Union CI CAP Assessment, CMA-FDC Monitoring, 2015
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
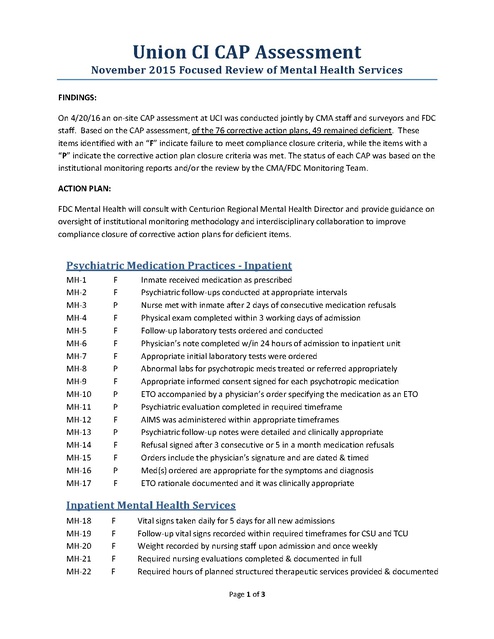
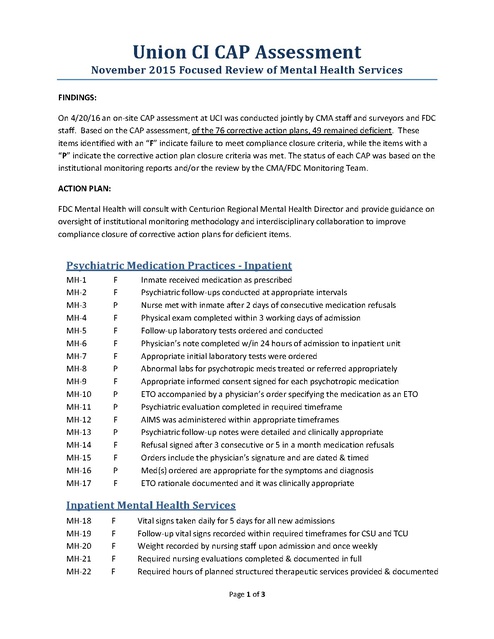
Union CI CAP Assessment November 2015 Focused Review of Mental Health Services FINDINGS: On 4/20/16 an on-site CAP assessment at UCI was conducted jointly by CMA staff and surveyors and FDC staff. Based on the CAP assessment, of the 76 corrective action plans, 49 remained deficient. These items identified with an “F” indicate failure to meet compliance closure criteria, while the items with a “P” indicate the corrective action plan closure criteria was met. The status of each CAP was based on the institutional monitoring reports and/or the review by the CMA/FDC Monitoring Team. ACTION PLAN: FDC Mental Health will consult with Centurion Regional Mental Health Director and provide guidance on oversight of institutional monitoring methodology and interdisciplinary collaboration to improve compliance closure of corrective action plans for deficient items. Psychiatric Medication Practices - Inpatient MH-1 MH-2 MH-3 MH-4 MH-5 MH-6 MH-7 MH-8 MH-9 MH-10 MH-11 MH-12 MH-13 MH-14 MH-15 MH-16 MH-17 F F P F F F F P F P P F P F F P F Inmate received medication as prescribed Psychiatric follow-ups conducted at appropriate intervals Nurse met with inmate after 2 days of consecutive medication refusals Physical exam completed within 3 working days of admission Follow-up laboratory tests ordered and conducted Physician’s note completed w/in 24 hours of admission to inpatient unit Appropriate initial laboratory tests were ordered Abnormal labs for psychotropic meds treated or referred appropriately Appropriate informed consent signed for each psychotropic medication ETO accompanied by a physician’s order specifying the medication as an ETO Psychiatric evaluation completed in required timeframe AIMS was administered within appropriate timeframes Psychiatric follow-up notes were detailed and clinically appropriate Refusal signed after 3 consecutive or 5 in a month medication refusals Orders include the physician’s signature and are dated & timed Med(s) ordered are appropriate for the symptoms and diagnosis ETO rationale documented and it was clinically appropriate Inpatient Mental Health Services MH-18 MH-19 MH-20 MH-21 MH-22 F F F F F Vital signs taken daily for 5 days for all new admissions Follow-up vital signs recorded within required timeframes for CSU and TCU Weight recorded by nursing staff upon admission and once weekly Required nursing evaluations completed & documented in full Required hours of planned structured therapeutic services provided & documented Page 1 of 3 MH-23 MH-24 MH-25 MH-26 MH-27 MH-28 MH-29 MH-30 MH-31 MH-32 MH-33 F F F P P F P P P F F MHP notes completed timely and address progress toward ISP goals Weekly group/activity summary note completed by MHP Overall, treatment provided was appropriate MDST met to review/document Behavioral Levels w/in required timeframes Initial nursing assessment fully completed within 4 hours of admission ISP was initiated and reviewed within the appropriate timeframe Entries dated, timed, signed & stamped Nursing provided explanation for admission and orientation to the unit w/in 4 hours Vital signs were obtained within one hour of admission For CM inmates the BRA was completed accurately and is signed by MDST Discharge or transfer summary completed before CSU discharge Outpatient Mental Health Services MH-34 MH-35 MH-36 MH-37 MH-38 MH-39 MH-40 MH-41 MH-42 MH-43 MH-44 MH-45 MH-46 MH-47 MH-48 MH-49 MH-50 MH-51 MH-52 MH-53 MH-54 MH-55 P P F F P F P P P F F P P F P F F F F P F P 1 hour group or individual counseling offered per week and documented (CM only) Inmate received medication as prescribed ISP lists type and frequency of intervention, and staff responsible The BRA was completed within required timeframes (CM inmates only) Interventions and services described by ISP are documented CM referral assessment completed w/in 5 days (CM inmates only) Upon arrival current psychotropic meds continued until seen by psychiatry Frequency of clinical contacts is sufficient and clinically appropriate Counseling offered every 30 days for inmates with psychotic disorders ISP is updated w/in 14 days of placement, and is current (CM only) Appropriate informed consent signed for each psychotropic medication Psychiatric follow-up conducted at appropriate intervals After start of MH services, initial ISP completed within 30 days Identified problems are on the problem list Inmate seen by psychiatry prior to expiration of psychotropic meds MSE completed, active MH problems assessed & ISP updated w/in 14 days of arrival Nurse met with inmate after 2 days of consecutive medication refusals ISP goals are time limited and written in objective measurable behavioral terms The BRA is completed accurately and is signed by MDST members (CM only) All entries were dated, timed, signed, and stamped ISP signed by all MDST members and inmate or refusal is documented Progress notes have sufficient detail to follow course of treatment Special Housing MH-56 P Outpatient treatment is continued as indicated on the ISP Page 2 of 3 MH-57 MH-58 MH-59 MH-60 MH-61 MH-62 F P F F P P A Special Housing Health Appraisal was completed by nursing staff Psychotropic medication continued while in special housing Initial mental status exam was completed in the required timeframe & documented Follow-up mental status exams are completed in the required timeframes All entries were dated, timed, signed, and stamped Mental status exams are sufficient to identify any possible adjustment problems Discharge Planning MH-63 F Consent or refusal signed w/in 30 days after the initiation of aftercare Inmate Requests MH-64 F Interview or referral took place as responded to on inmate request SHOS MH-65 MH-66 MH-67 MH-68 MH-69 F F P F F Observations recorded on checklist every 15 minutes Nurse evaluated inmate within 2 hours of admission Daily counseling by MH staff was conducted and documented Inpatient Mental Health Daily Nursing Evaluation completed each shift All entries were dated, timed, signed, and stamped Psychiatric Restraints MH-70 MH-71 MH-72 MH-73 MH-74 MH-75 MH-76 F F F F F F F Patient’s behavior observed every 15 minutes and documented on DC4-650A Respiration & circulation checks completed and documented on DC4-650A 4-point restraints: limbs exercised every 2 hours and documented on DC4-650A Restraints removed after 30 minutes of calm behavior Less restrictive means of behavioral control attempted and documented Offered food, fluids and bedpan/urinal as required and documented on DC4-650A Vital signs taken and recorded upon release from restraints Page 3 of 3 Overview of Union CI Audit conducted 11/9/15 - 11/10/15 This was a targeted review conducted jointly by CMA staff and surveyors and FDC staff. The review consisted of items selected from CMA audit tools and focused on the delivery of mental health services in the inpatient units (U, V, and T) and special housing dorms (O & P), with an emphasis on inpatient psychiatric medication practices and the administration of medication. There were a total of 67 items reviewed that were applicable to inpatient mental health services. Of these 67 items, 47 fell at or below 80% compliance, resulting in an overall non-compliance rate of 70%. For outpatient mental health services there were a total of 54 items reviewed. Of these 54 items, 29 fell at or below 80% compliance resulting in an overall non-compliance rate of 54% Below is a brief summary of each item with the corresponding percentage of records that were compliant. Only items that were at 80% compliance or below are included. Please note that while the total records reviewed is included for each area, each record reviewed was not necessarily applicable for all of the items. Psychiatric Medication Practices - Inpatient MH-1 5% Inmate received medication as prescribed MH-2 26% Psychiatric follow-ups conducted at appropriate intervals MH-3 33% Nurse met with inmate after 2 days of consecutive medication refusals MH-4 36% Physical exam completed within 3 working days of admission MH-5 40% Follow-up laboratory tests ordered and conducted MH-6 42% Physician’s note completed w/in 24 hours of admission to inpatient unit MH-7 50% Appropriate initial laboratory tests were ordered MH-8 50% Abnormal labs for psychotropic meds treated or referred appropriately MH-9 53% Appropriate informed consent signed for each psychotropic medication MH-10 56% ETO accompanied by a physician’s order specifying the medication as an ETO MH-11 56% Psychiatric evaluation completed in required timeframe MH-12 58% AIMS was administered within appropriate timeframes MH-13 61% Psychiatric follow-up notes were detailed and clinically appropriate MH-14 67% Refusal signed after 3 consecutive or 5 in a month medication refusals MH-15 72% Orders include the physician’s signature and are dated & timed MH-16 78% Med(s) ordered are appropriate for the symptoms and diagnosis MH-17 78% ETO rationale documented and it was clinically appropriate Total Records Reviewed: 19 Summary Comments: The review of these records confirmed grave concerns about the administration of medications in the inpatient units at Union CI. Out of 19 inpatient records reviewed, only 1 inmate received his medication as prescribed over the past 3-4 months. While there did appear Page 1 of 6 to be some recent improvement, a review of 50 current MARs for the first 9 days of November revealed that 54% of this sample did not receive medication as prescribed. The vast majority of the deficiencies were due to inmates not receiving one or more doses of medication, but there were a few instances where inmates received the wrong dose of medication. For example, in one case the physician’s order indicated that the inmate was prescribed 2 mg of Risperdal every evening. However, according to the October MAR the inmate was administered 2 mg of this medication twice a day. Compliance with required psychiatric follow-up visits was only at 26%. It was not unusual for inmates receiving Transitional Care to see a psychiatric provider every 2 months instead of the required monthly or biweekly visit. As reflected by the above percentages there were also significant compliance issues in the areas of laboratory tests, medication consents, and Emergency Treatment Orders (ETOs). Overall, in the area of Psychiatric Medication Practices only 3 of 20 items reviewed were above 80% compliance. Inpatient Mental Health Services MH-18 0% Vital signs taken daily for 5 days for all new admissions MH-19 0% Follow-up vital signs recorded within required timeframes MH-20 0% Weight recorded within required timeframes MH-21 5% Required nursing evaluations completed & documented MH-22 10% Required hours of planned structured therapeutic services provided & documented MH-23 14% Mental Health Professional notes were completed timely and clinically appropriate MH-24 24% Weekly group note was completed MH-25 30% Overall, treatment provided was appropriate MH-26 57% MDST met to review/document Behavioral Levels w/in required timeframes MH-27 64% Initial nursing assessment fully completed within 4 hours of admission MH-28 67% ISP was initiated and reviewed within the appropriate timeframe MH-29 71% Entries dated, timed, signed & stamped MH-30 75% Nursing provided explanation for admission and orientation to the unit w/in 4 hours MH-31 75% Vital signs were obtained within one hour of admission MH-32 75% For CM inmates the BRA was completed accurately and is signed by MDST MH-33 78% Discharge summary completed before CSU discharge Total Records Reviewed: 22 Summary Comments: These record reviews revealed additional serious deficiencies in inpatient nursing care, in addition to the medication administration issues described earlier. In all 22 records reviewed, weights and vital signs were not recorded per policy and in many instances the most recent graphic charts were from July or August. Additionally, there were no refusal forms found in the record to indicate that vitals were offered, but refused by the inmate. There were also many monthly TCU nursing evaluations missing, resulting in an overall compliance rate of 5%. In V dorm the most recent monthly nursing evaluations in the records were typically from July. Only 10% of the sample consistently received the required number of structured therapeutic services and overall these services primarily consisted of activity therapy and therapeutic community. There is Page 2 of 6 minimal individual and/or group counseling provided. For example, most records in U dorm reflected a total of 15 minutes of individual therapy and 30 minutes of group therapy per week. The provision of counseling services was even more limited in V dorm. Compliance with weekly group notes and case management notes was extremely poor and the most recent Mental Health Attendance Records found in the V dorm charts were typically from the week of September 21. Many of the progress notes in the TCU records, including the refusal notes, were “cookie-cutter” making it impossible to follow the course of treatment, including whether the inmate was making progress on the goals listed on his ISP. Progress notes in the CSU records were better, but did not always contain all of the required information. Additionally, many of the inpatient individualized services plans only listed the titles (e.g., mental health professional, psychiatrist), but did not specify the names of mental health providers. Outpatient Mental Health Services MH-34 0% 1 hour group or individual counseling offered per week and documented (CM only) MH-35 8% Inmate received medication as prescribed MH-36 15% ISP lists type and frequency of intervention, and staff responsible MH-37 20% The BRA was completed within required timeframes (CM inmates only) MH-38 29% Interventions and services described by ISP are documented MH-39 33% CM referral assessment completed w/in 5 days (CM inmates only) MH-40 44% Upon arrival current psychotropic meds continued until seen by psychiatry MH-41 46% Frequency of clinical contacts is sufficient and clinically appropriate MH-42 50% Counseling offered every 30 days for inmates with psychotic disorders MH-43 50% ISP is updated w/in 14 days of placement, and is current (CM only) MH-44 53% Appropriate informed consent signed for each psychotropic medication MH-45 58% Psychiatric follow-up conducted at appropriate intervals MH-46 63% After start of MH services, initial ISP completed within 30 days MH-47 64% Identified problems are on the problem list MH-48 67% Inmate seen by psychiatry prior to expiration of psychotropic meds MH-49 67% MSE completed, active MH problems assessed & ISP updated w/in 14 days of arrival MH-50 67% Nurse met with inmate after 2 days of consecutive medication refusals MH-51 69% ISP goals are time limited and written in objective measurable behavioral terms MH-52 71% The BRA is completed accurately and is signed by MDST members (CM only) MH-53 73% All entries were dated, timed, signed, and stamped MH-54 75% ISP signed by all MDST members and inmate or refusal is documented MH-55 78% Progress notes have sufficient detail to follow course of treatment Total Records Reviewed: 18 Summary Comments: The outpatient records reviewed consisted of Close Management or Death Row S-3 inmates. This review indicated that a total of 22 out of 36 items fell below 80% compliance. Similar to inpatient records, the review of outpatient MARs indicated that only 8% of the sample received their medication as prescribed over the past 3-4 months. Additionally, compliance with items pertinent to the Osterback case was poor. For example, in the applicable records reviewed Page 3 of 6 none contained documentation to confirm that 1 hour of counseling was consistently offered per week and only 20% of these records were compliant with the required timeframes for the completion of Behavioral Risk Assessments. Only 58% of the sample received psychiatric follow-up services in accordance with the timeframes specified in policy. Special Housing MH-56 27% Outpatient treatment is continued as indicated on the ISP MH-57 50% A Special Housing Health Appraisal was completed by nursing staff MH-58 50% Psychotropic medication continued while in special housing MH-59 62% Initial mental status exam was completed in the required timeframe & documented MH-60 64% Follow-up mental status exams are completed in the required timeframes MH-61 73% All entries were dated, timed, signed, and stamped MH-62 80% Mental status exams are sufficient to identify any possible adjustment problems Total Records Reviewed: 16 Summary Comments: This area consisted of a review of the delivery of mental health services in O and P dorms which revealed significant compliance issues as well. Only 1 out of the 8 items in Special Housing was above 80% compliance. Discharge Planning MH-63 25% Consent or refusal signed w/in 30 days after the initiation of aftercare Total Records Reviewed: 7 Summary Comments: Records reviewed for Aftercare Planning compliance revealed poor compliance with the documentation of signed consent or refusal. Inmate Requests MH-64 10% Interview or referral took place as responded to on inmate request Total Records Reviewed: 15 Summary Comments: A review of documentation in outpatient records revealed when an interview or referral was indicated in the response to the inmate request, in 9 out of 10 instances it did not occur as intended, raising significant concerns with access to care. SHOS MH-65 MH-66 MH-67 MH-68 40% 60% 67% 71% Observations recorded on checklist every 15 minutes Nurse evaluated inmate within 2 hours of admission Daily counseling by MH staff was conducted and documented Inpatient Mental Health Daily Nursing Evaluation completed each shift Page 4 of 6 MH-69 80% All entries were dated, timed, signed, and stamped Total Records Reviewed: 7 Summary Comments: The review of these records indicated less than 80% compliance in several areas of nursing services for inmates admitted to self harm observation status. In addition, daily counseling by mental health staff was not consistently conducted and documented. Psychiatric Restraints MH-70 0% Patient’s behavior observed every 15 minutes and documented on DC4-650A MH-71 0% Respiration & circulation checks completed and documented on DC4-650A MH-72 0% 4-point restraints: limbs exercised every 2 hours and documented on DC4-650A MH-73 0% Restraints removed after 30 minutes of calm behavior MH-74 50% Less restrictive means of behavioral control attempted and documented MH-75 50% Offered food, fluids and bedpan/urinal as required and documented on DC4-650A MH-76 50% Vital signs taken and recorded upon release from restraints Total Records Reviewed: 1 Summary Comments: This section of the audit was comprised of a single record, with 2 discrete events. This was the only applicable record documenting use of restraints at the time of the audit. The areas of significant non-compliance involved nursing staff documentation on DC4-650A of required monitoring during the restraint process, as well as a lack of documentation that less restrictive behavioral controls were attempted prior to the application of psychiatric restraints for 1 of the restraint episodes. Mental Health Systems Review and Inmate Interviews A review of staffing indicated 18 current nursing vacancies which included 12.6 LPNs, 4.6 RNs and the Director of Nursing position. It was reported that approximately 10 of the 18 vacancies are filled with agency nurses. A review of mental health logs found that both the Psychiatric Restraint Log and the Emergency Nursing Log had missing information. A total of ten inmates were interviewed (5 inpatient and 5 outpatient inmates). Overall, the information from the inmate interviews was consistent with the findings from the inpatient and outpatient record reviews. The primary complaint pertained to medication administration. Inmates reported they do not always receive their medication(s) and are informed by nursing staff that they ran out, the bottle is empty, etc. Inmates in V dorm reported that they are receiving little to no individual or group therapy. Overall, the inmates interviewed in V dorm reported more complaints about their mental health care than the inmates in U dorm. Page 5 of 6 In addition to medication complaints, inmates in O dorm reported some difficulties with access to inmate request forms and also indicated that when inmates declare mental health emergencies they are sometimes ignored by security staff. Two inmates independently described an incident where an inmate attempted to declare a mental health emergency, was reportedly ignored for several hours, and then attempted to hang himself. In an effort to verify these reports, the record of this inmate was reviewed and he had recently been placed on SHOS after a hanging attempt. A review of this inmate’s record revealed several concerning issues. He had recently been discharged from TCU level care to O dorm and per the MARs did not receive any of his medications the first 2 days following TCU discharge and did not receive one of his medications for 4 days. Additionally, there was no documentation that the decision to discharge this inmate was by the consensus of the MDST or that discharge was being contemplated. In fact, the inmate was seen in mid-September by a psychiatrist with a plan to see the inmate in 2 weeks due to medication changes, including a dosage increase of an anti-psychotic medication. There was no documentation in the record to indicate that after this appointment he saw a psychiatric provider or his case manager individually prior to his discharge at the end of October. At the time of this review he was on self-harm observation status (SHOS) and had been referred to the CSU. Overall Summary This review indicates serious and multiple deficiencies in the delivery of mental health care in both the inpatient and outpatient settings at Union Correctional Institution. The deficiencies in the administration of medication were particularly striking, as was the current nursing vacancy rate. The overall mental health care delivered in the inpatient units is inadequate, as evidenced by poor compliance with required psychiatric, psychological, and nursing services and sparse or missing documentation. The delivery and documentation of care in the Special Housing dorms was equally problematic with respect to the administration of medication and other requirements including those applicable to the Osterback case. Additionally, in many instances, inmates who submitted requests were not seen as intended, raising significant questions about access to care. In some cases it is possible that care was delivered, but was not documented, or the documents had not yet been filed. Nonetheless, this is unacceptable practice and certainly does not account for the majority of the findings in this report. Page 6 of 6