary confinement, but less rigidly; inmates left their cells to work together in workshops and DECLARATION OF DR. STUART GRASSIAN 7 exercise in a common courtyard, although here, too, absolute and strict silence was maintained at all times. Statistical comparisons began to generate evidence that "it was unnatural . . . to leave men in solitary, day after day, year after year; indeed, it was so unnatural that it bred insanity." (Rothman, p. 87). The Philadelphia Prison appeared to have a higher incidence, not only of insanity, but also of physical disease and death than its New York State counterparts. Meanwhile, the American system had been emulated in many major European prisons, such as at Halle, Germany. Although the Americans had been the world leaders in instituting rigid solitary confinement in their penitentiary system, Germans clinicians eventually assumed the task of documenting its demise. Between 1854 and 1909, 37 articles appeared in German scientific journals on the subject of psychotic disturbances among prisoners, summarizing years of work and hundreds of cases. A major review of this literature was published in 1913; (Nitsche, 1913). A summary and synthesis of this rather large body of work appears as an appendix to this declaration. But it should be noted that interest in the problem was not purely academic; psychotic disturbances among prisoners were of such frequency in these prisons that they attracted administrative as well as clinical concern, and great effort was made to explain this disturbing incidence. Thus, the literature covered a variety of issues, speculating for example, on the "moral degeneracy" of the prison population, some authors by comparing the psychopathology of those who committed "crimes of passion" with those who committed "crimes against property," or by detailing the incidence of the major diagnostic categories of the time (e.g., "circular insanity," "alcoholic psychoses," epilepsy, general paresis, etc.) among the prison population. However, multiple reports based on careful clinical observation suggested that a substantial majority of these prison psychoses were direct reactions to the conditions of imprisonment itself. Gradually a clinically distinguishable syndrome of acute reactive prison psychoses began to be defined. Different variables were considered in attempting to explain the etiology of these reactive prison psychoses, including, for example, long versus short duration of imprisonment, or imprisonment of those already convicted versus imprisonment while awaiting trial. However, the most consistent factor described, reported in over half the total literature, was solitary confinement. D. The Twentieth Century Experience: Prisoners of War, Brain Washing" and Experimental Research. 1. Prisoners of War and "Brainwashing". Unfortunately, other than some anecdotal reports, there was little discussion of the psychological effects of solitary confinement in the medical literature during the first half of the twentieth century. Undoubtedly, this was in part a consequence of the disastrous earlier experience with such confinement. As statistical evidence accumulated during the nineteenth century that solitary confinement produced a very disturbing incidence of insanity, physical disease and death, the system had fallen into disrepute, and with this, it had changed from an open, optimistic experiment in social reform into a hidden, secretive place of punishment and control. Its devastating psychological impact, however, did not change, a fact which became suddenly and very painfully evident in the 1950's as the American public began hearing the frightening and dramatic reports of "brainwashing" of American prisoners of war in Korea -- reports that alterations in the sensory environment were being intentionally imposed upon these prisoners in a seemingly Orwellian attempt to profoundly disrupt their psychological equilibrium. (Biderman and Zimmer, 1961). By the 1950's, reports had already appeared of major psychiatric disturbances among survivors of prolonged solitary confinement in war (e.g., Burney, 1952), but during the decade of the Korean War, DECLARATION OF DR. STUART GRASSIAN 8 major attention was riveted on the occurrence of these disturbances, not only in war, but in a variety of other settings as well. In 1956, the Group for the Advancement of Psychiatry (GAP) held a symposium -- "Factors Used to Increase the Susceptibility of Individuals to Forceful Indoctrination" -- to study methods used by the Chinese and Russian Communists to "indoctrinate" and "break the will" of political prisoners and prisoners of war. Dr. M. Meltzer, former Chief Medical Officer at Alcatraz Federal Penitentiary contributed his observations of psychiatric disturbances among prisoners exposed to punitive solitary confinement at Alcatraz. These prisoners were rarely confined for periods beyond one week. (Meltzer, 1956) Despite this, Dr. Meltzer described acute psychotic breakdowns among prisoners so confined; his descriptions closely paralleled the observations at Walpole: "The motor effects ranged from occasional tense pacing, restlessness and sense of inner tension with noise making, yelling, banging and assaultiveness at one extreme, to a kind of regressed, dissociated, withdrawn hypnoid and reverie-like state at the other . . . (The) sense of self, the ego and the ego boundary phenomena are profoundly affected by the isolation." (Meltzer, p. 98) In the same symposium, Dr. John Lilly of the National Institute of Mental Health noted that despite the importance of other factors which tended to "weaken personalities and make them more susceptible to [forced indoctrination]" -- such as semi-starvation, physical pain and injury, and sleep deprivation -- social and sensory isolation was still the central pathogenic factor in such confinement. (Meltzer, p. 89) 2, Experimental Research on Sensory Deprivation. An experimental model was therefore designed to study the effect of such sensory deprivation; this research, conducted during the 1950's and early 1960's, primarily at Harvard and McGill University Medical Centers, was in fact funded in large part by the United States Government -- and especially by the Department of Defense and U.S. Central Intelligence Agency. This research is described as an appendix to this declaration. Its relevant conclusions can, however, be described relatively briefly: In these studies (Brownfield, 1965; Solomon, et al., 1961), subjects were placed in a situation designed to maximally reduce perceptually informative external stimuli (e.g., light-proof, soundproof rooms, cardboard tubes surrounding the arms and hands to reduce proprioceptive and tactile sensation, and so on). The research revealed that characteristic symptoms generally developed in such settings. These symptoms included perceptual distortions and illusions in multiple spheres, vivid fantasies, often accompanied by strikingly vivid hallucinations in multiple spheres, derealization experiences, and hyperresponsivity to external stimuli. What was also clear, however, was that while some subjects tolerated such experiences well, many did not, and a characteristic syndrome was observed, including not only the above symptoms, but also included cognitive impairment, massive free-floating anxiety, extreme motor restlessness, emergence of primitive aggressive fantasies which were often accompanied by fearful hallucinations, and with decreasing capacity to maintain an observing, reality-testing ego function. In some cases, an overt psychosis supervened with persecutory delusions and, in some cases, a marked dissociative, catatoniclike stupor (delirium) with mutism developed. EEG recordings confirmed the presence of abnormalities typical of stupor and delirium. These findings clearly demonstrated that this experimental model did reproduce the findings in the nonexperimental situations, including the findings among prisoners of War, held in solitary confinement. E. Factors Affecting Response to Sensory Restriction and Solitary Confinement. Much of the subsequent research in this area attempted to delineate variables which might explain these differing outcomes. These variables can be divided into two categories: i) differences among various DECLARATION OF DR. STUART GRASSIAN 9 conditions of perceptual deprivation, and ii) differences in preexisting personality functioning among individuals experiencing such conditions: 1. Differing Conditions of Isolation. One of the factors that was commonly cited in the research was differences in the intensity and duration of the sensory deprivation; more severe sensory restriction, the presence of noxious stimulation, and longer duration oof the sensory deprivation experience,e have all been associated with an increased risk of adverse psychiatric consequences. In my experience, while conditions experienced by inmates in various prison solitary confinement settings generally bear some similarities (e.g. a cell of roughly 50-80 square feet, approximately 22 1/2 hours/day locked in the cell, with about one hour/day 5-7 days/week of exercise yard), in other respects, the conditions are fairly variable. For example, some cells have barred doors, which allow better ventilation, sound transmission and visual connection with the outside environment than do mesh steel doors; solid steel doors are the most restrictive - especially when they are either hinged or slide shut with almost no air gap from the wall. Moreover, administrative conditions regarding the amount and circumstances of visitation, the availability of reading material, reading, and television, and so forth, are all factors which vary from institution to institution, and even from time to time within a given institution. 2. The Perceived Intent of the Isolation Experience. In addition to the factors described above, another critical factor in determining the effect of isolation, appears to be the perceived intent of the isolation> Experimental research has demonstrated that an individual who receives clues which cause him to experience the isolation situation as potentially threatening, is far more likely to develop adverse psychiatric reactions to the isolation experience; conversely, if the subject has reason to believe the situation is likely to be benign, he will be far more likely to tolerate or even enjoy it. Among the latter group of subjects who tolerated isolation well, many reported pleasant or, at least nonthreatening, visual imagery, fantasy and hallucinatory experiences. "His mind may begin to wander, engage in daydreams, slip off into hypnogogic reveries with their attendant vivid pictorial images . . . he may be quietly having sexual or other pleasurable thoughts." (Wright & Abbey, 1965, pg. 6.) This finding is perhaps not surprising. It appears that sensory restriction, produces perceptual disturbances and illusions, which are analogous to those produced by hallucinogenic drugs -- and clearly, while there are some individuals who could be said to have volunteered to undergo such hallucinatory, psychotic-like experiences, it must be almost uniformly terrifying to be forced involuntarily to undergo an experience similar to that induced by hallucinogenic drugs. 3. Individual Differences in Response. Many studies have demonstrated that there is great variability among individuals in regard to their capacity to tolerate a given condition of sensory restriction. This variability helps to provide further insight into the nature of the toxic effect of such isolation conditions, and provides striking corroboration of the fact that such deprivation of environmental stimulation, especially when of prolonged duration, is toxic to brain functioning, and causes symptoms characteristic of stupor and delirium. Generally, individuals with mature, healthy personality functioning and of at least average intelligence are most able to tolerate the regressive pull and perceptual intrusions of such isolation situations. On the other hand, individuals with primitive or psychopathic functioning, individuals with borderline cognitive capacities, impulse-ridden individuals and individuals whose internal emotional life is chaotic or fearful, are especially at risk for severe psychopathologic reactions to such isolation. (Appendix C describes these studies in more detail.) DECLARATION OF DR. STUART GRASSIAN 10 Moreover, there is clear evidence that in a situation of restricted environmental stimulation, preexisting central nervous system dysfunction is a major predisposing factor to the development of adverse psychiatric reactions and of overt delirium. For example, in one study of patients suffering visual deprivation following eye surgery (eye-patched patients), those patients with preexisting central nervous system dysfunction were found to be at especially high risk to develop symptoms of delirium. (Ziskind et.al. 1960). Moreover, the presence of a preexisting personality disorder or impairment of psychosocial functioning was associated with increased risk of incapacitating fearfulness, paranoia, agitation and irrational aggression towards staff (Klein & Moses 1974). (A more extensive review of this literature is contained in Appendix A to this declaration.) In addition, individuals may at times be exposed to situations which cause impairment of central nervous system functioning. Such situations -- especially if they impair the individual's state of alertness, for example, sleep deprivation, abnormal sleep-wake cycles, or the use of sedating medication -- will substantially increase the individual's vulnerability to the development of delirium. Delirium among postsurgical patients, and the so-called "ICU Psychoses" are examples of this phenomenon. (Appendix A discusses this issue in more detail.) One of the characteristic difficulties experienced by inmates in solitary confinement is, in fact, abnormal sleep-wake cycles and impaired sleep. a. Findings at Pelican Bay State Prison. These findings received further corroboration in my observations of inmates at Pelican Bay State Prison, California. In 1991-92, as part of my participation in Madrid v. Gomez -- a class-action lawsuit challenging conditions at Pelican Bay State Prison, a new "supermax" facility in California -- I evaluated 49 inmates housed in the Special Housing Unit (SHU) at the institution, and prepared a lengthy report to the Federal Court of my findings. (Much of the literature review and historical material in the present declaration is taken from my Madrid declaration.) Many of the inmates I evaluated there suffered severe psychiatric disturbances while housed in Pelican Bay SHU -- either springing up de novo while so incarcerated, or representing a recurrence or severe exacerbation of preexisting illness. Of the 49 inmates I evaluated, at least 17 were actively psychotic and/or acutely suicidal and urgently in need of acute hospital treatment, and 23 others suffered serious psychopathological reactions to solitary confinement, including in several cases, periods of psychotic disorganization. The clinical data at Pelican Bay also added striking corroboration that the severe and prolonged restriction of environmental stimulation in solitary confinement is toxic to brain functioning, by demonstrating that the most severe, florid psychiatric illnesses resulting from solitary confinement tend to be suffered by those individuals with preexisting brain dysfunction. As noted before, I have observed a high incidence of preexisting central nervous system dysfunction among inmates I evaluated in solitary confinement settings. This was also the case at Pelican Bay, and statistical analysis of the Pelican Bay data quite dramatically demonstrated that inmates with such preexisting vulnerability were the most likely to develop overt confusional, agitated, hallucinatory psychoses as a result of SHU confinement. b. Attention Deficit and Antisocial Personality Disorders. In addition, research regarding Attention Deficit Disorder and Antisocial Personality Disorder demonstrated that these conditions are similarly associated with a particular inability to tolerate restricted environmental stimulation. There is in fact increasing evidence that childhood impulsivity and Attention Deficit Hyperactivity Disorder bear some relationship to Antisocial Personality Disorder, that both are characterized by impulsivity and stimulation-seeking behavior, and that both involve biologically based abnormalities in central nervous system functioning. Moreover, the clinical literature demonstrates that individuals with Antisocial Personality Disorder are especially intolerant of restricted environmental stimulation. For example, Quay (1965) characterized the psychopathic individual as pathologically DECLARATION OF DR. STUART GRASSIAN 11 "stimulation seeking ... impulsive ... (and) unable to tolerate routine and boredom." (Appendix B contains a more detailed discussion.) Given the exigencies of conducting clinical observations of inmates in solitary confinement, it is not surprising that little systematic attempt has been made to elucidate the underlying psychological characteristics of those most at risk for developing severe psychopathological reactions to such isolation. However, among the clinical reports on Ganser's Syndrome (a related condition) in non-prison populations are several studies of patients in psychiatric hospitals. These patients were, of course, available for extensive psychological assessment and observation, and these reports described the majority of these patients as suffering long-standing hysterical character disorders, having problems with severe impulsivity, childhood truancy, and antisocial behavior patterns. (Appendix B contains a more detailed discussion.) Thus, the medical literature demonstrates that individuals whose internal emotional life is chaotic and impulse-ridden, and individuals with central nervous system dysfunction, may be especially prone to psychopathologic reactions to RES in a variety of settings. Yet among the prison population, it is quite likely that these are the very individuals who are especially prone to committing infractions that result in stricter incarceration, including severe isolation and solitary confinement. c. Langley v. Coughlin. In the late 1980's, I interviewed and reviewed the medical records of several dozen inmates confined in maximum security prisons in New York State, especially including a large group of women incarcerated at the maximum security women's prison for the State of New York at Bedford Hills. During the process of these evaluations, it became clear that a very high percentage of these women had a history of serious emotional/organic mental difficulties. Many had severe cognitive limitations, were highly emotionally labile, impulse ridden, and prone to psychotic disorganization. In many cases, the infraction which led to their original incarceration was an act which had been committed impulsively and chaotically. Under the stress of imprisonment, these inmates became even more unable to conform their behavior to the requirements of their situation. Inevitably, this resulted in their being sentenced to terms in the SHU, and once in the SHU, their subsequent course was often a nightmare. Many became grossly disorganized and psychotic, smearing themselves with feces, mumbling and screaming incoherently all day and night, some even descending to the horror of eating parts of their own bodies. The resulting lawsuit, Langley v. Coughlin, was ultimately settled by consent decree. The settlement provided injunctive relief as well as monetary damages both for the mentally ill inmates whose emotional condition had deteriorated during their incarceration in the SHU, and also for the non-mentally ill women who had been subjected to the bedlam of mental illness created in their SHU environment. The injunctive relief required the prison to begin to reframe the meaning it gave to behavioral disturbances which they had previously responded to by further SHU time. Under the settlement, the prison began to actively consider whether such disturbances were the result of organic personality disturbances, affective or impulse disorders, or even of schizophreniform illness. The result of these changes was apparently quite dramatic. Many of the prisoners who had been in SHU began to be treated in a residential psychiatric unit within the prison. This unit had previously refused to treat such inmates, claiming that their security needs were greater than could be handled. When pressed to provide services as a result of the settlement, not only did the unit discover that it was able to provide those services, but moreover discovered that the custodial and security needs of these inmates dramatically decreased when their behavioral disturbances were framed as psychiatric problems rather than as a security issue. Thus, as a result of the settlement of the lawsuit, all parties to the suit benefited -- prisoners and the officers of the correctional facility alike. DECLARATION OF DR. STUART GRASSIAN 12 d. Effects on Psychologically More Resilient Inmates: Baraldini v. Meese and Hameed v. Coughlin. In 1988, in the course of my involvement in Baraldini v. Meese, a class-action challenging the confinement of a small group of women in a subterranean security housing unit at the Federal Penitentiary in Lexington, Kentucky, I had the opportunity to interview several women who were in confinement in this facility. These women had been convicted of having committed politically motivated crimes, were all highly educated, and had a history of relatively strong psychological functioning prior to their confinement. None of these women developed the florid confusional psychosis described earlier in this affidavit, yet each of them demonstrated significant psychopathological reactions to their prolonged confinement in a setting of severe environmental and social isolation. These included perceptual disturbances, free-floating anxiety and panic attacks. These inmates also uniformly described severe difficulties in thinking, concentration and memory; for example, one inmate reported that she was able to perform tasks requiring some mental effort - such as reading or writing - only for about the first three hours of the morning after she awoke; by then, her mind had become so slowed down, so much "in a fog", that she was entirely unable to maintain any meaningful attention or expend any meaningful mental effort. In addition, in 1993, I evaluated Bashir Hameed, an inmate who had been incarcerated in the SHU at Shawangunk C.F. and who had brought suit - Hameed v. Coughlin, 89 CV 578 (NDNY) - concerning his incarceration there. As I described in my testimony in that case, Mr. Hameed is an individual who evidence strong prior psychological adjustment, and no prior psychiatric history, yet became significantly ill as a result of his SHU confinement. F. Long Term Effects of Solitary and Small Group Confinement Long-term studies of veterans of P.O.W. camps and of kidnapping and hostage situations have demonstrated that while many of the acute symptoms I outlined above tend to subside after release from confinement, there are also long-term effects which may persist for decades. These not only include persistent symptoms of post traumatic stress (such as flashbacks, chronic hypervigilance, and a pervasive sense of hopelessness), but also lasting personality changes -- especially including a continuing pattern of intolerance of social interaction, leaving the individual socially impoverished and withdrawn, subtly angry and fearful when forced into social interaction. (This literature is reviewed in Appendix D to this declaration.) In addition, from time to time I have had the opportunity to evaluate individuals who had been incarcerated in solitary confinement several years previously; I have found the same pattern of personality change described above -- these individuals had become strikingly socially impoverished and experienced intense irritation with social interaction, patterns dramatically different from their functioning prior to solitary confinement. III. Conclusions. The restriction of environmental stimulation and social isolation associated with confinement in solitary are strikingly toxic to mental functioning, producing a stuporous condition associated with perceptual and cognitive impairment and affective disturbances. In more severe cases, in mates so confined have developed florid delirium - a confusional psychosis with intense agitation, fearfulness, and disorganization. But even those inmate who are more psychologically resilient inevitably suffer severe psychological pain as a result of such confinement, especially when the confinement is prolonged, and especially when the individual experiences this confinement as being the product of an arbitrary exercise of power and intimidation. Moreover, the harm caused by such confinement may result in prolonged or permanent psychiatric disability, including impairments which may seriously reduce the inmate's capacity to reintegrate into the broader community upon release from prison. DECLARATION OF DR. STUART GRASSIAN 13 Many of the prisoners who are housed in long-term solitary confinement are undoubtedly a danger to the community and a danger to the Corrections Officers charged with their custody. But for many, they are a danger, not because they are coldly ruthless, but because they are volatile, impulse-ridden and internally disorganized. As noted earlier in this statement, modern societies made a fundamental moral division between socially deviant behavior which was seen as a product of evil intent, and that behavior seen as a product of illness. Yet this bifurcation has never been as simple as might at first glance appear. Socially deviant behavior can in fact be described along a spectrum of intent. At one end are those whose behavior is entirely "instrumental" -ruthless, carefully planned and rational; at the other are individuals whose socially deviant behavior is the product of unchecked emotional impulse, internal chaos, and often of psychiatric or neurologic illness. It is a great irony that as one passes through the levels of incarceration - from the minimum to the moderate to the maximum security institutions, and then to the solitary confinement section of these institutions -- one does not pass deeper and deeper into a subpopulation of the most ruthlessly calculating criminals. Instead, ironically and tragically, one comes full circle back to those who are emotionally fragile and, often, severely mentally ill. The laws and practices that have established and perpetuated this tragedy deeply offend any sense of common human decency. Stuart Grassian, M.D. APPENDICES Appendix A Reports of Psychiatric Disturbances in Conditions of Restricted Environmental Stimulation: Small Group Confinement Appendix B The Nineteenth Century German Experience with Solitary Confinement: Ganser's Syndrome Appendix C Experimental Research on the Psychiatric Consequence of Profound Sensory Deprivation: Factors Influencing Vulnerability To Psychiatric Harm Appendix D Reports of the Long-Term Effects of Solitary Confinement in Former Hostages and in Prisoners of War DECLARATION OF DR. STUART GRASSIAN 14 REPORTS OF PSYCHIATRIC DISTURBANCES IN OTHER CONDITIONS OF RESTRICTED ENVIRONMENTAL STIMULATION The psychopathologic syndrome which we have described in the body of this declaration is found in other settings besides isolation in civil prisons. Some of these settings involve small group, rather than solitary isolation, and the studies have demonstrated that isolated groups comprising two individuals may be the most pathogenic of all. These studies also suggest that those individuals with below average intelligence and poor psychosocial adjustment prior to isolation developed more severe psychiatric difficulties during isolation in some studies, such disturbances persisted in one year follow-up after reentry. Aviation Bennett (1961) described psychiatric disturbances among pilots of the British Royal Air Force who had been exposed in-flight to periods of restricted auditory and visual stimulation. All of the groups he described became significantly anxious--many suffering full-blown panic attacks--and many experienced unusual sensations which they were very reluctant to describe. The most severely disturbed groups refused to expose themselves further to the isolation conditions of these flights; at all levels of impairment, however, anxiety was common (both panic and free-floating anxiety). Pilots reported anxiety symptoms such as feeling "hot and tense and powerless" (Bennett, p. 162) and "nervous and afraid" (ibid, p. 164). Feelings of derealization, feelings of detachment from reality, and perceptual distortions were described. Some of these perceptual distortions were dangerous (e.g., having the impression that the aircraft was turning when it was not) and resulted in serious errors in judgment (e.g., making the aircraft spiral dangerously downward after attempting to "correct" for what was incorrectly perceived as a turning aircraft). Clark & Graybiel (1957) described strikingly similar symptoms among United States Navy pilots exposed to periods of in-flight isolation. Among pilots who flew alone, at high altitude, (i.e., in a situation of monotonous visual and sensory stimulation) and flying with a minimum of pilot activity, over one third experienced frightening feelings of unreality and became severely anxious. Small Group Confinement Many studies--both anecdotal and experimental--have been made of individuals confined together in small groups; groups thus described have ranged in size from two to approximately sixty individuals, the larger groups include reports of men isolated on a Pacific island, submarine inhabitants, Antarctic explorers, etc. (see Zubek, 1969). The most consistent finding was of dramatically increased levels of hostility, interpersonal conflict and paranoia (Zubek, p. 377). Individuals exposed to such conditions also tend to become irrationally territorial, staking out "areas of exclusive or special use, [and] acting with hostility to trespasses by others." (Zubek, p. 380) Confined groups comprising just two individuals may be the most pathogenic of all, associated with especially high rates of mutual paranoia and violent hostility. Admiral Byrd believed it to be extremely unsafe to staff an Antarctic base unit with just two men: "It doesn't take two men long to find each other out... the time comes ... when even his [campmate's] unformed thoughts can be anticipated, his pet ideas become a meaningless drool, and the way he blows out a pressure lamp or drops his boots on the floor or eats his food becomes a rasping annoyance.... Men who have lived in the Canadian bush know well what happens to trappers paired off this way ... During my first winter at Little America I walked for hours with a man who was on the verge of murder or suicide over imaginary persecutions by another man who had been his devoted friend" (Zubek, 1969, p.381). Many men confined in Antarctic stations have experienced near psychotic states, creating a danger to all inhabitants of the work station (Zubek, 1969). The pathogenicity of such dyadic groups was confirmed in DECLARATION OF DR. STUART GRASSIAN 15 an experimental study involving volunteer sailors living and working together in dyadic pairs, socially isolated from the world for a period of ten days. Under such conditions, the sailors developed evidence of subjective distress, inability to concentrate, a breakdown of inner controls on behavior, hostility, and increasing schizoid withdrawal from social contact (Cole, J.D., 1967). Polar Habitation Psychiatric disturbances have been described in Arctic and Antarctic inhabitants (explorers, researchers and their support staff), spending varying periods in winter isolation. In these regions, winters last for up to nine months with weather conditions so cold (-100F) that leaving the confines of the indoors is dangerous. Typically, teams of work groups have fewer than 50 members who spend up to two years working in small quarters. Small group isolation conditions at these stations have been compared to life in prisons by at least one researcher: "... the isolation imposed by the harsh environment [of the Antarctic] is rarely experienced outside penal conditions" (Biersner & Hogan, 1984, p. 491). In a review of the literature on the psychological adjustment to Antarctic living, Rothblum (1990) described a staff wintering over at a British Antarctic station; those of the staff who adjusted best tended to be socially mature, intelligent, reserved and trusting individuals. Similarly, French, United States and Australian studies revealed that intelligence and previous social adjustment predicted a decreased risk for psychiatric disturbance among workers at Antarctic stations. On the other hand, lack of respect for authority and aggression were important markers for poor isolation adjustment (Mullin & Connery, 1959). Similarly, Wright, Chylinski, Sisler and Quarrington (1967) correlated outcome measures with psychological testing obtained prior to work station assignment. They found specifically that persons with antisocial and psychotic tendencies were poor risks for efficient functioning in conditions of isolation. As a result of these disturbing findings among Antarctic workers, systematic efforts have been made to provide psychological screening of potential station employees and to ameliorate the isolation conditions prevailing in such stations (Cochrane & Freeman, 1989). Despite these efforts, significant psychiatric disturbances have continued to be observed (Natini & Shurley, 1974). The fact that these individuals were confined in small groups rather than alone was not found to prevent these disturbances; indeed, one of the central pathogenic factors cited in this literature has been the interpersonal tension and hostility generated by small group confinement (Biersner & Hogan, 1984). Strange & Klein (1974) and Rothblum (1990) described a "winter-over syndrome" including progressively worsening depression, hostility, sleep disturbance, impaired cognitive functioning and paranoia during small group winter confinement in the Antarctic. Strikingly similar findings were reported by the United States Navy Medical Neuropsychiatric Research Unit, which found high incidences of sleep disturbance, depression, anxiety, aggression, somatic complaints, and a progressive impoverishment of social relationships as the winter progressed (Gunderson, 1963; Gunderson & Nelson, 1963). Psychiatric problems worsened as the length of time in this confinement increased; in one study of a group of Japanese winter-stationed in the Antarctic periodic psychological testing revealed increasing levels of anxiety and depression as the winter progressed (Rothblum, 1990). Similar findings have been described among a group of Americans stationed in the Antarctic (Gunderson & Nelson, 1963). In a review of the literature on the psychological adjustment to Arctic life, Cochrane and Freeman (1989) describe a syndrome which parallels the Antarctic literature: sleep disturbances, apathy, irritability, cognitive, dysfunction, hallucinations, depression and anxiety were widely reported as a result of the small group isolation endured by inhabitants. They also reported "depression, irritability, easily provoked anger which may escalate into dramatic and florid acting out and, not surprisingly, a breakdown in relationships with other members of the group . . . insomnia, pallor, loss of interest, psychomotor retardation, paranoidal ideation, non-specific hallucinations of light flashes and sudden movements" (p. 887) Many individuals became intolerant of social contact, and fearful of reentering society. Even when Arctic DECLARATION OF DR. STUART GRASSIAN 16 workers were adequately preselected by psychological screening, trained and supported, sleep difficulties, apathy and irritability persisted. Studies on reintegration into the home environment after Antarctic living even one year after reintegration, found persisting problems and symptoms, including sleep disturbances, cognitive slowing, emotional withdrawal, resentment of authority, indecisiveness and poor communication (Rothblum, 1990). Biersner & Hogan (1984) summarized the findings related to personality variables in the Arctic and Antarctic workers: Individuals with high needs for novelty and new sensations ... who are emotionally unstable, or who are unconcerned with social approval seem unsuited for ... such environments. The opposite [traits are found in] those who adjust well (p.495) Explorers: Solo Voyages Anecdotal reports of shipwrecked sailors and individuals accomplishing long solo sea voyages have generally described "disturbances in attention and in organization of thought, labile and extreme affect, hallucinations and delusions" (Zubek, 1969, p. 7). Dramatic anecdotal reports have appeared from time to time. Some of these were summarized in a review article by Dr. Philip Solomon, one of the lead scientists in the Harvard Medical School/Boston City Hospital group: "Christine Ritter in her very sensitive document `A Woman in the Polar Night,' reported that at times she saw a monster ... [and] experienced depersonalization to the extent that she thought she and her companions were dissolving in moonlight `as though it were eating us up' ... The Spitzbergen hunters use the term ran (strangeness) to describe these experiences ..." Tales of the sea have provided many accounts of hallucinatory phenomena. John Slocum sailed alone around the world . . . [In the South Atlantic] he suddenly saw a man, who at first he thought to be a pirate, take over the tiller . . . . Walter Gibson, a soldier in the British Indian Army, was on a ship torpedoed in the Indian Ocean by the Japanese in World War II .... [The shipwrecked survivors] reported that "all of us at various stages in that first week became a prey to hallucinations"... [As the weeks passed] the feeling of comradeship disappeared and the men began to find themselves "watching our fellows covertly and suspiciously." Murder, suicide and cannibalism followed as social controls dissolved. Medical Conditions 1. Eye Patched Patients Restricted environmental stimulation conditions also occur post-operatively and in certain medical conditions: in a study of 100 American patients with macular degeneration of the retina (Holroyd, Rabins, Finkelstein, Nicholson, Chase & Wisniewski, 1992), a high percentage of such patients experienced disturbing visual hallucinations. Those patients who were relatively cognitively limited, those who were socially isolated and those with simultaneous sensory impairment in another modality (e.g., hearingimpaired patients) fared worst. But other factors, including the presence of concomitant medical illness, did not appear to affect the incidence of hallucinations. In an especially relevant study of eye patched patients, Klein & Moses (1974) determined that psychologically well-adjusted patients (as assessed prior to surgery) tended not to develop visual hallucinations during the period when their eyes were patched, whereas those suffering preexisting personality disturbances did tend to develop such hallucinations. Among those patients who did develop DECLARATION OF DR. STUART GRASSIAN 17 hallucinations, almost half developed complex hallucinations involving human figures and with a content suggesting serious preoccupations with themes of depression and anxiety. Moreover, among those patients who had both preexisting personality disturbances and difficulty with their premorbid psychosocial adjustment, eye patching produced severe psychiatric symptomatology, including: paranoid thoughts about being poisoned, physically harmed or attacked; psychomotor agitation; interpersonal aggressiveness; inability to comply with staff directives; fearful visual hallucinations, and incapacitating anxiety. In this most disturbed group, symptoms had not remitted when observed one week after their eye patches were removed. Other studies have also found patients to suffer from perceptual distortions, thinking disturbances and mood changes following the visual deprivation that is part of postoperative recovery in eye surgery (Ziskind, 1958; Ziskind, Jones, Filante & Goldberg, 1960). Furthermore, Ziskind et. al., (1960) noted that: "In patients with . . . brain damage, there were also delirioid symptoms, e.g., confusion, disorientation, memory impairment, vivid hallucinations [and disorganized] hyperkinetic activity" (p. 894). Finally, in Jackson's (1969) extensive literature review of hospitalized eye patched patients, psychiatric disturbance was commonly found. These patients suffered from unusual emotional, cognitive and sensory-perceptual disturbances, similar to those previously described. 2. Poliomyelitis Polio patients confined to tank-type respirators have become psychotic as a direct result of such confinement; moreover, they became more ill, with more florid hallucinations and delusions, at night when sensory input was diminished. The same florid hallucinatory, delusional psychosis has been found in other patients similarly confined in tank respirators (Liederman, et. al., 1958). 3. Cardiac Patients Patients with decompensated heart disease are at times placed on very strict bed rest; some of these patients have developed acute confusional, paranoid, hallucinatory psychoses, especially at night during periods of decreased sensory input (Liederman, et. al., 1958). Studies of postoperative open heart surgery patients who were bed confined--their visual stimulation restricted to looking up at a white-tiled hospital room ceiling--revealed a high rate of disordered thinking, visual and auditory hallucinations and disorientation (Egerton & Kay, 1964; Kornfeld, Zimberg & Maim, 1965; Lazarus & Hagens, 1968; Wilson, 1972). There is an extremely disturbing incidence of psychosis following open heart surgery, ranging in various studies from 14 to 30 percent (Lee & Ball, 1975). Upon recovery these patients described their postoperative environment as a major pathogenic factor in producing their psychiatric illness (Kornfeld et. al., 1965). Perceptual disturbances and emotional liability, as well as paranoia, depression and obsessive-compulsive reactions to the restrictive postoperative environment have been documented in other studies as well (Ellis, 1972; Goldstein, 1976; Lee & Ball, 1975; Thomson, 1973). 4. Hearing Impaired Individuals Another condition of restricted environmental stimulation leading to psychiatric disturbance involves the hearing impaired. Studies of the deaf (Altshuler, 1971; Houston & Royse, 1954) consistently find significantly higher rates of paranoia in these individuals. High rates of paranoia have been reported in both the developmentally hearing impaired as well as those who became deaf in later life (Zimbardo, Andersen & Kabat, 1981). Experimentally induced deafness in psychiatrically unimpaired adults also produced paranoia (Zimbardo, et. al., 1981). 5. Other Medical Patients DECLARATION OF DR. STUART GRASSIAN 18 Disorientation and delusional psychoses have also been reported among immobilized orthopedic patients and in patients postsurgically bed-confined (Liederman, et. al., 1958). Nursing researchers (Downs, 1974) have studied this phenomenon and have concluded that frightening hallucinatory experiences "are probably far more widespread than has been reported" (Downs p. 434). Occupational Situations McFarland and Moore (1957) reported in the New England Journal of Medicine on a study of fifty longdistance truck drivers; of these, thirty experienced vivid visual hallucinations; some became disoriented, "as in a dream." Animal Studies As noted in the body of this declaration, many prisoners confined in solitary report become intolerant of normal levels of environmental--especially social--stimulation. These reports receive experimental confirmation in laboratory research on animals. Such research demonstrates that sensory deprivation produces an intolerance to normal levels of environmental stimulation; animals exposed to sensory deprivation conditions became overly aroused--"hyperexcitable"--when exposed to normal levels of environmental stimulation, often resulting in severe behavioral disturbances (Riestin, 1961). Other studies have demonstrated that such animals often display diffuse, frenzied, random activity, and social withdrawal, and are prone to psychophysiologic illnesses (e.g., peptic ulcers) when exposed to environmental stress (Zubek, 1969). Barnes (1959) produced agitation in mice and rats after a few days of isolation, a report which corroborated previous studies with rats. Others (Matsumoto, Cai, Satoh, Ohta & Watanabe, 1991) have also found that isolation induced aggressive behavior in mice (e.g., biting attacks). Further, social isolation has been demonstrated to produce profound and lasting psychological effects in primates. Washburn and Rumbaugh (1991) note that over 400 published investigations of the effects of social isolation on primates show such deleterious effects as self-mutilation and disturbances in perception and learning. They found than in adult rhesus monkeys even brief periods of social isolation produce compromised cognitive processing. McKinney, Suomi and Harlow (1971) produced symptoms of depression in rhesus monkeys by confining them for 30 days. They concluded that solitary "confinement produced greater destructive behavioral effects in less time and with fewer individual differences among subjects than did total social isolation, previously [demonstrated to be] the most powerful technique for producing psychopathological behavior among monkey subjects" (p. 1317). Induced depression through confinement has been reported in both young and mature monkeys (Harlow & Suomi, 1974). Finally, isolation-produced fear in dogs has been clearly demonstrated (Thompson & Melzack, 1956). DECLARATION OF DR. STUART GRASSIAN 19 THE NINETEENTH CENTURY GERMAN EXPERIENCE WITH SOLITARY CONFINEMENT Between 1854 and 1909, thirty-seven articles appeared in the German medical literature on the subject of psychotic disturbances among prisoners, summarizing years of work and many hundreds of cases. A major review of this literature was published in 1912 (Nitsche, 1912) Solitary confinement was the single most important factor identified in the etiology of these psychotic illnesses. Indeed, the first report on the subject of prison psychoses was that of Delbruck (1854), Chief Physician at the Prison at Halle, in which "the frequency of mental disturbances was at last so great that it attracted the attention of the authorities." (Nitsche, p.1). Delbruck's report concluded that: Prolonged absolute isolation has a very injurious effect on the body and mind and that it seems to predispose to hallucinations . ... He advised the immediate termination of solitary confinement. (Nitsche, p. 2). In 1863, Gutsch reported on 84 cases of "The Psychosis of Solitary Confinement" and described vivid hallucinations and persecutory delusions, apprehensiveness, psychomotor excitation, sudden onset of the syndrome, and rapid recovery upon termination of solitary confinement. Many of these individuals developed "suicidal and maniacal outbursts." (Nitsche, p. 8) In 1871, in a report on 15 cases of acute reactive psychoses, some of which apparently occurred within hours of incarceration in solitary, Reich described, in addition to hallucinosis and persecutory delusions, severe anxiety leading to "motor excitement . . .. The patient becomes noisy, screams, runs aimlessly about, destroys and ruins everything that comes in his way." He also described an acute confusional state accompanying these symptoms, sudden cessation of symptoms, recovery, and subsequent amnesia for the events of the psychosis: "The gaze is staring, vacant, indefinite. . . consciousness becomes more and more clouded . . . and later there is amnesia for all events during this time . ... He frequently awakens as from a dream . ..." (Nitsche, pp. 32-33) In a statistical summary, Knecht reported in 1881 on the diagnostic assessment of 186 inmates at the "insane department" of the prison at Waldheim, and concluded that over half the total were reactive manifestations to solitary confinement. The majority of these inmates fell insane within two years of confinement in solitary. (Nitsche, p. 17) In 1884, Sommer reported on 111 cases describing an acute, reactive, hallucinatory, anxious, confusional state associated with solitary confinement, emphasizing the "excited outbursts" and "vicious assaults" of these patients. His patients' illness began with difficulty in concentration, and hyperresponsivity to minor "inexplicable" external stimuli. These "elementary disturbances of the sensorium (i.e., the five senses)" were seen as leading to "elementary hallucinations" which became more numerous, eventually including auditory, visual and olfactory hallucinations, and eventually becoming incorporated with fearful persecutory delusions. (Nitsche, pp. 12-16) In 1889, Kirn described 129 cases of psychosis among the inmates at the county jail at Freiburg, concluding that in 50 of those cases, "solitary confinement can be definitely considered as the etiological factor, (and these) show a certain characteristic stamp" (Nitsche, p. 21) including persecutory delusions and hallucinations in multiple spheres (auditory, visual olfactory, tactile). He also noted that these symptoms often precipitated at night: "The patient is suddenly surprised at night by hallucinatory experiences which bring on an anxious excitement. These manifestations become constant from now on, in many DECLARATION OF DR. STUART GRASSIAN 20 cases occurring only at night, in others also in the daytime. Attentive patients not infrequently hear at first a humming and buzzing in their ears, unpleasant noises and inarticulate sounds which they cannot understand until finally they hear well differentiated sounds and distinct words and sentences . . . . The visual hallucinations are very vivid." (Nitsche, p. 24) In 1888, Moeli contributed a description of Vorbereiden -- "the symptom of approximate answers"1 . Ten years later Ganser contributed to the literature the elucidation of a syndrome which included Moeli's symptom. (Ganser, 1898) As Arieti points out, Ganser's Syndrome became well-known -- indeed, almost a codification of the whole body of literature on the prison psychoses. Ganser provided a comprehensive and well-elucidated synthesis of symptoms, most of which had been previously described elsewhere. The syndrome he described included, (in addition to Vorbereiden), vivid visual and auditory hallucinations, a distinct clouding of consciousness, sudden cessation of symptoms, "as from a dream" and "a more or less complete amnesia for the events during the period of clouded consciousness." Ganser's most original description was of "hysterical stigmata" within the syndrome, including conversion symptoms -especially, total analgesia. (Arieti, 1974, Vol. II, pp. 710-712) Some of the German authors failed to note whether the inmates they were describing were housed in solitary confinement and, unfortunately, Ganser was one of these, stating only that his were "prisoners awaiting trial." However, Langard, in 1901, also reporting on observations of accused prisoners awaiting trial, described an acute violent hallucinatory confusion with persecutory delusions, and specifically stated that this syndrome occurred exclusively among those who awaited trial in solitary confinement. (Nitsche, p. 32) Also in 1901, Raecke similarly reported on prisoners awaiting trial and described the full syndrome of Ganser, including Vorbereiden; he specifically condemned solitary confinement as responsible for the syndrome (Nitsche, p. 34). He described his cases as beginning with apathy, progressing to "inability to concentrate, a feeling of incapacity to think," and even catatonic features, including negativism, stupor, and mutism. (Nitsche, pp. 33-35) In another report written the same year, Skliar reported on 60 case histories of which he identified 21 as acute prison psychoses caused by solitary confinement. While Vorbereiden was not noted, most of the other symptoms described by Ganser and Raecke were noted, including: massive anxiety, fearful auditory and visual hallucinations -- in severe cases, hallucinations of smell, taste, and "general sensation" as well -- persecutory delusions, senseless agitation and violence, confusion and disorientation. The psychosis developed rapidly -- at times within hours of incarceration in solitary confinement. Catatonic symptomatology was also noted (Nitsche, pp. 35-36). The German literature reported only on prisoners who suffered gross psychotic symptomatology, some of whom were observed in hospitals or "insane departments" of prisons; thus, these reports generally described only syndromal expressions that rose to the level of overt psychosis. The German reports do, however, powerfully demonstrate the existence of a particular, clinically distinguishable psychiatric syndrome associated with solitary confinement. These multiple reports described a syndrome which included: 1. Massive free-floating anxiety 2. "Disturbances of the Sensorium", including -a. Hyperresponsivity to external stimuli 1 Vorbereiden is a rather remarkable symptom of deranged and confused thought processes in which the individual's response to a question suggests that he grasped the gist of the question, and his answer is clearly relevant to the question, and related to the obvious correct answer, yet it still oddly manages to be incorrect. An example would be: Q: "How many colors are there in the flag of the United States" A: "Four". Q: "What are they?" A: "Yellow" DECLARATION OF DR. STUART GRASSIAN 21 b. 3. 4. 5. 6. 7. Vivid hallucinations in multiple spheres (including auditory, visual, olfactory, gustatory and tactile modalities); in some reports, these began as simple "elementary" hallucinations and progressed to complex, formed hallucinations. Persecutory delusions, often incorporating coexistent complex hallucinations. Acute confusional states. In some reports, these were seen as beginning with simple inattention and difficulty in concentration. In others, the onset was described as sudden. The confusional state and disorientation was in several reports described as resembling a dissociative, dreamlike state, at times involving features of a catatonic stupor, including negativism and mutism, and upon recovery leaving a residual amnesia for the events of the confusional state. Ganser and others observed hysterical conversion symptoms during this confusional state. Vorbereiden: An infrequent finding, mostly described in conjunction with a confusional, hallucinatory state. Motor excitement, often associated with sudden, violent destructive outbursts. Characteristic course of the illness: a. Onset was described by some authors as sudden, by others as heralded by a progression beginning with sensory disturbances and/or inattention and difficulty in concentration. b. In many cases, rapid subsidence of acute symptoms upon termination of solitary confinement. The German reports were generally based upon prisoners who had been hospitalized because of their psychotic illness; in contrast, the population reported upon in the Walpole study was not preselected by overt psychiatric status; despite this, all of the major symptoms reported by the German clinicians were observed in the Walpole population, except for Vorbereiden and hysterical conversion symptoms. In addition, less severe forms of the isolation syndrome were observed in the Walpole population, including: • • • • • Perceptual distortions and loss of perceptual constancy, in some cases without hallucinations. Ideas of reference and paranoid ideation short of overt delusions. Emergence of primitive aggressive fantasies which remained ego-dystonic and with realty-testing preserved. Disturbances of memory and attention short of overt disorientation and confusional state. Derealization experiences without massive dissociative regression. Since Ganser's report has become the twentieth century's clearest memory of a much vaster body of literature, it is also of interest to review the literature describing observations of Ganser's Syndrome in non-prison populations. Several of these reports have been studies of patients in psychiatric hospitals suffering from this syndrome. Since these patients were hospitalized, it was possible to obtain more extensive evaluation and testing of their status. Several reports (Ingraham & Moriarity, 1967; May, Voegele & Padino, 1960; Tyndel, 1956; Weiner & Braiman, 1955) described a majority of the patients studied as suffering long standing hysterical conversion symptoms. Impulsivity, childhood truancy, and antisocial behavior were also commonly described. These findings suggest also that antisocial behavior patterns and psychopathic personality disorder may bear a close relationship to primitive hysterical personality disorder, a relationship which has been described by other authors as well (e.g., Woodruff, Goodwin & Gaze 1974). DECLARATION OF DR. STUART GRASSIAN 22 EXPERIMENTAL RESEARCH ON THE PSYCHIATRIC EFFECT OF PROFOUND SENSORY DEPRIVATION: FACTORS INFLUENCING VULNERABILITY TO PSYCHIATRIC HARM As noted in the body of this declaration, laboratory research has demonstrated that experimentallyinduced sensory deprivation has major psychological effects, and can precipitate severe psychiatric illness (see e.g. Brownfield, 1965; Solomon 1961). Much of the research in this area attempted to delineate factors, in addition to the duration and intensity of sensory restriction, which might account for these differing outcomes; the factors which have been elucidated include two which are especially relevant to this discussion, and may help to explain the particular malignancy of sensory deprivation in solitary confinement: The Influence of Expectation Orne and Scheibe (1964) suggested that a subject's reaction to participation in a sensory deprivation experiment could be profoundly manipulated by external cues imposed by the experimenter: "[These] dramatic effects could be a function of the demand characteristics of the experimental situation. ... There is evidence that preparing a subject for probable hallucinations significantly affects the frequency of hallucinations. Such devices as 'panic buttons' in experiments ... are in a sense eloquent instructions. The use of such a device increases the subject's expectation that something intolerable may occur, and with it, the likelihood of a bad experience. (p. 4) In their own experiment, Orne and Scheibe exposed two groups of subjects to identical conditions of sensory deprivation. The experimental group's introduction to the experiment included the presence of a medical "Emergency Tray," and instructions about a "Panic Button." As predicted, the experimental group became significantly more symptomatic in measures of cognitive impairment and restlessness, and also more symptomatic in every other measure -- including perceptual aberrations, anxiety, and spatial disorientation. In a related manner, prisoners in solitary confinement generally view such confinement as threatening and punitive, and often as a deliberate attempt to make them "crack up" or "break my spirit." In light of this , it is not surprising that the only recent report suggesting no major ill effect of solitary confinement (Walters, 1963) utilized prisoners who volunteered to spend four days in solitary confinement. Individual Differences in Response Several authors have directed attention to the fact that within a given experimental format, massive differences in response can be observed among individual subjects. Often subjects who tolerated the experimental situation well reported pleasant, or at least non-threatening, visual imagery, fantasy, and hallucinatory experiences: "His mind may begin to wander, engage in daydreams, slip off into hypnogogic reveries with their attendant vivid pictorial images ... he may be quietly having sexual and other pleasurable thoughts. (Wright & Abbey, 1965, p. 6) On the other hand: "Another subject in the same situation may deal with it in quite another manner. He may soon complain of all manner of things: the bed is causing him a backache, his mind is a blank,... intense boredom, tenseness, depressive feelings or of having unpleasant thoughts or picture-like images that disturb him." (Goldberger, 1966, p. 777) DECLARATION OF DR. STUART GRASSIAN 23 In response to these concerns about the incidence of psychopathological reactions to sensory deprivation, an important thrust of the experimentation in this area has been, by prescreening, to select as subjects only those persons demonstrating, by some measure, psychological strength and capacity to tolerate regression. The theoretical premise of such work has been, as Goldberger (1966) states: "In the sensory deprivation experiments, it is the ego's autonomy from the drives that is predominately involved. ... Differences in drive-discharge thresholds, phantasy, and daydream capacity, capacity for what Kris has termed "regression in the service of the ego" are other theoretically relevant structural dimensions accounting for differences in isolation behavior." (p. 778) These ideas have been subjected to experimental verification, which has corroborated that same individuals tolerate such isolation better than others. For example, Wright and Abbey (1965) using the Rohrshach Test for prescreening, concluded that: "[The Rohrshach] manifestations of an individual's defense and control mechanisms ... appears to be a reliable measure for predicting whether or not an individual will be effective in controlling the drive-dominated responses that might emerge during his period of reduced sensory stimulation." (Wright & Abbey, 1965, p. 37) Anecdotal reports in a similar vein appear from time to time in the literature. Freedman and Greenblatt (1960) mention one subject who became panicky during sensory deprivation and stated he had been diagnosed "borderline psychotic" (p. 1489). Curtis reports on a psychotic paranoid reaction in one subject who suffered delusions for several days afterwards, and severe anxiety and depression lasting several weeks; personality test prescreening had suggested "poor adjustment, hostility, lack of insight, and insecurity in interpersonal relationships" (Curtis & Zuckerman, 1968, p. 256). Grunebaum, Freeman, and Greenblatt (1960), prescreened 43 subjects and identified 7 as suffering "personality deviations." Two of these subjects, who were diagnosed as borderline, developed frightening, aggressive fantasies, paranoia, and difficulty in reality testing; one of them prematurely terminated the experiment. Two others were diagnosed as psychopathic; both forced the premature termination of the experiment by disruptive behavior. Azima and Kramer (1956), using interview techniques and formal psychological test data, studied the effects of 2 to 6 days of sensory deprivation on hospitalized psychiatric patients. Among the previously non-psychotic patients they studied, two developed overt paranoid psychoses during the experiment, ultimately necessitating electroshock treatment. These particular individuals appeared to have been unable to tolerate the emergence of aggressive fantasies and images during the sensory deprivation experience. Effects of Sensory Deprivation on Antisocial Personality Disorder: "Aversive Conditioning" Individuals with psychopathic personality disorder are probably among the least tolerant of sensory deprivation. Quay (1965) actually described the essential core of psychopathic pathology as a pathological inability to tolerate restricted environmental stimulation: "The psychopath is almost universally characterized as pathologically stimulus seeking and highly impulsive. ... He is unable to tolerate routine and boredom. ... (His) DECLARATION OF DR. STUART GRASSIAN 24 outbursts frequently appear to be motivated by little more than a need for thrill and excitement. ... It is the impulsivity and lack of even minimal tolerance for sameness which appear to be the primary and distinctive features of the disorder." (p. 180) He goes on to argue that psychopathic individuals may chronically exist in a state of relative stimulus deprivation: "Highly impulsive psychopathic behavior [may be seen] in terms of stimulation seeking pathology. Decreased reactivity and/or rapid adaptation [to environmental stimuli]... produce in these persons an affective state ... close to that produced by sensory deprivation in the normal individual. He argues that behavioral impulsivity in such individuals may be an effort at coping with this condition of relative sensory deprivation which they experience: "It may be possible to view much of the impulsivity of the psychopath, his need to create excitement and adventure, his thrill seeking behavior, and his inability to tolerate routine and boredom as a manifestation of an inordinate need for an increased or changing pattern of stimulation." (p. 181) In a later study, directly comparing psychopathic inmates with non-psychopathic controls, Emmons & Webb (1974) corroborated these findings; the psychopathic inmates scored significantly higher on measures of boredom susceptibility and of impulsivity. The authors concluded that psychopaths are pathologically stimulation seeking and incapable of tolerating isolation conditions. In a large scale study of criminal offenders suffering from mental illness, Cota & Hodgins (1990) noted that the prevalence rate of severe mental illness is higher among incarcerated offenders than among the general population; and that, compared with non-mentally ill inmates, the mentally ill inmates were more likely to be housed in solitary. (p. 271) Moreover many of these mentally ill inmates suffered from a combination of psychiatric disorders predisposing them to both psychotic breakdown and to extreme impulsivity (often including substance abuse). (p. 272). Such individuals tended to be highly impulsive, lacking in internal controls, and tended to engage in self-abusive and self-destructive behavior in the prison setting, and especially so when housed in solitary. Many of the inmates placed in solitary confinement are thus likely to be among the least capable of tolerating the experience, and among the most likely to suffer behavioral deterioration as a consequence of such confinement. Solitary confinement has at times been rationalized as being a form of "Aversive Conditioning", intended to extinguish negative inmate behaviors. Yet this assertion ignores many of the most basic tenets of any behavior modification treatment, and would in any case clearly violate the ethical guidelines governing the use of aversive conditioning: 1. Ethical Considerations: First of all, since aversive conditioning -- the use of punishment as a means of inducing behavior change - is inherently suspect ethically, and creates an inherent risk of harm, very clear outcome variables have to be articulated and systematically measured over time. (Foxx, Plaska and Bittle, 1986; AABT Task Force 1982) As a result of these serial measurements, there must be clear evidence that the undesirable behavior is in fact lessening in frequency and intensity. Such measurement will also identify those patients for whom such aversive conditioning is actually harmful, allowing these individuals to be removed from the aversive treatment protocol. Were such measurements done in the prison setting, staff would inevitably be required to acknowledge the behavioral deterioration which many inmates were suffering as a result of placement in solitary, and in such c ases, ethical considerations would have required transferring the inmate out of such confinement. DECLARATION OF DR. STUART GRASSIAN 25 2. SHU Incarceration is Not Aversive Conditioning: And moreover, SHU incarceration does not meet criteria for aversive conditioning. (Personal Communication; 1993 Drs. R. Worshan and M. Israel) (AABT; 1982 Foxx et al., 1986) Indeed, any behavior modification scheme must define and describe very explicitly two variables: (a) The behavior being changed: Behavior researchers have learned that in order for a subject to benefit from aversive (or any other form of) conditioning, the behavior at issue must be a single, very clearly defined behavior. When multiple behaviors are responded to by the same reinforcer or punishment, learning and behavior change does not occur. Thus, placement in SHU which is "punishment" for a host of different behaviors, is simply not being used in a manner consistent with an intent of behavior modification; there is inadequate linkage of any specific behavior to this "punishment." (b) The "punishment": Moreover, SHU confinement is quite clearly not "punishment" as defined by aversive conditioning experts. (Personal Communication: Drs. R. Worsham and M. Israel, 1993) To be effective, a "punishment" must be very closely linked in time to the targeted behavior, and for learning to occur, there must be repeated opportunities to experience this close link between the target behavior and the punishment. Thus, the "punishment" must be brief, and immediate. For example, a mild but painful electric shock, a sudden very loud noise, would be ideal punishments in aversive conditioning. Occasionally, "time outs" the brief use of a seclusion room to quickly control disruptive behavior -- are used as part of an aversive conditioning program. But when this technique is employed, it is used very quickly and for a very brief period of time -- in order for the "time out" to work as a behavior modifier, there must be very clear alternative behaviors which, when manifested, will immediately end the "time out." For any behavior modification scheme to work, then there must always be an exquisitely close relationship between behavior and response. Indeterminate or prolonged sentencing to solitary simply has nothing to do with aversive conditioning. DECLARATION OF DR. STUART GRASSIAN 26 REPORTS OF THE LONG-TERM EFFECTS OF SOLITARY CONFINEMENT IN FORMER POLITICAL PRISONERS AND IN PRISONERS OF WAR: SOLITARY CONFINEMENT AS A MEANS OF "BRAIN WASHING" AND "INDOCTRINATING" Although concerns about the psychiatric effects of solitary confinement among prisoners of war were raised in the medical literature at least as early as post World War II, this issue reached massive public exposure only after the fearful news of "brainwashing" among American prisoners of war in Korea. As is well known, the 1950's were an era of tremendous fear of Communism and of the attempts by Communist States to "indoctrinate" people into their ideology. As noted in the body of this declaration, in the 1950's the U.S. Department of Defense and Central Intelligence Agency sponsored a great deal of research on these issues; Hinkle and Wolff (1956) published results of extensive research done by them for the Department of Defense. The paper documented interrogation techniques of the Soviet KGB in regard to the incarceration of political prisoners, and the Chinese communists' imprisonment of American prisoners of war in Korea. The report indicated that the KGB operated detention prisons, many of which were "modern . . . well built and spotlessly clean . . . (with) attached medical facilities and rooms for the care of sick detainees. An exercise yard is a standard facility. Incarceration in these prisons is almost universally in solitary confinement in a cell approximately 10' x 6' in size. An almost invariable feature of the management of any important suspect under detention is a period of total isolation in a detention cell." (p. 126) This isolation was seen as a central feature of the imprisonment: "The effects upon prisoners of the regimen in the isolation cell are striking. ... A major aspect of this prison experience is isolation. ... (In the cells) his internal as well as external life is disrupted (and) ... he develops a predictable group of symptoms, which might almost be called 'disease syndrome.'" This syndrome develops over time: "He becomes increasingly anxious and restless and his sleep is disturbed ... The period of anxiety, hyperactivity, and apparent adjustment to the isolation routine usually continues from 1 to 3 weeks. ... The prisoner becomes increasingly dejected and dependent. He gradually gives up all spontaneous activity within his cell and ceases to care about personal appearance and actions. Finally, he sits and stares with a vacant expression, perhaps endlessly twisting a button on his coat. He allows himself to become dirty and disheveled. ... He goes through the motions of his prison routine automatically, as if he were in a daze. ... Ultimately, he seems to lose many of the restraints of ordinary behavior. He may soil himself; he weeps; he mutters. ... It usually takes from 4 to 6 weeks to produce this phenomenon in a newly imprisoned man. ... His sleep is disturbed by nightmares. Ultimately he may reach a state of depression in which he ceases to care about his personal appearance and behavior and pays very little attention to his surroundings. In this state the prisoner may have illusory experiences. A distant sound in the corridor sounds like someone calling his name. The rattle of a footstep may be interpreted as a key in the lock opening the cell. Some prisoners may become delirious and have visual hallucinations. Not all men who first experience total isolation react in precisely this manner. In some, the symptoms are less conspicuous. In others, dejection and other despondence earlier, or later. Still others, and especially those with preexisting personality disturbances, may become frankly psychotic." (p. 129) DECLARATION OF DR. STUART GRASSIAN 27 The authors note that the procedures in the Chinese detention camps are somewhat more complex. Prisoners there underwent an initial period of isolation similar to that found in the Soviet prisons. (p. 153) In the second phase, however they were housed in extremely tight quarters within "group cells" comprising approximately eight prisoners. Under the tensions and hostilities created in this environment, brutality of prisoners against other prisoners was almost inevitable and was, according to the authors, apparently an intended result of this "group cell" confinement. (p. 159) There are many long-term studies of American prisoners of war; unfortunately, the factor of solitary confinement has not generally been separated out in these studies. However, one relatively recent study of Korean POWs describe long-term effects including interpersonal withdrawal and suspiciousness, confusion, chronic depression and apathy towards environmental stimuli. Irritability, restlessness, cognitive impairment and psychosomatic ailments were extremely common in the group, most of whom had suffered periods of incarceration in solitary confinement at the hands of the Chinese. This report also included a case report of one individual exposed to harsh conditions of solitary confinement for more than 16 months; 30 years after release, he continued suffering sleep disturbances, nightmares, fearfulness, interpersonal suspicion and withdrawal, severe anxiety and severe depression. These former prisoners also had psychosomatic ailments including gastrointestinal disturbances, chronic headaches and obsessive ruminations. They tended to become confused and thus cognitively impaired and were emotionally volatile and explosive. In a more recent study, Sutker et al. (1991) studied former prisoners of war in the Korean conflict, approximately 40 years after their release from confinement. Solitary confinement was cited as one of the severe stressors in this group. These former prisoners demonstrated persistent anxiety, psychosomatic ailments, suspiciousness, confusion, and depression. They tended to be estranged and detached from social interaction, suffered from obsessional ruminations, and tended to become confused and cognitively impaired, suffering memory and concentration difficulties which affected their cognitive performance on formal testing. DECLARATION OF DR. STUART GRASSIAN 28 Altshuler, K.Z., (1971). Studies of the deaf: Relevance to Psychiatric Theory. American Journal of Psychiatry, 127(11), 1521-1526. American Psychiatric Association (1986). Diagnostic and Statistical Manual of Mental Disorders, III-R, Washington, D.C., A.P.A. Publishing. Arieti, S. (1974) The American Handbook of Psychiatry, Second Edition. New York, Basic Books. Association for the Advancement of Behavior Therapy (1982). The Treatment of Self-Injurious Behavior. Behavior Therapy, 13, 529-534. Barnes, T.C. (1959). Isolation stress in rats and mice as a neuropharmacological test. Federal Proceedings, 18, 365. Bennett, A.M.H. (1961). Sensory Deprivation in Aviation. In Sensory Deprivation, Solomon, P., Kubzansky, P.E., Leiderman, P.H., Mendelson, J.H., Trumbull, R., & Wexler, D. (Eds.). Cambridge, MA: Harvard University Press. Biderman, A. & Zimmer, H., eds. (1961). The Manipulation of Human Behavior. New York, John Wiley & Sons, Inc. Biersner, R.J., & Hogan, R. (Hogan). Personality correlates of adjustment in isolated work groups. Journal of Research in Personality, 18, 491-496. Brownfield, C. (1965). Isolation: Clinical and Experimental Approaches. New York, Random House. Burney, C. (1952). Solitary Confinement London, Colin MacMillan. Clark, B. & Graybiel, A. (1957). The break-off phenomenon: A felling of separation from the earth experienced by pilots at high altitudes. Journal of Aviation Medicine, 28, 121. Cochrane, J.J., & Freeman, S.J.J., (1989). Working in Arctic and sub-arctic conditions: Mental health issues. Canadian Journal of Psychiatry, 34, 884-890. Cota, G., & Hodins, S. (1990). "Co-occurring mental disorders among criminal offenders." Bulletin of the American Academy of Psychiatry and Law, 18, (3), 271-281. Curtis, G. & Zuckerman, M. (1968). "A psychopathological reaction precipitated by sensory deprivation." American Journal of Psychiatry, 125, 255-260. Downs, F. (1974). Bed rest and sensory disturbances. American Journal of Nursing, 74(3), 434-438. Egerton, N., & Kay, J.H. (1964). Psychological disturbances associated with open heart surgery. British Journal of Psychiatry, 110, 433-439. Ellis, R. (1972). Unusual sensory and thought disturbances after cardiac surgery. American Journal of Nursing, 72(11), 2021-2025. Emmons, T., & Webb, W. (1974). "Subjective correlates to emotional responsivity and stimulation seeking in psychopaths, normals and acting out neurotics." Journal of Consulting & Clinical Psychology, 42, (4), 620-631. DECLARATION OF DR. STUART GRASSIAN 29 Foxx, R.M. Plaska, T.G. & Bittle, R.G., (1986). Guidelines for the use of Contingent Electric Shock to Contingent Treat Abberant Behavior. Progress in Behavior Modification, 20, 1-36. Freedman, S. & Greenblatt, M. (1960). "Studies in Human Isolation IV: Hallucinations and Other Cognitive Findings." U.S. Armed Forces Medical Journal, 11, 1479-1497. Ganser, J. (1898) Uber einen eigenartigen hysterischen Dammerzustand. Archives Psychiat Nervenk 30:633-640. Goldberger, L. (1966). "Experimental Isolation: An Overview." American Journal of Psychiatry, 122, 774782. Goldstein, A.G. (1976). Hallucinatory experience: A personal account. Journal of Abnormal Psychology, 85(4), 423-429. Grassian, S. (1983). "Psychopathological Effects of Solitary Confinement." American Journal of Psychiatry, 140, 1450-1454. Grassian, S., & Friedman, N. (1986). "Effects of Sensory Deprivation in Psychiatric Seclusion and Solitary Confinement." International Journal of Law and Psychiatry, 8, 49-65. Gunderson, E.K. (1963). Emotional symptoms in extremely isolated groups. Archives of General Psychiatry, 9, 362-368. Gunderson, E.K., & Nelson, P.D. (1963). Adaptation of small groups to extreme environments. Aerospace Medicine, 34, 1111-1115. Harlow, H.F., & Suomi, S.J. (1974). Induced depression in monkeys. Behavioral Biology, 12, 273-296. Hinkle, L. & Wolf, H. (1956). Communist Interrogation and Indoctrination of `Enemies of the States': Analysis of Methods Used by the Communist State Police. Archives of Neurology and Psychiatry (Vol. 1956, pp. 115-174). Holroyd, S. Rabins, P.V., Finkelstein, D., Nicholson, M.C., Chase, G.A., Wisniewski, S.C. (1992). Visual hallucinations in patients with muscular degeneration. American Journal of Psychiatry, 149(12), 17011706. Houston, F., & Royse, A.B. (1954). Relationship between deafness and psychotic illness. Journal of Mental Science, 990-993. Ingraham, M. & Moriarity, D. (1967). A contribution to the understanding of the Ganser Syndrome. Comprehensive Psychiatry, 8, 35-44. Jackson, C.W., Jr. (1969). Clinical sensory deprivation. A review of hospitalized eye patients. In J.P. Zubek (Ed.), Sensory deprivation: Fifteen years of research. New York: Appleton-Century-Crofts. Kerkhof, J.F.M., & Bernasco, W. (1990). "Suicidal behavior in jails and prisons in the Netherlands. Incidents, characteristics & prevention." Suicide & Life Threatening Behavior, 20, (2), 123-137. Klein, H., & Moses, R. (1974). Psychological reaction to sensory deprivation in patients with ablatio retinae. Psychotherapy and Psychosomatics, 24, 41-52. DECLARATION OF DR. STUART GRASSIAN 30 Kornfeld, D.S., Zimberg, S., & Malm, J.R. (1965). Psychiatric complications of open-heart surgery. New England Journal of Medicine, 273(6), 287-292. Lazarus, H.R., & Hagens, J.H. (1968). Prevention of psychosis following open-heart surgery. American Journal of Psychiatry, 124(9), 1190-1195. Lee, R.E., & Ball, P.A. (1975). Some thoughts on the psychology of the coronary care unit patient. American Journal of Nursing, 75(9), 1498-1501. Liederman, P. (1976). Sensory deprivation: Clinical aspects. Archives of Internal Medicine, 101(2), 389396. Liederman, P. (1962). Man Alone: Sensory Deprivation and Behavior Change. Correctional Psychiatry and Journal of Social Therapy, 8:64-72. Lilly, J. (1956). Mental effects of reduction of ordinary levels of physical stimuli on intact, healthy persons. Psychiatric Research Reports, 5, 1-9. Matsumoto, K., Cai, B., Satoh, T., Ohta, H., & Watanabe, H. (1991). Desipramine enhances isolationinduced aggressive behavior in mice. Pharmacology Biochemistry and Behavior, 39, 167-170. May, R., Voegele, G. & Paolino, A. (1960). The Ganser Syndrome. A report of three cases. Journal of Nervous & Mental Diseases, 130, 331-339. McFarland, R.A. and Moore, R. "Human Factors in Highway Safety: A Review and Evaluation." New Eng. J. Med., 256: 792-798, 815-837, 890-897, 1957. McKinney, W.T., Jr., Suomi, S.J., & Harlow, H.F. (1971). Depression in primates. American Journal of Psychiatry, 127(10, 1313-1320. Meltzer, M. (1956). Solitary Confinement. in GAP (Group for the Advancement of Psychiatry) Symposium #3: Factors Used to Increase the Susceptibility of Individual to Forceful Indoctrination. New York. Mullin, C.S., & Connery, H.J.M. (1959). Psychological study at an Antarctic IGY Station. Armed Forces Medical Journal, 10, 290-296. Nitsche, P., Willaims K. (1912). The History of the Prison Psychoses. New York, Nervous and Mental Disease Publishing Company. Orne, M., & Scheibe, K. (1964). "The contribution of nondeprivation factors in the production of sensory deprivation effects: the psychology of the "panic button." Journal of Abnormal & Social Psychology, 68, 3-12. Personal Communication (Sept. 1993): Drs. Matthew Israel and Bob Worsham, Behavioral Research Institute, Providence, Rhode Island. Quay, H. (1965). "Psychopathic personality as pathological stimulation seeking. "American Journal of Psychiatry, 122, 180-183. Riestin, A. (1961). Excessive arousal effects of stimulation after early sensory deprivation. In Sensory Deprivation, Solomon, P., Kubzansky, P.E., Leiderman, P.H., Mendelson, J.H., Trumbull, R., & Wexler, D. (Eds.). Cambridge, MA: Harvard University Press. DECLARATION OF DR. STUART GRASSIAN 31 Rothblum, E.D., (1990). Psychological Factors in the Antartic. Journal of Psychology, 124(3), 253-273. Rothman, D., (1971). The Discovery of the Asylum. Boston. Little Brown & Company Schultz-Ross, R.A. (1993). "Theoretical difficulties in the treatment of mutually ill prisoners." Journal of Forensic Sciences, 38(2), 426-431. Solomon, P., et. al. (1961). Sensory Deprivation: A Symposium held at Harvard Medical School. Cambridge, MA, Harvard University Press. Strange, R.E., & Klein, W.J. (1974). Emotional and social adjustment of recent U.S. winter-over parties is isolated Antarctic stations. Antarctic Bibliography, 7, 229. Sutker, P. et al. (1991). Cognitive Deficits and Psychopathology Among Former Prisoners of War and Combat Veterans of the Korean Conflict. American Journal of Psychiatry, 148:1, 67-72. Thomson, L.R. (1973). Sensory deprivation: A personal experience. American Journal of Nursing, 73(2), 266-268. Thompson, W.R., & Melzack, R. (1956). Early environment. Scientific American, 194, 38-42. Tyndel, M. (1956). Some aspects of the Ganser state. Journal of Mental Sciences. 102, 324-329. Walters, R. (1963). "Effects of Solitary Confinement on Prisons. "American Journal of Psychiatry," 119, 771-773. Washburn, D.A., & Rumbaugh, D.M. (1991). Impaired performance from brief social isolation of rhesus monkeys (Macaca mulatta): A multiple video-task assessment. Journal of Comparative Psychology, 105(2), 145-151. Weiner, H. & Braiman, A. (1955). The Ganser Syndrome. American Journal of Psychiatry, 11, 767-773. Wilson, L.M. (1972). Intensive care delirium. Archives of Internal Medicine, 130, 225-226. Woodruff, R., Goodwin, D., & Guze, S. (1974). Psychiatric Diagnosis. New York, Oxford University Press. Wright, M.W., Chylinski, J., Sisler, G.C., & Quarrington, B. (1967). Personality factors in the selection of civilians for isolated northern stations: A follow-up study. Canadian Psychologist, 8, 23-31. Wright, N., & Abbey, D. (1965). "Perceptual Deprivation Tolerance and Adequacy of Defenses." Journal of Perceptual Motor Skills, 20, 35-38. Zimbardo, P.G., Andersen, S.M., & Kabat, L.G. (1981). Induced hearing deficit generates experimental paranoia. Science, 212, 1529-1531. Ziskind, E. (1958). Isolation stress in medical and mental illness. Journal of the American Medical Association, 168(11), 1427-1431. Ziskind, E., Jones, H., Filante, W., & Goldberg, J. (1960). Observations on mental symptoms in eye patched patients: Hypnagogic symptoms in sensory deprivation. American Journal of Psychiatry, 116, 893-900. Zubek, J.P. (1969). Sensory deprivation: Fifteen years of research. New York: Appleton-Century-Crofts. DECLARATION OF DR. STUART GRASSIAN 32