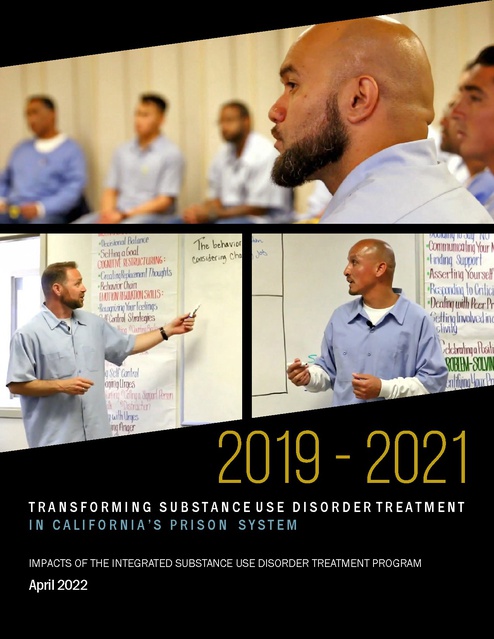
2019-2021 Impacts of the Integrated Substance Use of Disorder Treatment Program, April 2022
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
I
cmmN<i :
IT!nuJil~
hr d1nq ~~rt
Asedi11l} YourseW
~ u•lil~ \o (nli ,i
Deali1~ wi~ Peer Pr
,d Iir¥1 lnvolv~ inc
n
JXJl~ll5=
r!CY'linqc
m\rxf
1v1\9
'
.
2019 - 2021
TRANSFORMING SUBSTANCE USE DISORDER TREATMENT
IN CALIFORNIA’S PRISON SYSTEM
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM
April 2022
1
.
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
CALIFORNIA CORRECTIONAL
HEALTH CARE SERVICES
This report was prepared by: The California Department of Corrections and Rehabilitation &
California Correctional Health Care Services
The authors of this report used the most current data available; therefore, timeframes for
analyses may differ across measures.
2
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
TABLE OF CONTENTS
Executive Summary
••••••••••••••••••••••••••••
An Overdose Epidemic in California’s Prisons
• • • • • • • • • •
A New Approach for Substance Use Disorder Treatment
ISUDT Strategies and Services
6
• •
8
• • • • • • •• • • • • • •• ••
10
Significant Progress Implementing ISUDT
•••••••••
13
• • • • • • • • • • • • • • •
14
•••••• •••••• •••••• •••
19
•• • • • • ••••••• • • • • ••••••• • • • • ••••••
23
Impacts of the ISUDT Program to Date
Challenges and Opportunities
Conclusion
4
3
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
I
EXECUTIVE SUMMARY
I
The United States is facing a surge in overdose deaths that has reached crisis proportions. Nationally, overdose
deaths have more than tripled in just over a decade, from just over 21,000 in 2010 to more than 100,000 in
2021.1 The increase in overdose deaths, which spans age cohorts and racial groups, has been driven by a new
public health threat: synthetic opioids, primarily fentanyl. Impacts are exponentially worse in jails and prisons,
where overdose death rates among incarcerated individuals grew by 600% from 2001 to 2018.2 Amidst the
COVID-19 pandemic, overdose deaths have continued to increase across the nation – but not among residents
of the California Department of Corrections and Rehabilitation (CDCR) and California Correctional Health Care
Services (CCHCS).
In large part, this is because California’s taxpayers made an unprecedented investment to expand evidencebased substance use disorder (SUD) treatment within CDCR and CCHCS under the Integrated Substance
Use Disorder Treatment (ISUDT) Program. The ISUDT Program provides timely and effective treatment and
transition to the community for incarcerated individuals with SUDs, with the goals of saving lives, reducing
avoidable health complications and costs, improving public safety and promoting healthier communities.
In January 2020, the ISUDT Program was implemented, and includes five core program elements: 1) SUD
Screening and Assessment, 2) Medication Assisted Treatment (MAT), 3) Cognitive Behavioral Interventions
(CBI), 4) Supportive Housing; and 5) Enhanced Pre-Release Planning and Transition Services aimed at
strengthening care coordination upon release.
The goals CDCR and CCHCS are seeking to achieve through the implementation of the ISUDT Program are
supported by research that shows upfront investment in SUD treatment is effective and cost-beneficial.
According to the National Institute on Drug Abuse (NIDA), every dollar invested in SUD treatment yields a
return on investment (ROI) of between $4 and $7 in criminal justice costs, and when accounting for avoided
health care costs, SUD treatment can yield on ROI of 12 to 1.3 The preliminary findings presented in this
report indicate that the investment in the ISUDT Program has already begun to pay off through lives saved and
reductions in avoidable health complications.
This report is intended to provide an overview of the ISUDT Program, document the status of implementation,
and present preliminary findings on program impacts and its potential to improve a range of outcomes,
including morbidity and mortality. In addition, this report describes the challenges and future direction
necessary to fully realize the positive potential of the ISUDT Program.
Just three months after implementation of the ISUDT Program, the COVID-19 pandemic first reached
California’s prison system. CDCR and CCHCS directed departmental resources to a system-wide emergency
public health response to protect the residents and staff living and working in California’s prisons. Despite
modifications to virtually every aspect of departmental operations, including limitations on programming and
contractor access to prisons to prevent the spread of COVID-19, CDCR and CCHCS continued its commitment to
1
Ahmad, F. B., Rossen, L. M., & Sutton, P. (2022, January 12). NVSS Vital Statistics Rapid Release Provisional Drug Overdose Death Counts. (L. M. Rossen, A. Lipphardt,
F. B. Ahmad, J. M. Keralis, Y. Chong, Editors, & National Center for Health Statistics) Retrieved January 24, 2022, from National Center for Health Statistics: https://
www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm
2
Carson, E. A. (2021). Mortality in State and Federal Prisons, 2001-2018 - Statistical Tables. Office of Justice Program, Bureau of Justice Statistics. Washington, D.C.:
U.S. Department of Justice. Retrieved from https://bjs.ojp.gov/content/pub/pdf/msfp0118st.pdf
4
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
the ISUDT Program, becoming operational at all 34 prisons.
In accordance with infection control guidelines, CDCR and CCHCS adapted in-person CBI to packet-based
programming to enable participants to continue CBI participation in a self-paced, independent format with
weekly check-ins with an Alcohol and Other Drug (AOD) counselor in locations where in-person programming
was not feasible or safe due to the pandemic. With the introduction of the COVID-19 vaccine, and easing of
some COVID-19 restrictions in 2021, the Department restored in-person CBI. Through in-person and packet
programming, CDCR and CCHCS provided CBI to more than 14,200 residents statewide. After extensive
work to develop new coordination processes and communication mechanisms with county probation
offices and community health care partners, the pre-release teams connected more than 2,200 people with
community SUD treatment and related support services prior to their release from CDCR. The Supportive
Housing component of ISUDT, which was envisioned as separate housing for those involved in ISUDT, has
been significantly impacted by COVID-19 due to isolation and quarantine requirements. The Department is
currently examining several options for Supportive Housing with discussions focused on rehabilitation and
recovery housing for ISUDT participants plus those involved in other rehabilitative programs and services.
The Department is aiming to initiate Supportive Housing in the summer of 2022, contingent upon COVID-19
restrictions.
During the implementation of ISUDT, the Department made many large-scale operational changes in response
to the COVID-19 pandemic. However, detailed analysis indicates ISUDT services were the major driver of a
change in SUD-related health outcomes. A study of CDCR overdose patterns indicates that overdoses began to
decline before the pandemic and continued to decline even as the Department vaccinated most of its resident
population, COVID-19 restrictions eased, programming resumed at near-normal levels in many institutions, and
once again in-person visitation was allowed. Other state prison systems that implemented the same restrictive
policies as CDCR during the pandemic, did not see the same decline in overdose deaths and hospitalizations
as observed among CDCR’s population. A comparison of CDCR residents who received MAT versus those
who were on the MAT evaluation waitlist between January 2020 and March 2021, showed that the overdose
hospitalization rate related to opiates was 48% lower for those prescribed MAT compared to those who
were on the MAT evaluation waitlist. While the results are trending in a positive direction, the Department
recognizes the unprecedented circumstances in our prisons and communities during the time these analyses
were conducted and the potential impacts those circumstances may have on the data; however, we remain
cautiously optimistic and ever vigilant.
The initial results of the ISUDT Program have surpassed expectations, with great progress made
towards screening and assessing residents with SUD:
• As of January 2022, the Department has screened more than 64,690 people for SUD, assessed
an additional 38,638, and prescribed MAT to treat nearly 22,558 individuals. In terms of service
volume, California’s prison system has become the largest MAT provider among jails and prisons in
the country. Additionally, among non-correctional health care systems, the Department ramped-up
at a rate that exceeds rapidly expanding community programs, with 140 people per 1,000 receiving
MAT services under ISUDT.
• It was originally estimated that about half of all residents offered MAT would actually accept
that component of the ISUDT Program; to date, nearly nine out of ten patients offered MAT have
accepted treatment.
5
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
• Among California’s prison population, the rate of overdose deaths declined 58% from 2019 to
2020 and according to the preliminary 2021 mortality data is on track to remain low even as the
Department returned to near-normal operations in 2021.
• Hospitalization rates for overdoses and skin/soft tissue infections have declined after ISUDT
implementation, by 18% and 21%, respectively.
• Among those treated for hepatitis C virus (HCV), the reinfection rate for those prescribed MAT was
29% lower than for those with an opioid use disorder (OUD) who were not prescribed MAT. Since
implementation of ISUDT, CDCR and CCHCS are also seeing improvements in other health outcomes
closely linked to SUD. For example, an underlying risk factor for most HCV infections is SUD. Even
after HCV treatment, individuals with SUD may become re-infected if the SUD is not addressed.
• Over the past two years, CDCR and CCHCS have received numerous testimonials from residents
and staff about the remarkable ways in which the ISUDT Program is changing lives.
Despite the pandemic, CDCR and CCHCS staff have made substantial progress toward fully realizing the vision
of the ISUDT Program, and promoting a better way of life for incarcerated individuals with SUDs. In the
coming year, ISUDT leaders will navigate challenges, such as continued COVID-19 related infection prevention
strategies, as the CDCR and CCHCS will work to expand ISUDT to all residents with SUDs. The CDCR and CCHCS
will seek to leverage opportunities to improve health outcomes for residents in prison and upon release to
the community, including two major Medi-Cal expansion programs, and the Governor’s initiatives to end
homelessness. The CDCR and CCHCS will also collaborate with academic partners and state agencies to
evaluate and report program outcomes within the CDCR and communities post-release, with special emphasis
on continuity of care, sustained recovery, recidivism, and the individual’s post-release ability to maintain stable
housing, employment, and treatment.
I
AN OVERDOSE EPIDEMIC IN CALIFORNIA’S PRISONS
I
In 2019, 50,000 people in the United States died from opioid-involved overdoses, a surge in mortality linked
to the emergence of synthetic opioids. The NIDA labeled the problem an opioid overdose crisis, declaring,
“The misuse of opioids – including prescription pain relievers, heroin, and synthetic opioids such as fentanyl –
is a serious national health crisis that effects public health as well as social and economic welfare.” 4 California
saw its own increase in overdose deaths in 2019, with the statewide rate per 100,000 increasing by 16% over
the prior year.5 Please see Figure 1.
3
NIDA. https://nida.nih.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/frequently-asked-questions/drug-addictiontreatment-worth-its-cost
4
NIDA. (2021, March 11). Opioid Overdose Crisis. Retrieved January 24, 2022, from National Institute on Drug Abuse Advancing Addiction Science: Opioid Overdose
Crisis | National Institute on Drug Abuse (NIDA)
5
California Department of Public Health. (2022, January 19). California Overdose Surveillance Dashboard. Retrieved from https://skylab.cdph.ca.gov/ODdash/
6
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
Nationally, the overdose mortality rate in state prison systems increased 623% from 2001 to 2019.6 In 2019,
overdoses deaths within California’s prison system, most of them related to opioid use, reached a record high
of 51 overdose deaths per 100,000 residents, which was the highest overdose mortality rate for a state prison
system in the United States. Please see Figure 1. This was a culmination of a steep climb in overdose deaths
that began in 2012.7
FIGURE 1. OVERDOSE DEATHS PER 100,000 INCARCERATED INDIVIDUALS:
THE CDCR VS. OTHER STATE PRISON SYSTEMS
CDCR: 363% increase
2012-2019
60
51
48
50
40
30
22
18
20
15
14
10
3
4
2012
2013
0
7
4
CDCR
2014
Other State Prison Systems
2015
2016
2017
2018
2019
The Department saw an increase of 95% in Emergency Department visits and hospitalizations due to overdose
between 2016 and 2019. Please see Figure 2.
FIGURE 2. EMERGENCY DEPARTMENT VISITS AND HOSPITAL ADMISSIONS
FOR DRUG OVERDOSE AMONG CALIFORNIA PRISON RESIDENTS
2016 - 2019
95% Increase
1400
1248
Ill
a: 1200
LU
z~
::,
0
1082
1000
u
zLU
800
LI.
0
a:
LU
m
~
::,
z
639
600
400
200
0
2016
2017
-
2018
2019
Total Hospitalizations
6
Carson, E. A. (2021). Mortality in State and Federal Prisons, 2001-2019 - Statistical Tables. Office of Justice Program, Bureau of Justice Statistics. Washington, D.C.:
U.S. Department of Justice. Retrieved from https://bjs.ojp.gov/content/pub/pdf/msfp0119st.pdf
7
Imai, K. (2021). Analysis of 2020 California Correctional Health Care Services Inmate Mortality Reviews. Consultant to the California Prison Receivership. California
Correctional Health Care Services. Retrieved from https://cchcs.ca.gov/wp-content/uploads/sites/60/MS/2020-CCHCS-Mortality-Review.pdf
7
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
Long-term substance use contributes to a number of acute and chronic health complications including heart
and lung disease, stroke, cancer, and mental health conditions,8 which can be challenging to treat and often
result in hospitalizations. Injection drug use is associated with many serious health conditions including
Hepatitis B and C viruses, which can lead to liver failure, Human Immunodeficiency Virus (HIV),9 and bacterial
infections of the heart, bones, muscles, and skin. Alcohol Use Disorder (AUD) is linked to high blood pressure,
heart disease, liver disease, stroke, at least eight different cancers, weakening of the immune system,
depression, anxiety, and learning and memory problems.10 Prolonged methamphetamine use can cause
permanent damage to the heart and brain; high blood pressure leading to heart attacks and strokes; liver,
kidney, and lung damage; paranoia, hallucinations, and mood disturbances; intense itching and associated skin
sores; premature osteoporosis; and severe dental problems.11 The medical complications of SUDs not only
significantly increase health care costs in the prison system, but also in the community at large.
The riskiest time for California’s incarcerated population with SUD, which is estimated to be near 70% of
the population, occurs upon release to the community. Newly-released individuals who are struggling with
converging transition-related stressors such as obtaining immediate survival needs and finding stable housing
and employment are susceptible to using substances as a coping mechanism. With easy access to drugs
and a reduced physical tolerance for drug effects after years in prison, one study found that newly-released
individuals with SUD are 40 times more likely to die of a drug overdose within two weeks of leaving prison
than their age-matched counterparts in the community.12
Within the prison population, drug trafficking contributes to a violent and dangerous atmosphere,
undermining efforts to give residents a safe and stable environment to obtain treatment, learn a trade, or
advance their education. Individuals with untreated SUD are often not successful upon community reentry
and are more likely to re-offend.
A NEW APPROACH
FOR SUBSTANCE USE DISORDER TREATMENT:
STATUS OF PROGRAM IMPLEMENTATION
Substance use-driven factors impacting the quality of resident life and the safety of prisons has elevated SUD
treatment to the highest priority level for California’s prison administrators.
8
NIDA. (2020, July). What are the health consequences of drug addiction? Retrieved from National Institute on Drug Abuse Advancing Addiction Science: https://nida.
nih.gov/publications/drugs-brains-behavior-science-addiction/addiction-health
9
CDC. (2021, August 31). Persons Who Inject Drugs (PWID)s Infectious Diseases, Opioids and Injection Drug Use. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/pwid/opioid-use.html
10
CDC. (2021, December 29). Alcohol and Public Health Alcohol Use and Your Health. Retrieved from Centers for Disease Control and Prevention: https://www.
cdc.gov/alcohol/fact-sheets/alcohol-use.htm#:~:text=Over%20time%2C%20excessive%20alcohol%20use%20can%20lead%20to,and%20poor%20school%20performance.%20...%20More%20items...%20
11
Substance Abuse and Mental Health Services Administration (SAMHSA). (2021, November 11). Know the Risks of Meth Learn about Methamphetamine. Retrieved
from SAMHSA.gov: https://www.samhsa.gov/meth
12
Ranapurwala, S. I., Shanahan, M. E., Alexandridis, A. A., Proescholdbell, S. K., Naumann, R. B., Edwards Jr, D., & Marshall, S. W. (2018, September). Opioid Overdose Mortality Among Former North Carolina Inmates: 2000–2015. American Journal of Public Health, 108, 1207-1213. doi:10.2105/AJPH.2018.304514. Accessed at
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6085027/
8
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
In 2019, then-Secretary of the CDCR, Ralph Diaz, and the Federal Court Receiver assigned to oversee the prison
medical system, J. Clark Kelso, jointly requested the support of the Governor’s Office, the Legislature, and
the presiding judge in Plata vs. Newsom, the Honorable Jon S. Tigar, to address the SUD crisis in California’s
prisons. As current Secretary of the CDCR, Kathleen Allison has renewed the Department’s commitment to
maintaining a quality ISUDT Program as a top departmental priority.
In Fiscal Year 2019-20, the California Legislature approved the Department’s request for ongoing funding of
more than $160 million per year to implement the first phase of the new SUD treatment approach under
the ISUDT Program. In July 2019, upon receiving support from the Legislature, CDCR and CCHCS leaders
established an implementation plan that would make the five service areas described in this section fully
operational by the end of June 2021.
The CDCR/CCHCS consulted with substance use specialists and national addiction medicine experts, and
reviewed medical evidence to update and redesign a SUD treatment system that would effectively address
the challenges posed by fentanyl and other synthetic opioids. The Department convened advocates for the
incarcerated, representatives from state and county SUD treatment systems, court experts in medical, mental
health, and disability issues, and academic partners to inform program development.
The ISUDT Program incorporates the most current best practices in addiction science and manages SUD
as a chronic illness. The ISUDT Program is grounded in the principal that SUD results from a combination
of biological, genetic, and environmental factors, similar to other chronic diseases, such as diabetes, and
all of those factors must be considered in the development of effective treatment strategies. Consistent
with current addiction medicine practices, the ISUDT Program combines pharmaceutical interventions with
behavior interventions, lifestyle adaptations, and peer and self-help support strategies. Similar to the way a
primary care team may prescribe diabetic patients insulin but would also educate patients in making changes
to diet and exercise, and how to monitor their own blood sugar levels. The design of the ISUDT Program
utilizes the Whole Person Care approach and considers the impacts of adverse childhood experiences such as
abuse, neglect, and toxic trauma, as well as co-existing health conditions, such as mental illness and chronic
infections like HCV.
The new model requires multi-disciplinary coordination, drawing participation from all program areas within
the Department.13 In addition, the model includes collaboration with other state agencies such as the California
Department of Health Care Services (DHCS), which manages the state’s Medi-Cal Program; and coordination
with jails; probation, social service, and health departments within California’s 58 counties; non-profit,
government and university public health and SUD treatment experts; and critical stakeholders, including the
families and friends of incarcerated people, and court experts and plaintiffs’ attorneys in three class action
lawsuits; among others.
Three months into ISUDT implementation efforts, the COVID-19 pandemic reached California, sending the
Department into an emergency response mode that continues to date and which has modified virtually every
aspect of operations for the CDCR and CCHCS. Residents of correctional facilities, like residents of college
dormitories, military barracks, and nursing homes, are among the highest risk populations for contracting
COVID-19 infections.
13
CDCR program involvement includes, but is not limited to, the Division of Rehabilitative Programs, Division of Adult Institutions, Division of Adult Parole, Board
of Parole Hearings, Prison Industry Authority, all clinical disciplines within Health Care Services and the Quality Management/Patient Safety Programs, Division of
Administrative Services, Office of Public and External Communications, Office of Legal Affairs and Office of Legislative Affairs.
9
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
At its peak in December 2020, the COVID-19 infection rate was six times higher for prison residents than the
non-incarcerated population in California. At that time, the CDCR and CCHCS were managing 10,000 cases in
facilities across the state, representing roughly 1 in 10 residents.14
Like other health care organizations, the CDCR and CCHCS limited operations to only essential health care
services. Early in the pandemic, Department leaders recognized SUD treatment as an essential health care
service, because the need for SUD treatment was more crucial than ever. Public health experts across the
country, including California, identified a surge of overdose deaths, as sudden changes in daily routines,
isolation, fear of disease, deaths of loved ones, financial struggles, and other stressors that resulted from
the pandemic caused people with SUD to need substances more than ever to cope. The Centers for Disease
Control and Prevention (CDC) announced the highest-ever recorded number of overdose deaths in the United
States for the one-year period ending May 2020, including an increase in synthetic opioid-involved deaths of
more than 98% for the 10 western states.15
The ISUDT Program offers five major treatment strategies to support recovery, address SUD for incarcerated
individuals, and to ensure continuity of care as they transition to the community upon release. The following
section describes each ISUDT Program component and provides an update on the status of implementation.
THROUGH THESE STRATEGIES AND SERVICES,
THE ISUDT PROGRAM STRIVES TO:
• Reduce SUD-related mortality and morbidity, and
associated health care costs.
• Create a rehabilitative environment in state prisons,
improving safety for residents and staff.
• Successfully reintegrate individuals into their
community at time of release.
• Improve public safety and promote healthy
families and communities.
• Reduce recidivism and associated criminal justice
costs.
1. SCREENING & ASSESSMENT
To determine eligibility for ISUDT services, departmental health care staff screen patients for SUD and assess
them using standardized tools from the NIDA and the American Society for Addiction Medicine (ASAM). Based
on assessment results, clinicians identify the severity of the individual’s SUD and determine a level of care
and appropriate intensity of services for their particular needs. The first group prioritized for treatment were
individuals scheduled for release within 15-24 months and persons at highest risk for overdose or those who
had arrived to the CDCR already on MAT.
2. MEDICATION ASSISTED TREATMENT
MAT is the use of medications, in combination with counseling and behavioral therapies, to provide a “Whole
14
Population COVID-19 Tracking. (2022, January 27). Retrieved from California Department of Corrections and Rehabilitation: https://www.cdcr.ca.gov/covid19/
population-status-tracking/
15
CDC. (2020, December 18). Overdose Death Accelerating During COVID-19 Expanded Prevention Efforts Needed. Retrieved from Centers for Disease Control and
Prevention: https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
16
SAMHSA. (2021, November 4). MAT Medications, Counseling, and Related Conditions. Retrieved from SAMHSA.gov: https://www.samhsa.gov/medication-assistedtreatment/medications-counseling-related-conditions
10
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
Person” approach to the treatment of SUDs.16
In the past decade, advances in genetics, molecular biology, behavioral neuro-pharmacology, and brain
imaging have allowed addiction specialists to map the neurological damage caused by substance use and
develop pharmaceutical interventions to treat it. Prolonged SUD dysregulates dopamine levels in the brain. To
the extent that people with SUD require increasing amounts of dopamine to achieve base levels of function,
MAT is now available.
The federal Food and Drug Administration has approved several different medications to treat alcohol and
OUD. MAT medications relieve withdrawal symptoms and psychological cravings. Medications used for MAT
are evidence-based treatment options and do not substitute one drug for another.17 Under the ISUDT Program,
physicians and advanced practice providers prescribe federal Food and Drug Administration-approved
medications to improve neuro-behavioral function for patients who meet specific clinical criteria.
CCHCS physicians prescribe medication to eligible patients who have been diagnosed with alcohol use disorder
and/or OUD to repair neurological damage caused by prolonged SUD, prevent debilitating symptoms of
withdrawal, and enable individuals to effectively participate in rehabilitative programs. To meet the needs of
the large number of CDCR patients who would benefit from the MAT component of the ISUDT Program, CDCR
and CCHCS have created one of the largest primary care provider (PCP) workforces in the country who are
prepared to deliver MAT services.
PCPs prescribe medications for the patients
on their panel, spreading the workload of
MEDICATIONS USED TO TREAT SUD IN CDCR:
managing the many patients with SUD over
hundreds of trained PCPs rather than a small
ALCOHOL USE DISORDER
and centralized group of addiction medicine
Acamprosate
specialists. Over the last two years, all of the
Naltrexone
Department’s 500 PCPs and physician leaders
OPIOID USE DISORDER
received additional training to manage SUD
Naltrexone
patients and obtained Drug Enforcement
Buprenorphine
Agency X-waivers permitting them to prescribe
Methadone
buprenorphine, the medication most often
Naloxone (overdose reversal)
used to treat OUD. The effort to prepare PCPs
to manage their own patients represents one of
the largest endeavors in the country to engage a PCP workforce in the treatment of SUD.
3. COGNITIVE BEHAVIORAL INTERVENTIONS
Rooted in cognitive behavioral therapy, CBI is based upon the premise that how people think impacts
emotional responses and resulting behavior. CBI focuses on recognizing and addressing self-destructive
thoughts, beliefs, and attitudes (cognitive distortions), changing behaviors, and skills to improve emotional
regulation and cope with stressful or adverse circumstances in a healthy way. Based on individual screening
and assessment results, program participants are eligible for one of three different CBI pathways, which vary
in curriculum content and intensity of service. The pathways include Life Skills, Outpatient Treatment, and
Intensive Outpatient Treatment, facilitated by AOD counselors.
17
SAMHSA. (2021, November 4). MAT Medications, Counseling, and Related Conditions. Retrieved from SAMHSA.gov: https://www.samhsa.gov/medication-assistedtreatment/medications-counseling-related-conditions
11
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
4. SUPPORTIVE HOUSING
Supportive Housing was envisioned as housing units separate from other incarcerated populations to promote
a rehabilitative environment for those engaging in ISUDT programming. Although space for Supportive
Housing was identified at each institution, the implementation of Supportive Housing was impacted by
COVID-19. Research indicates that individuals with SUD who participate in Supportive Housing have lower
rates of both relapse and recidivism than people who do not participate in supportive group environments.18
The Department is currently exploring options for rehabilitation and recovery focused housing for ISUDT
Program participants and others involved in rehabilitative programming, and are aiming to initiate Supportive
Housing in the summer of 2022, contingent upon COVID-19 restrictions.
5. ENHANCED PRE-RELEASE PLANNING & TRANSITION SERVICES
Under the final major component of ISUDT Program, Enhanced Pre-Release Planning and Transition Services,
staff with different roles work to prepare individuals for their transition to the community including assessing
the participant’s current needs, collaborating to develop a comprehensive pre-release plan, and facilitating
connections with the community in accordance with that plan. Since January 2020, the ISUDT Program has
connected 2,211 participants with community SUD providers upon their release.
Enhanced pre-release planning is not only intended to ensure that participants receive continuity of SUD
treatment upon release and mitigate the immediate and exponentially high risk of overdose after leaving
prison, but also to ensure that participants receive the support necessary to successfully integrate into the
community. Individuals who are released from prison without stable housing or a source of income are
vulnerable to homelessness, relapse of substance use and recidivism.
In the latter part of 2020 and early 2021, ISUDT leaders established weekly multi-disciplinary team meetings
and new automated population management tools to facilitate continuity of SUD services with community
providers. For each participant, the needs assessment and enhanced pre-release plan dictates a series of tasks
that must be performed by multi-disciplinary pre-release teams. Team huddles are utilized to review the status
of these tasks for soon-to-be-released participants and address any barriers in linking participants to what they
need before they are released. Through the enhanced pre-release process, the Department offers Naloxone to
each participant, a life-saving medication that can be administered when a person overdoses on opioids.
To coordinate care, institution and community health care providers need access to critical clinical data. The
ISUDT Program has established a series of near real-time, automated tools to support enhanced pre-release
planning that are available to county probation and public health departments through a new communication
portal. The portal offers a means of sharing information and a common reference point for program partners,
which is critical to navigating 58 different county-level SUD systems. During the pandemic, this portal served
an unexpected function when CDCR was able to use it to provide public health departments with the COVID-19
status of every CDCR resident soon-to-be-released to California counties, supporting county public health
efforts to set up quarantine and isolation services as necessary.
18
Inciardi, J. A. (1996, June). A Corrections-Based Continuum of Effective Drug Abuse Treatment. National Institute of Justice, Office of Justice Programs. U.S.
Department of Justice. Retrieved from https://nij.ojp.gov/library/publications/corrections-based-continuum-effective-drug-abuse-treatment
12
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
SIGNIFICANT
PROGRESS
IMPLEMENTING THE
ISUDT PROGRAM
In 2020 and 2021, CDCR and CCHCS balanced the immediate need to offer SUD treatment with the urgent
need for infection control by modifying aspects of the ISUDT Program that would have conflicted with the
COVID-19 response, including Supportive Housing. With this approach, CDCR and CCHCS were able to become
fully operational with MAT and CBI at all 34 institutions while deploying a rapidly-evolving statewide response
to the public health emergency. From the time the Department applied its most restrictive emergency
public health measures in March 2020 to the reopening of CDCR institutions and resumption of near-normal
programming in April 2021, health care staff continued to screen, assess, and evaluate residents for SUD
and refer residents to appropriate MAT and CBI treatment. From March 2020 to April 2021, the number of
participants receiving MAT within CDCR increased 780%. Please see Figure 3.
Figura 3. califomia Prison Residents Taking Medication Assisted
Treatment Statewide, January 2019 - January 2022
64,690
Residents screened for SUD
16000
14000
38,638
Residents assessed for specific
treatment needs
Statewide shift to
emergency operations
due to COVID-19
12000
10000
Statewide shift_ to
emergency o rations
due to COVID-19
8000
6000
22,658
Residents received Medication
Assisted Treatment to treat SUD
Data as of January 19, 2022
4000
2000
0
°'...r:!: °''Z
!!.I
:E
:E
~
. .
>,
1°'
~
°'~ °'
.,,e-
iz
C
N
r:!:
~
. ~.
C
~
:E
:E
C
C
~
.,,e-
~
~
C
... ... ... ... ... ...
.. 1.
~
N
~
z
~
:E
~
r:!:
:E
~
~
~
.,,e-
~
~
z
N
N
r:!:
~
It was originally estimated that about half of all CDCR residents offered MAT would actually accept that
component of the ISUDT Program; to date, nearly nine out of ten patients offered MAT have accepted
treatment. The ISUDT Program now provides MAT services to more patients each year than any other prison
or jail system in the United States. For comparison purposes, the Federal Bureau of Prisons (FBOP) and the
Cook County Jail in Chicago (the largest single-site jail in the United States), have annual populations of about
100,000 (comparable to CDCR). The FBOP offers SUD treatment through various behavioral interventions
to over 25,000 individuals each year, but by the end of 2019, only provided MAT to 116 people (the most
13
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
recent data available) - although they have plans for MAT expansion.19 The Cook County Jail treats about 6,000
individuals each year with MAT (roughly 500 per month).20 The rate of CDCR residents on MAT also exceed
community comparison groups.21
The ISUDT Program pairs MAT with CBI, to recognize the self-destructive thoughts, beliefs, and attitudes
(cognitive distortions) behind SUD compulsions, which often stem from prior childhood and ongoing
psychosocial trauma. Early in the pandemic, delivery of CBI services was interrupted when the Department
attempted to decrease the risk of COVID-19 entering the prisons by limiting access to visitors and certain
contractors, including AOD counselors. In response, ISUDT leaders established a self-guided, packet version
of the CBI curriculum and one-on-one encounters with an AOD counselor to continue services until regular
programming could resume. After the Department once again allowed access to prisons, ISUDT leaders
initiated group sessions, employing COVID-19 precautions such as physical distancing, personal protective
equipment, and air purifiers placed within treatment rooms. Consistent with other rehabilitative programs,
eligible ISUDT participants are awarded milestone completion credits for successful completion of CBI.
Over the past two years, ISUDT leaders have created a local infrastructure to manage the ISUDT Program.
Specifically, CDCR and CCHCS issued quarterly goals to guide institutions through the phased program
implementation and established an automated ISUDT Dashboard, which is updated daily and posted to the
Department’s intranet. The ISUDT Dashboard offers dual functionality providing performance data to help
institutions assess their progress toward program goals and operational tools with record-level data and colorcoded alerts to give institution staff the detailed information necessary to improve performance. A public
version of the Dashboard can be accessed here: https://cchcs.ca.gov/isudt/dashboard/
Each institution implemented a multi-disciplinary ISUDT Steering Committee to convene leaders ISUDT INSIDERisudt
INSIDER
monthly, assess progress to date, and troubleshoot program barriers. ISUDT leaders also
organized a network of change ambassadors to facilitate the cultural shift required to support
ISUDT operations, and a robust communications strategy, including, but not limited to; an ISUDT
web site; coordination of large conferences to gather input from program stakeholders to inform
program planning and implementation; distribution of the “ISUDT Leader,” a quarterly electronic magazine
for staff that includes program information and updates; and the “ISUDT Insider,” a monthly newsletter-style
publication for program participants that includes brain-teasing activities, inspiring patient feedback, notes of
encouragement from providers, and fillable journal entries, with approximately 215,000 copies distributed.
THE
- pg 2
Crossword
- pg 3
Word Search
- pg 3
Dr.’s Note
4-5
tips - pgs
Happiness
5
Sudoku - pg
t - pg 6
Patient insigh
- pg 7
Yoga lesson
pgs 8-15
Journals - pg 17
Feedback form
I
IMPACTS OF THE ISUDT PROGRAM TO DATE
THE
ER 11
NumB
ISSUE g good”
“ FeelinY 2021
MA
“I really mean when I say my biggest
fear in early recovery was that I would
never have fun again. The beautiful
truth is that recovery has given me
freedom and the confidence to go out
in the world and leave my own mark.”
~Tom Stoddart
8
mBER ”
E Nu
ISSU at last
“ freeuary 2021
Febr
- pgs 6-7
SMART Goals
pgs 8-15
Journals - pg 2
- pg 16
Crossword
- pg 3
Patient Art
h, Dr.’s Note
4-5
- pg 17
Word Searc
Making - pg
/Feedback
story, Motto
Journal Share
Free At Last
5
Sudoku - pg
I
Two years into the ISUDT Program, overdose deaths among CDCR residents have sharply declined at a time
when they are increasing in other state prison systems, California communities, and the country at large.
During the pandemic, the CDC reported that the United States had experienced back-to-back years of recordbreaking overdose deaths. The country reached 100,306 deaths in the 12-month period ending April 2021,
a 28% increase over the previous all-time high noted for the prior 12-month period.22 During this same
timeframe, the mortality rate among CDCR residents decreased from a high of 52 overdose deaths per 100,000
residents in 2019, the year the ISUDT Program began, to a preliminary estimate of 20 deaths per 100,000
residents in 2021.
14
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
Prior to ISUDT Program implementation, drug overdose was the third leading cause of death for CDCR’s
residents; however, by the end of 2020, it had fallen to the eighth leading cause of death, its lowest ranking in
nine years.23
The decrease in mortality due to overdose corresponded with the increase in MAT participation, which began
prior to the start of the pandemic. As enrollment in the MAT component of ISUDT grew, overdose deaths and
hospitalizations decreased. Participation in MAT gradually increased from just over 200 participants in early
2020 to nearly 14,000 by the end of 2021. In the first year of the program, the overdose death rate dropped
by 58%. Preliminary data shows the overdose mortality rate is on track to remain at this lower level for 2021.
Please see Figure 4.
FIGURE 4. OVERDOSE DEATHS & PATIENTS ON MAT BY YEAR (PER 100K)
~
0
0
.......
60
16,000
so
14,000
0
12,000 ~
...
40
10,000 X,
30
8,000
ti
Q.
..
"'
.c
Ill
ti
0
0
0
~
6,000
20
4,000
10
2,000
0
.."'
C
ti
;
Ill
a.
~
:E
0
2016
2017
2018
-
OD Deaths per 100k
2019
2020
On MAT per 100k
2021*
*Preliminary data
During the COVID-19 pandemic, a series of infection prevention measures were implemented to protect the
residents and staff of CDCR. Nearly every aspect of day-to-day operations were modified, from visiting hours
and resident movement to the way a wide variety of rehabilitative programs were delivered. In particular, the
Department frequently limited contact between residents and other people, be that other residents, staff,
or visitors. Leaders suspected the reduction in contact had cut off avenues for illicit substances; however,
detailed analysis points to ISUDT services as the most significant driver in the decline in overdose deaths and
hospitalizations for four reasons.
1. The sharp drop in overdose deaths began prior to the pandemic. A study of overdose deaths indicates
that mortality rates began to decline around September 2019, six months before the Department initiated
the COVID-19 response. Please see Figure 5.
19
Carson, E. (2021). Federal Prisoner Statistics Collected under the First Step Act, 2020. Office of Justice Programs, Bureau of Justice Statistics. Washington, D.C.: U.S.
Department of Justice. Retrieved January 21, 2022, from https://www.bjs.gov/content/pub/pdf/fpscfsa20.pdf
Expert interview with Chief of Operations, Cook County Jail
21
SAMHSA. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS
Publication No. PEP21-07-01-003, NSDUH Series H-56). Center for Behavioral Health Statistics and Quality. Rockville, MD: Substance Abuse and Mental Health Services
Administration. Retrieved from https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.
pdf
22 CDC. (2021). https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm
23 Imai, K. (2021). Analysis of 2020 California Correctional Health Care Services Inmate Mortality Reviews. Consultant to the California Prison Receivership. California
Correctional Health Care Services. Retrieved from https://cchcs.ca.gov/wp-content/uploads/sites/60/MS/2020-CCHCS-Mortality-Review.pdf
20
15
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
FIGURE 5. DRUG OVERDOSE MORTALITY WITHIN CDCR BY MONTH
2016 - 2020 (N=206)
...
t/1
95% Cl : Feb-19 - Mar-20
120
ta
GI
Pre-COVID
COVID Response
95% Cl: Feb-19 - M ar-20
:rC
100
E!
80
8
0
60
....0...
GI
40
0
GI
Q.
0
.
Q.
GI
ta
a:
20
•• •
•
•
•
• • ••
••
0
•
Observed Crude Rate
•
Modeled Crude Rate
Analysis Provided by Justine Hutchinson , PhD, Research Specialist IV ISUDT Program & Public Health
2. Other state prison systems implementing the same types of COVID-19 restrictions as CDCR and CCHCS did
not see a similar decline in overdose rates. For example, North Carolina has reported a 15% increase in
opioid overdose deaths since the beginning of the pandemic, with jail and prison opioid overdose deaths
contributing to this uptick,24 and Colorado also noted an increase in overdoses in its jails and prisons while
under limited programming due to COVID-19.25 Formal overdose hospitalization and death information
for prisons and jails lags, but through participation in national organizations and workgroups, ISUDT
leaders are hearing from many correctional departments through informal reporting that non-fatal and
fatal overdoses have continued to increase during the pandemic.26 It should be noted that opioid-related
overdose deaths continue to be associated with illicit heroin and fentanyl not buprenorphine.
3. When CDCR and CCHCS returned near-normal operations in April 2021, and visitors and contractors were
again allowed access into prisons, the trend in declining overdose deaths and hospitalizations continued
unabated.
In addition to reductions in overdose deaths, hospitalizations due to overdose and substance use-associated
conditions dropped during the implementation of the ISUDT Program. The Department saw an average of
92 overdose hospitalizations per month per 100,000 residents between July and December 2019, the period
just prior to the increase in MAT participation under the ISUDT Program; however, overdose hospitalizations
dropped to 75 per 100,000 residents by the middle of 2021 (March 2021 through August 2021), an 18% decline
(p-value: 0.01).
24
https://www.northcarolinahealthnews.org/2020/08/25/is-it-time-to-provide-medication-assisted-treatment-in-nc-prisons/
Paul, J. (2021, December 13). A lot more drugs are being confiscated in Colorado prisons as inmates die from overdoses. The Colorado Sun. Retrieved from
https://coloradosun.com/2021/12/13/drugs-colorado-prisons-overdoses/
26
https://healthandjusticejournal.biomedcentral.com/track/pdf/10.1186/s40352-021-00138-6.pdf
25
16
V,
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
("')
Mar-19
:::!
)>
I.I)
V,
'Tl
::0
0
0
::0
::0
n
n
<
-,
C.
(1)
Q)
!:!?
m
C.
(.I)
m
0
Q)
-I
z
(.I)
I.I)
0
C:
V,
S'
Oct-21
n
....5·
Nov-21
;;,
:,
Sep-21
(1)
Aug-21
;::r
::!
V,
Jul-21
C.
Jun-21
:,
May-21
,...
s·
Apr-21
:,
Mar-21
0V,
..9
0
Feb-21
(1)
Jan-21
II
z
0
0
Dec-20
0
er
_o
:,
(I)
Nov-20
....0
....&i"
-,
Oct-20
-0
"2.
~~
,-
""O
0
Sep-20
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
V,
n
3
::0
)>
Jul-19
-n
N
,_.
ci"
0
Aug-20
m
~
Jun-19
'Tl
~
::0
0
'°I
I.I)
z
Jun-20
0
'Tl
C
z
Injection drug use commonly results in cellulitis, abscesses, and other types of acute and chronic infections,
often leading to hospitalization and expensive treatments. From July through December 2019, residents were
hospitalized for skin and soft tissue infections at a rate of 77 per 100,000. Subsequently after implementation
of ISUDT, from March through August 2021, the rate dropped to 61 per 100,000, a decrease of nearly 21%
(p-value: 0.03). Please see Figure 6.
Feb-19
Apr-19
G)
May-19
::0
A comparison of overdose outcomes for CDCR residents receiving MAT versus those who were on the MAT
evaluation waitlist, found the rate of overdose for MAT participants was 42% lower than those with SUD
on the MAT evaluation waitlist. The difference was even higher for people with AUD and OUD who were
participating in MAT; their risk of overdose declined by 48%.28 Please see Figure 7.
28
27
Per analysis conducted by Kim Lucas, PhD, Research Scientist IV, California Correctional Health Care Services.
Per analysis conducted by Justine Hutchinson, PhD, Research Scientist IV, California Correctional Health Care Services.
17
Similarly, the ISUDT Program has had a positive impact on patients with HCV infection. People with SUD,
especially OUD, who intravenously inject drugs are high-risk for HCV infection, which can lead to advanced
liver disease, liver failure, and premature death. The Department aggressively screens and treats residents
with HCV, but people with SUD who relapse after HCV treatment may again become infected, necessitating
additional courses of costly treatment, and again putting residents at risk for serious health complications.
ISUDT Program participants have lower risk of re-infection. The Department compared 1,212 MAT participants
who were post HCV treatment with 777 non-MAT residents who were post HCV treatment. Individuals
participating in MAT had a 29% lower HCV re-infection rate than patients not prescribed MAT.27
V,
~ 0
Q.l
::,
0
r+
Jul-20
NI.I)
-<
r+
Mar-20
-n
;:::;:
•
•
•
3
C
Feb-20
•
Nov-19
Oc
;;:io
s: n
"S!..
;:;·
(.I)
OJ
(I)
•
•
0
)> :,:,
0
::::j
Jan-20
•
)>~
~ -I
•
•
•
•
•
Q.l
I•
)>
•
:I:
(I)
I
,-
Oct-19
-,
I
""O
0
Dec-19
g;
0I.I)
Sep-19
Apr-20
I
'Tl
-I
m
::,
May-20
u,
C
I.I)
Aug-19
C:
I
Jan-19
....
N
8
8
u,
0
....
0
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
FIGURE 7. DRUG OVERDOSE RATE PER 100 PERSON YEARS PATIENT ON MAT WAITLIST VS ON MAT
3
2.66
...
cu
42% lower overdose
rate ff taking MAT
vs. on the waitlist
<II
(IJ
>;-
2.5
C:
0
...
<II
(IJ
a..
2
0
0
.......
1.54
~ 1.5
....cu
(IJ
0:::
(IJ
<II
0
...
1
"C
(IJ
>
0
0.5
0
On Waitlist
On MAT
Prior to 2019, the CDCR and most other state prison systems were experiencing steadily increasing overdose
deaths. With the implementation of the ISUDT Program, the Department’s trajectory is changing even as other
prison systems continue the trend of increasing overdose deaths.
Beyond the metrics, CDCR and CCHCS continue to receive positive input about this program from patients
and staff. For example, an institution Chief Medical Executive (CME) discussed how notifying residents’ family
members that their loved one has died of an overdose was a demoralizing part of his job. “I used to think,
‘What a waste. What a waste of life.’” ISUDT has brought a reprieve from this difficult task as the prison where
that CME works, has not had an overdose death in two years. The CME reports conversations with patients
now include stories about how they are repairing relationships. “What I hear from families, and more so from
patients, is that this reconnection is happening. Family had given up on them.”
Residents talk about how MAT has made it possible for them to more fully participate in rehabilitative
programs. “It’s that itch you wake up with in the morning, you know, and it is like, ‘Man, I just got to do
something,’” said one resident. “The Suboxone takes that out of it, out of my day, and I can focus on other
things, instead of constantly trying to hustle around to get high. Now I can focus on the things I need to do.”
Another stated, “This program is in short the best thing that has happened to me in the 20 years I’ve been
incarcerated. I’ve been off street drugs for six months and it’s the first time I’ve been off them since I was 15
years old.”29
29
Buis, K. (2021, Summer). In Their Own Words: ISUDT Feedback from the Incarcerated Population. The ISUDT Leader (1). Retrieved from: https://cchcs.ca.gov/wpcontent/uploads/sites/60/ISUDT/ISUDTLeader-Issue1.pdf
18
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
I
I
CHALLENGES & OPPORTUNITIES
The ISUDT Program is off
to a favorable start despite
significant challenges.
Moving forward, the
program will continue to
overcome challenges, and
seek to identify promising
opportunities to grow
through collaboration with
other statewide initiatives.
COVID – 19
The Department has made great strides to fully vaccinate more than 80% of residents. During the third week
of January 2022, the emergence of the hyper-contagious Omicron variant, resulted in nearly 6,000 COVID-19
cases among residents, and 4,400 staff cases statewide. In an effort to contain the virus, resident movement
was reduced and many institutions were again required to shift to modified programming, temporarily
suspending in-person CBI groups. However, due to the high vaccination rate among residents and infection
control polices, in-person CBI groups began reopening in early March 2022 and the Department is moving
forward from the Omicron surge.
REACHING ALL RESIDENTS WITH SUD
The next phase of the ISUDT Program will expand services from only residents in the highest risk categories to
all residents, which will require an increase in staffing. Even in the current model, which focuses on residents
scheduled for release within the next 15-24 months, those with the highest risk for overdose, and those who
arrive into the prison system already taking MAT, there was a backlog of more than 3,200 residents awaiting
evaluation for MAT as of early January 2022. The next ISUDT Program phase includes reaching residents who
arrive at CDCR with sentences too brief to allow participation in the full treatment program. Approximately
900 individuals per month come to the CDCR with between 7 and 14 months to serve, who are in need of
rehabilitative programming and SUD treatment. Under the current programming model, there is insufficient
time for these individuals to complete the full CBI model. Based on recommendations from national addiction
experts, the Department is developing evidence-based programming to provide a short-term SUD-focused CBI
component for this population that otherwise would not receive services. In addition to packet programming,
these individuals will have a regular check-in with an AOD counselor.
19
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
MEDICATION DELIVERY
As the program continues to screen CDCR residents for SUD, and more residents are determined to be eligible
for MAT based on rigorous clinical criteria, workload at medication lines will increase. Most MAT medications
are taken daily and each dose requires observation by CDCR and CCHCS staff. This can make medication lines
a time-consuming endeavor, which can be aggravating to residents who must wait in the same lines for other
critical medications. When institutions become overly stretched with the MAT workload and other activities,
such as managing Omicron outbreaks, adherence to protocols becomes difficult, and there are opportunities
for medication misuse. To support institutions, the ISUDT Program has initiated several efforts to collaborate
with the field to 1) identify best practices in medication line management within CDCR institutions and in
other large MAT systems around the nation, and 2) redesign and standardize medication line processes in
preparation for continued growth of the ISUDT Program and 3) continue to test patients on MAT to ensure they
are taking their medications. In 2021, of the more than 129,000 urine toxicology tests obtained from patients
on MAT, 97% of the test results showed that the patients were taking the Suboxone.
STANDARDIZING COORDINATION PROCESSES WITH COUNTY SYSTEMS
Prior to release from prison, Department staff assess ISUDT Program participants for their particular health
care needs, create an enhanced pre-release plan, and coordinate with county partners to ensure the success
of that plan upon the individual’s release from the CDCR. Each county has its own organizational structure
and network of programs available for people transitioning from prison, and many of these programs come
with their own distinct enrollment processes. Since residents housed at any one CDCR institution come from
a range of counties, the handoff process to the community is logistically complex. As part of implementing
the new enhanced pre-release planning process, ISUDT leaders are working toward standardizing handoff
processes as much as possible, collaborating with county partners to build a more efficient process. At the
end of March 2021, the ISUDT Program initiated a series of meetings with individual counties, focusing first
on those counties that receive the majority of CDCR releases including San Bernardino, Riverside, Orange,
Los Angeles, Sacramento, and Kern. These meetings have been helpful in getting a more detailed picture of
common concerns relative to warm handoffs (points of contact, data transfer/content, gaps in service). In
Sacramento, the enhanced pre-release team is starting to work on detailed communication protocols. Having
laid a strong foundation, the team is on track for significant handoff improvements in the major counties by
December 2021, with all remaining counties to follow.
PROVIDING TRAUMA INFORMED CARE
Research has demonstrated a link and strong graded relationship between adverse childhood experience
(ACE) such as violence, abuse, neglect, and growing up in a family with mental health or substance use
problems, and lifetime drug use. With each ACE an individual experienced, the likelihood for early initiation
of drug use increases by 2- to 4-fold. Compared with people with no ACE, people with 5 or more ACE were
7- to 10-times more likely to report drug use problems, addiction, and parenteral drug use. The portion
of drug use problems, addiction, and injection drug use attributed to ACE was calculated to be 56%, 64%,
and 67%, respectively. This indicates that one-half to two-thirds of SUDs could be attributable to ACE.30
Women, American Indians/Alaskan Natives, and Blacks are more likely to experience four or more ACE than
other groups. Because of the association between ACE and SUD, the federal CDC and other health care
organizations are designing programs to address trauma in the course of SUD health care service delivery,
referred to as trauma informed care. These programs include screening patients for trauma, developing
treatment plans that recognize and treat trauma, and helping patients develop positive coping skills. Trauma
20
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
informed care programs in correctional settings provide education and training to clinical and correctional staff
to assist them in effectively responding to trauma symptoms. While the nexus between trauma and SUD is
explored and addressed as part of CBI, CDCR is working to incorporate trauma informed care into the ISUDT
Program in other areas, such as clinical encounters and Supportive Housing, given the high prevalence of ACE
among CDCR’s residents.
MEDI–CAL EXPANSION PROJECTS
Two Medi-Cal expansion initiatives present
immediate opportunities between the CDCR
and the DHCS to improve services for the
justice-involved population in California.
•
The California MAT Expansion Project
seeks to address the rising number of
opioid overdose deaths in California
through increasing access to MAT, and
provide other prevention, treatment, and
recovery services.31 In particular, the MAT
Expansion offers resources to county health
care systems to build up MAT and SUD
treatment capacity, especially in historically
underserved communities, such as rural
counties and Native American populations. This will expand the network of treatment available to people
leaving the prison system and transitioning to county systems of care. In addition, the MAT Expansion
Project includes new data systems, which could assist CDCR and CCHCS in monitoring post-release
continuity of care.
•
California Advancing and Innovating Medi-Cal (CalAIM) is a Medi-Cal expansion program intended to
address social drivers of health and transform services for communities that have been historically
under- resourced and subject to structural racism in health care, among them the justice-involved.
CalAIM’s Enhanced Care Management benefit seeks to address the clinical and non-clinical needs of highneed Medi-Cal enrollees through intensive coordination of health care and health-related services and
engagement of enrollees where they live, seek care, or choose to access care. The Community Supports
aspect of CalAIM will allow counties greater capacity to provide assistance with housing supports and food
insecurity for Medi-Cal enrollees, increasing the available avenues for many formerly-incarcerated people
to get help with basic survival needs and mitigate risk of relapse.
Tilson, E. C. (2018, May). Adverse Childhood Experiences (ACEs): An Important Element of a Comprehensive Approach to the Opioid Crisis. North Carolina Medical
Journal, 79(3), 166-169. https://doi.org/10.18043/ncm.79.3.166
30
DHCS. (2021, September 8). The California MAT Expansion Project Overview. Retrieved from State Targeted Response to Opioid Crisis Grant:
https://www.dhcs.ca.gov/individuals/Pages/MAT-Expansion-Project.aspx
31
21
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
INITIATIVES TO REDUCE HOMELESSNESS
Formerly incarcerated persons already face a risk of relapse when they return to community environments
with established SUD risk factors; they are further tested when they struggle to find a stable home base from
which to continue SUD treatment, access other necessary health care services, and establish employment.
If previously incarcerated persons become homeless, recidivism also becomes more likely because there is
a close relationship between homelessness and incarceration; both are risk factors for the other.32 In 2021,
Governor Newsom committed $12 billion to address homelessness in California, with a focus on grants to
local governments, solutions for tent encampments, and the creation of more than 42,000 homeless housing
units. Part of the $100 billion California Comeback Plan, the initiative to tackle homelessness also offered
$10.3 billion for affordable housing.33 The Governor’s proposed budget released in January 2022 adds $2 billion
for mental health housing and services and another 10,000 housing units and treatment slots for homeless
people, as well as $2 billion toward affordable housing.34 The State’s investment in programs to decrease
homelessness and increase affordable housing supports efforts to establish stable home environments for
previously incarcerated individuals, increasing the likelihood that people with SUD will be able to continue
treatment.
IMPACTS ON VIOLENCE IN PRISON & OTHER CHRONIC DISEASE OUTCOMES
One of the goals of the ISUDT Program is to reduce the risk of violence affiliated with drug interdiction, debts,
and prolonged substance use, which may make prisons safer for residents and staff. To examine the impacts of
ISUDT on mitigating violence related to drugs in prison, the ISUDT Program will work with academic partners to
study violent incidents at the system-level, assessing aggregate trends pre- and post-program implementation.
This may also include disaggregated analyses focused on specific institutions of interest. CDCR/CCHCS will
also expand its evaluation of SUD treatment impacts on overall resident health, reviewing a broader range of
diseases and health outcomes.
POST–RELEASE IMPACTS
To understand the success of reintegration efforts and the impacts of the ISUDT Program beyond prison walls,
the Department needs access to a number of large state databases, which will require new or expanded datasharing partnerships with departments like the Department of Justice, California Department of Public Health,
the DHCS, the California Department of Health Care Access and Information (formerly the Office of Statewide
Health Planning and Development), Employment Development Department, and many county-level agencies.
This is the most ambitious data pooling effort CDCR and CCHCS has attempted, and it is slow process – The
Department will be looking for ways to accelerate this process in the coming year. With the assistance of
academic partners, CDCR and CCHCS will evaluate the impacts of the ISUDT Program on post-release outcomes
such as recidivism, relapse, hospitalization, mortality, housing, employment, and education.
32
National Health Care for the Homeless Council. (2013, November). Incarceration & Homelessness: A Revolving Door of Risk. In Focus: A Quarterly Research Review
of National HCH Council, 2:2. Nashville, TN: [Author: Sarah Knopf-Amelung]. Retrieved from https://nhchc.org/wp-content/uploads/2019/08/infocus_incarceration_
nov2013.pdf
33 Governor Newsom Signs Historic Housing and Homelessness Funding Package as Part of $100 Billion California Comeback. (2021, July 19). Retrieved from Office of
Governor Gavin Newsom: https://www.gov.ca.gov/2021/07/19/governor-newsom-signs-historic-housing-and-homelessness-funding-package-as-part-of-100-billioncalifornia-comeback-plan/
34
Office of Governor Gavin Newsom. (2022, January 10). Retrieved from Governor Newsom Releases California Blueprint to Take on the State’s Greatest Existential
Threats and Build on Historic Progress: https://www.gov.ca.gov/2022/01/10/governor-newsom-releases-california-blueprint-to-take-on-the-states-greatest-existentialthreats-and-build-on-historic-progress/
22
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
conclusion
The success of the ISUDT Program, two years into implementation is extraordinary; already, the program is
saving lives, reducing morbidity and other adverse outcomes for California prison residents that exceeds all
projections. This success is even more remarkable when it is taken into account that the program was
implemented with COVID-19 limitations.
This program has demonstrated the transformative power that comes with leadership, long-term vision,
investment, and large-scale collaboration. The ISUDT Program represents the dedication of CDCR and CCHCS
staff to the Department’s rehabilitative mission.
As the program moves forward, the Department will partner with other state and county agencies to measure
the impacts to public safety and successful reintegration into the community post-release. It is the hope of
CDCR and CCHCS leaders that not only will former ISUDT Program participants remain healthy, hold down
jobs, achieve stable housing, and form strong relationships with their family and friends, they will become the
embodiment of hope for their often disproportionately disadvantaged communities.
23
IMPACTS OF THE INTEGRATED SUBSTANCE USE DISORDER TREATMENT PROGRAM | 2019 — 2021
The California Department of Corrections and Rehabilitation manages California’s prison and
parole systems, which includes 34 correctional institutions stretching from the Oregon border
to the border of Mexico, with a population of approximately 100,000 incarcerated individuals.
The Department’s mission is to facilitate the successful reintegration to the individuals’ in the
Department’s care back to their communities equipped with the tools to be drug-free, healthy, and
employable members of society by providing education, treatment, rehabilitative, and restorative
justice programs, all in a safe and humane environment.
Learn more about CDCR at www.cdcr.ca.gov.
Health care services within California’s prison system are delivered in partnership with California
Correctional Health Care Services, the division run by Federal Court Receiver J. Clark Kelso,
appointed through the Plata vs. Newsom class action litigation.
Learn more about CCHCS at www.cchcs.ca.gov.
This report was written by the following California Correctional Health Care Services staff:
Renee Kanan, MD, MPH
Deputy Director, Medical Services
Annette Lambert
Deputy Director, Quality Management
Donna Kalauokalani, MD, MPH
Deputy Medical Executive, ISUDT/Complex Care
Denise Allen, MS, MA
Research Specialist IV
With Research, Data Analysis, and Other Contributions from:
Kim Lucas, MPH
Research Specialist IV
Spencer Puente
Research Data Manager
Ryan Jones
Research Data Manager
Ike Dodson
Information Officer II
Jenifer Espinoza
Health Program Manager III
Justine Hutchinson, PhD
Research Specialist IV
Marcus Dahlstrom, MD
Clinical Informaticist
Michelle Amaral, PhD
Research Data Supervisor II
Kyle Buis
Information Officer I
Kelsey Schultheis
Health Program Specialist II
ISUDT Executive Director
Lisa Heintz
Director, Legislative Affairs and Special Projects
California Correctional Health Care Services
ISUDT Project Director
Janene DelMundo
Information Technology Manager II
California Correctional Health Care Services
24