RECOMMENDATIONS FOR PRIORITIZATION AND DISTRIBUTION OF COVID-19 VACCINE IN PRISONS AND JAILS
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
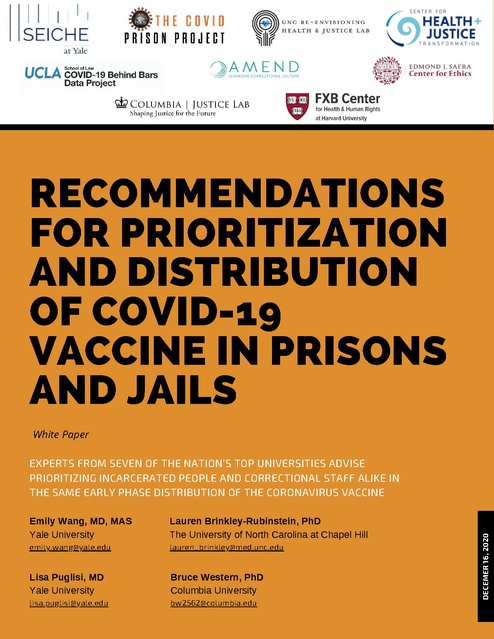
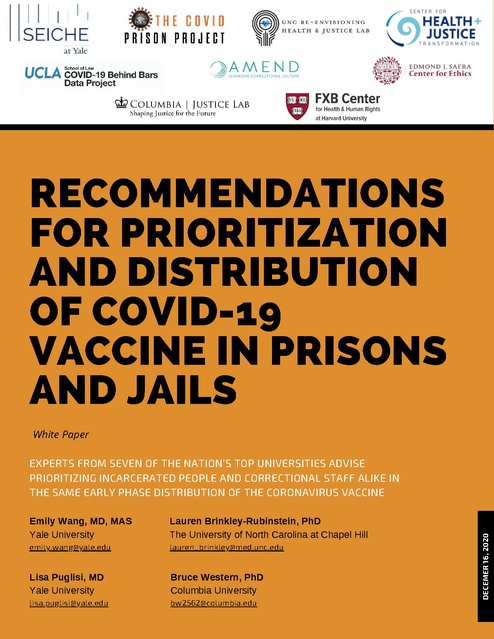
RECOMMENDATIONS FOR PRIORITIZATION AND DISTRIBUTION OF COVID-19 VACCINE IN PRISONS AND JAILS White Paper Emily Wang, MD, MAS Yale University Lauren Brinkley-Rubinstein, PhD The University of North Carolina at Chapel Hill emily.wang@yale.edu lauren_brinkley@med.unc.edu Lisa Puglisi, MD Yale University Bruce Western, PhD Columbia University lisa.puglisi@yale.edu bw2562@columbia.edu DECEMER 16, 2020 EXPERTS FROM SEVEN OF THE NATION’S TOP UNIVERSITIES ADVISE PRIORITIZING INCARCERATED PEOPLE AND CORRECTIONAL STAFF ALIKE IN THE SAME EARLY PHASE DISTRIBUTION OF THE CORONAVIRUS VACCINE Recommendations for Prioritization and Distribution of COVID-19 Vaccine in Prisons and Jails Emily Wang, MD, MAS Yale University emily.wang@yale.edu Lauren Brinkley-Rubinstein, PhD The University of North Carolina at Chapel Hill lauren_brinkley@med.unc.edu Lisa Puglisi, MD Yale University lisa.puglisi@yale.edu Bruce Western, PhD Columbia University bw2562@columbia.edu Prisons and jails across the country have been epicenters of the COVID-19 pandemic. Since the beginning of the pandemic, correctional facilities have accounted for a majority of the largest single-site, cluster outbreaks across the country. Nearly 20% of the prison population has tested positive for COVID-19, with an infection rate that is higher than five times and an age-adjusted mortality rate that is three times that of the general population. Yet, to date, recommendations on vaccine distribution, set forth by the Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices, have not given incarcerated people priority in COVID-19 vaccine distribution. This is in stark contrast to the explicit and appropriate prioritization of people in long-term care facilities, another group that has experienced marked rates of COVID-19 and resultant morbidity and mortality. Prisons and jails are not places apart from the community. Outbreaks in correctional facilities spill over to the community and further burden health care systems that are overtaxed, especially in rural communities with local jails. That is why we conclude that prioritization for vaccination for those who live and work in correctional systems is critical to public health. This white paper describes the rationale and details the following four recommendations: States should prioritize vaccine distribution to all incarcerated people at the same stage as correctional officers (essential workers/first responders) 1. or higher; States should create vaccine distribution and implementation plans developed by medical & public health professionals that are specific to correctional 2. systems; 3. State advisory vaccine groups should have correctional healthcare, administrative leadership, and justice-involved individuals in committees; 4. States should identify policies and methods to effectively fund vaccine distribution and administration in correctional systems and following release. The Challenge Efforts to prevent and control the transmission of SARS-CoV-2, the novel coronavirus, have met many challenges in correctional systems. It is nearly impossible to implement physical distancing inside facilities with congregate, dormitory-style housing or in facilities that are overcrowded, old, or poorly ventilated. Hygiene standards, infection control, and mask wearing are difficult to maintain and enforce. Irregular testing, inadequate medical resources, siloed healthcare systems, the movement of correctional staff between home and work, and the churn of admissions and releases from incarceration further amplify transmission. And, because incarcerated people suffer disproportionately from conditions such as hypertension and asthma, they are more likely to experience COVID-19 complications and death. December 16, 2020 page 1 of 4 Despite being a focal point of the pandemic and past outbreaks, correctional facilities have not always been included in pandemic planning. This same pattern has emerged with vaccine distribution. Unlike in nursing homes and other long-term care facilities, which are also sources of outbreaks, prisons and jails are not consistently being prioritized for vaccine distribution (see Figure below). They have also not received the federal support for vaccine allocation that long-term care facilities have received, which would reduce the burden on the facilities themselves and local health departments. Criteria for Prioritizing COVID-19 Vaccine Distribution in Prisons and Jails The Advisory Committee on Immunization Practices has provided interim guidance to the federal government and states on allocation of the initial doses of COVID-19 vaccine. They prioritized health care workers and residents of long-term care facilities. Thus far, incarcerated people have not been prioritized for initial allocation. This is despite the fact that they too reside in congregate settings and are subject to a risk of exposure to COVID-19 in jails and prisons that is extremely high, on par with that of other congregate living facilities that have been prioritized. The state and federal government must provide healthcare in correctional facilities that is commensurate with the community standard of care. Under pandemic conditions, this means prioritizing people at highest risk. Given the epidemiology of infection and the responsibility of the government for adequate healthcare standards in prisons and jails, prioritization of vaccine distribution for incarcerated people is critical. When the Advisory Committee on Immunization Practices meet next, they are expected to consider essential workers in the next phase of the vaccine distribution. The U.S. Cybersecurity and Infrastructure Security Agency has identified correctional officers as essential workers, which means they would be considered one of the high-priority populations to receive early administration of vaccine if the CDC and states adopt these recommendations. Additionally, correctional staff that work in healthcare settings, including clinicians, nurses, therapists, environmental service workers, given their occupational risks, ought to be included in the earliest allocation along with all other healthcare workers. We recommend following an approach devised by the National Academies of Science, Engineering and Medicine (NASEM), in their report entitled, “A Framework for Equitable Allocation of Vaccine for the Novel Coronavirus.” NASEM uses the following criteria to justify prioritization of populations at severe risk of COVID-19, depending on the risk they face of: 1. 2. 3. 4. acquiring infection, severe morbidity and mortality, negative societal impact, and transmitting infection to others. Because incarcerated people and correctional staff rank high in at least three of these criteria, NASEM highly prioritized both groups for the vaccine. Prioritizing vaccines for those who live and work in corrections will reduce serious complications from COVID-19 in correctional settings and may also reduce transmission to surrounding communities. The American Medical Association has also affirmed that designating correctional staff and incarcerated people as high-priority populations for the vaccine will protect them and their communities from COVID-19 outbreaks. This presents an opportunity for a large public health impact by vaccinating a relatively small number of people (1.5 million currently in U.S. prisons and 5 million who will pass through local jails over the next six months). At the state level, prison populations and correctional officers will represent a small percentage of overall vaccine allocations. Review of States’ Interim Vaccine Plans While national guidance on vaccine prioritization exists, ultimately vaccines are allocated directly to states, which have been charged with developing distribution plans that reflect local needs. States submitted their vaccine prioritization plans to the CDC on December 4, 2020, which are draft plans that can still be adapted. A review of the plans for all available states and Puerto Rico, conducted by the COVID Prison Project, shows significant variation. page 2 of 4 Interim Plans for Vaccine Distribution WA MT VT ND ME MN OR ID WI SD NV UT AZ CO IL KS OK NM PA IA NE MO WV KY VA TN NJ DE MD Phase 1: Highest Priority Population Phase 2: Medium Priority Population Phase 3: Lowest Priority Population SC AL No Phase: Not Included in Plans GA UNAVAILABLE: No Plan Currently Available LA FL AK CT RI NC AR MS TX OH IN MA NY MI WY CA NH PR HI Source: COVID Prison Project (2020). https://covidprisonproject.com/ Source: Michaud, J., Kates, J., Dolan, R., & Tolbert, J. (2020). States are getting ready to distribute COVID-19 vaccines. What do their plans tell us so far? - State plans. Retrieved from: https://www.kff.org/report-section/states-are-getting-ready-to-distribute-covid-19-vaccines-what-do-their-plans-tell-us-so-far-state-plans/ As of December 15, 2020, 12 states/territories have included incarcerated population as part of their Phase 1 vaccine distribution; 24 states included incarcerated populations as part of their Phase 2 vaccine distribution. In Missouri, incarcerated people were identified as targets for Phase 3 while correctional staff were targeted for Phase 1. And in 11 states, they were not included explicitly in any part of the plan. States can continue to modify these plans. In recent days, some states made their plans more specific and included incarcerated people in phase 1 after having considered them in lower phases. It is not too late to prioritize incarcerated people and staff now. Other states still have time to follow this best practice in vaccine priority. Recommendations 1) States should prioritize vaccine distribution to all incarcerated people at the same stage as correctional officers (essential workers/first responders) or higher. People who work and live in jails and prisons are at high risk for getting COVID-19 and experiencing severe illness and death. A randomized trial of the Pfizer-BioNtech vaccine demonstrated 95% efficacy at reducing symptomatic and severe illness. Rapid deployment of the vaccine would significantly improve safety in a setting with a very high risk of extreme suffering and death. The best empirical evidence indicates that the risk of COVID-19 is in fact higher for incarcerated people than for correctional staff. Thus, the medical necessity for vaccinating incarcerated people is at least as great, as for staff. Further, prioritizing staff over incarcerated people (or vice versa) can also create tensions between incarcerated people and staff and can stoke further mistrust of vaccines beyond the prison gates. A survey commissioned by Pew Center of States found that 49% of participants would not get vaccinated initially, and these rates are highest among Black and Latinx communities, which have been neglected and discriminated against by the healthcare system at large. Improving health equity in the impact of COVID-19 on Black, Latinx and Indigenous communities is impossible without prioritizing incarcerated people early in vaccine distribution plans. page 3 of 4 2) States should create vaccine distribution and implementation plans developed by medical and public health professionals that are specific to correctional systems. Of the two vaccines that have concluded phase three clinical trials (Pfizer-BioNTech and Moderna), cold-chain vaccine distribution (delivering the vaccine at recommended low temperatures) and administration of COVID-19 vaccines (two shots separated by 3-4 weeks) may be a challenge for many correctional systems and especially for jails that have high levels of population turnover among people with relatively short lengths of stay. Vaccine administration plans will need to account for follow-up shots in the community for those who are being released from incarceration prior to the second dose. The challenges inherent in wide-scale vaccine deployment should not supersede the public health imperative to prioritize this group. The responsibilities for vaccine distribution and administration should not lie entirely with Departments of Correction or local jails, many of which have staffing shortages and strained health services. There are national examples of large-scale collaboration between pharmacy companies like CVS and Walgreens and the government to distribute vaccines to all people in long-term care facilities. Such partnerships with large pharmacy plans at the state level should be considered to address logistical challenges in corrections, especially rural jails. Finally, public health and behavioral scientists who are experts in vaccine hesitancy should be consulted to determine how best to increase COVID-19 vaccine uptake rates. 3) State advisory vaccine groups should have correctional healthcare, administrative leadership, and justice-involved individuals in committees. Statewide vaccine distribution plans must be informed by the realities and needs in correctional settings. All governors have convened vaccine advisory groups, many of which do not include the expertise of those who live or work in correctional systems. Their expertise will enable states to anticipate problems and identify solutions for vaccine distribution challenges that pertain to prisons and jails. A sub-committee of a vaccine advisory group focused on corrections could then be the foundation for longer lasting partnerships with local departments of health, which prepare for future waves of this and future pandemics. The FDA has been working with the Vaccine Confidence Project to increase uptake of the COVID-19 vaccine mainly via focus groups with under-represented communities. The ethos espoused by the Vaccine Confidence Project centers on the following tenets: listen, engage, innovate, and co-create. Utilizing these guideposts, and including incarcerated people and correctional leadership in planning, will ensure successful deployment of vaccines and increased uptake. 4) States should identify policies and methods to effectively fund vaccine distribution and administration in correctional systems and following release. The correctional healthcare system is separated from public health and emergency preparedness planning and has not been resourced to manage pandemic outbreaks. As a result, during this pandemic, some facilities did not have the resources to obtain timely tests, personal protective equipment, or sanitation supplies. Some relied on paper medical records and could not identify who were most at risk. When correctional facilities are fully staffed and have the capacity and technology to implement an efficient, facility-wide vaccine campaign, they can ensure better outcomes. Under the Centers of Medicare & Medicaid Services (CMS) administrative rules, states can initiate programs or policies, which include covering the costs of SARS-CoV-2 health needs, including vaccination implementation. These programs also would facilitate smooth transition of care to individuals who were released after one vaccine dose and needed the second in the community. To maximize healthcare coverage of incarcerated and formerly-incarcerated people, Medicaid coverage should also be expanded with waivers under Sections 1115 of the Social Security Act to extend the scope of services to incarcerated people during the COVID-19 emergency to cover testing or vaccine administration costs. Lastly, wholesale expansion of Medicaid in the first 30 days prior to release would create a smoother transition to the community for follow-up care and a second vaccine as needed. By prioritizing incarcerated people and correctional staff in COVID-19 vaccine plans, we will better be able to stem the virus and protect our most vulnerable and the community at large. Vaccine priority is a test of our pragmatism and commitment to fairness. For these reasons vaccinating people who live and work in prisons and jails is an urgent priority. page 4 of 4