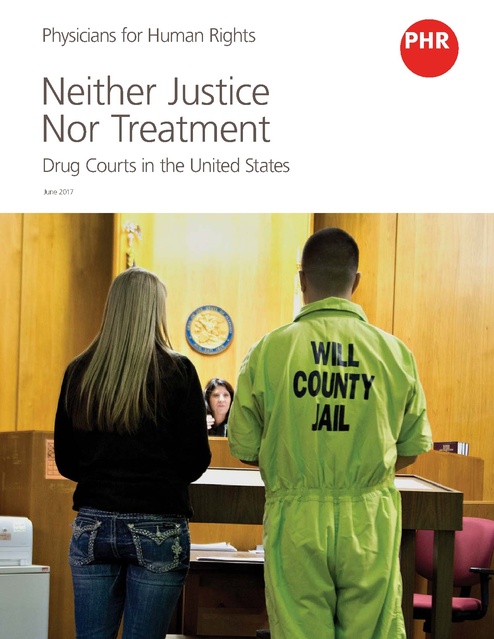
Physicians for Human Rights - Neither Justice Nor Treatment, 2017
Download original document:
Document text
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
Physicians for Human Rights Neither Justice Nor Treatment Drug Courts in the United States June 2017 There are more than 3,100 drug courts operating in the United States. But while the courts’ proponents say they reduce recidivism for people with substance use disorders, critics say the system abuses due process, often mandates treatment for people who don’t actually need it – people without drug dependence – and fails to provide quality care to many who do. Physicians for Human Rights (PHR) assessed the availability and quality of substance use disorder treatment through drug courts in three states – Florida, New Hampshire, and New York – and found major obstacles in all three states. Overall, PHR found that drug courts largely failed at providing treatment to those who truly needed it, and filled up limited treatment spaces with court-mandated patients who didn’t always need the care. In many cases, court officials with no medical background mandated inappropriate treatment, or mandated treatment for people who didn’t need it. In all cases, the functioning and mandate of the drug courts posed significant human rights concerns. Contents 3 Executive Summary 5 Methodology and Limitations 6 Background 8 Research Findings 20 Human Rights, Health Care, and Criminal Justice 21 Conclusion and Recommendations 22 Endnotes Cover: A sister and brother, both recovering from heroin addiction, appear before a judge during a session of drug court at the Will County Courthouse in Joliet, Illinois. Photo: Daniel Acker/Bloomberg via Getty Images. Acknowledgements This report was written by Marianne Møllmann, LLM, MSc, director of research and investigations at Physicians for Human Rights (PHR) and Christine Mehta, researcher at PHR. The research was carried out by the authors, assisted by Dorit Heimer, JD, research fellow at PHR. The report benefitted from review by PHR staff, including DeDe Dunevant, director of communications, Donna McKay, executive director, Susannah Sirkin, MEd, director of international policy and partnerships, and Homer Venters, MD, director of programs. Several PHR interns contributed invaluable research assistance for this report, including Anne Jacobs and Silvia Raithel. The report benefitted from external review by Rebecca Schleifer, JD, MPH, visiting fellow at Yale University Global Health Justice Partnership. The report was reviewed, edited, and prepared for publication by Claudia Rader, MS, content and marketing manager. Support for this report was provided by the Open Society Foundations. Executive Summary Richard, a 37-year-old who was sentenced to long-term residential treatment in New York for marijuana possession, was prescribed an inappropriate treatment plan by a drug court official with no medical background; according to his doctor, Richard has no addiction problem and doesn’t need treatment. A New Hampshire man who was desperate for drug treatment and rehab was refused admission to a treatment program because the prosecutor was determined to punish him with a prison sentence. His lawyer said the man became suicidal. And a Florida man who had struggled with heroin addiction for years was forced to detox in jail - a harrowing experience - because there was no room for him in Gainesville’s only detox facility. “I want to wait for my spot in detox,” he begged the judge, unsuccessfully, before being taken into custody. “I’ve been wanting to get help. I’ve detoxed in jail before … they don’t care if I die.” All three men were swept up in U.S. drug courts, specialized courts within the criminal justice system set up to provide alternative sentencing options – treatment instead of jail or prison time – for people charged with criminal behavior linked to drug possession, sale, or addiction. The first courts were opened in 1989 to ease dockets and jails that were overflowing as a result of strict federal and state laws passed in the 1980s in an attempt to reduce drug supply and consumption. Almost three decades later, there are more than 3,100 drug courts operating in the United States. But while the courts’ proponents say they reduce recidivism for people with substance use disorders, critics say the system abuses due process, often mandates treatment for people who don’t actually need it – people without drug dependence – and fails to provide quality care to many who do. Physicians for Human Rights (PHR) assessed the availability and quality of substance use disorder treatment through drug courts in three states – New York, New Hampshire, and Florida , chosen for the diversity of their drug court and health system approaches – and found major obstacles to quality evidence-based treatment for drug court participants in all three states. Overall, PHR found that drug courts largely failed at providing treatment to those who truly needed it, and filled up limited treatment spaces with courtmandated patients who didn’t always need the care. In many cases, court officials with no medical background mandated inappropriate treatment not rooted in the evidence base, or mandated treatment for people who didn’t need it. In all cases, the functioning and mandate of the drug courts posed significant human rights concerns. than deviant, drug court participants were often punished for relapsing, missing therapy appointments, or otherwise failing to follow court rules. One key concern motivating this research was whether drug courts were able to appropriately diagnose and facilitate treatment for people with substance use disorders who are in conflict with the law. We found that, in many cases, they are not. Diagnosis and initial treatment plans for drug court participants were often developed by people with no medical training or oversight, at times resulting in mandated treatment that was directly at odds with medical knowledge and recommendations. The most egregious example of this was the refusal, delay, or curbing of medication-assisted treatment (MAT) (also known as substitution or replacement therapy) to people with opioid use disorders, despite evidence that treatment for such disorders in many cases requires long-term – sometimes permanent – medication. Some drug courts also prevented participants from accessing or staying on medically prescribed treatment for anxiety, Attention Deficit Hyperactivity Disorder, and other chronic health problems. Ironically, the form of MAT that appeared to have the most support in many of the drug courts visited – an injectable form of naltrexone, Vivitrol – has the weakest evidence base of all Food and Drug Administrationapproved treatments for opioid dependence. Most drug courts visited by PHR operated in communities where the understanding of addiction treatment, including amongst treatment providers, varied widely. This, however, cannot justify a system where non-clinical staff drive treatment decisions. PHR found that drug court teams at times dismissed legitimate medical opinion, with potential harm to the patient. Even where drug court team members were knowledgeable about best practices for evidence-based treatment and mandated appropriate treatment, some court participants could not receive the care they needed because they didn’t have sufficient insurance coverage and could not afford the treatment otherwise. Participants in Florida, one of 19 states that did not choose to expand Medicaid, could not use Medicaid to access treatment. Even in New York, which did undertake Medicaid expansion, one man said he could not get methadone treatment for his opioid-addicted wife because she had the wrong kind of Medicaid coverage, and treatment center staff spoke to complicated application processes and uncertainty that was particularly hard to navigate for people suffering from addiction. At the most basic level, PHR found that access to quality treatment was hampered by the inherent tension between a punitive criminal justice logic and therapeutic concern for drug court participants as patients. In fact, despite the stated intention of drug courts to treat people who use drugs as ill rather Another obstacle was the serious lack of quality treatment options in the communities served by drug courts. In communities visited by PHR where evidence-based treatment theoretically was available, all residential, in-patient, and detox treatment facilities had waiting lists. For people seeking treatment voluntarily without a court mandate, waiting lists could be months. As a result, for many people with problematic drug use, PHR found Neither Justice Nor Treatment Physicians for Human Rights phr.org 3 Executive Summary continued that drug courts were indeed the most viable route to treatment, giving at least some people access to care they otherwise would not be able to obtain. This creates a perverse incentive to commit a crime in order to access care, something not lost on several drug court participants. But this access to care came at the cost of participants waiving their rights. In general, PHR found that the delivery of essential health care and treatment through the criminal justice system raised several human rights concerns, including, specifically, questions regarding patient confidentiality and autonomy, dual loyalty, privacy, and the ability of the patient to give meaningful consent to treatment. U.S. federal law specifically protects the confidentiality of drug and alcohol abuse treatment and prevention records, but provides broad exceptions to this rule. Notably, while treatment providers usually are covered by federal confidentiality regulations, drug court team members are exempt. Moreover, all drug court participants were asked to waive patient-doctor confidentiality as a condition for drug court participation, and PHR observed patient information openly discussed in court, even at times without relevance to the person’s drug use, addiction, or alleged criminal behavior. International human rights law protects the right to physical autonomy, including the right to refuse medical treatment. This principle is routinely flouted in drug courts. The treatment provided in drug courts is touted by proponents as voluntary, because participants are “free” to choose jail or prison over drug court participation. However, many participants PHR spoke to felt forced to enter the drug court treatment programs to avoid lengthy legal proceedings, and, in order to do so, were required to plead guilty to charges that had never been investigated. The criminalization of possession of certain drugs for personal consumption also meant that many people who got caught up in the criminal justice system – and ended up in drug courts – did not suffer from substance use disorders or didn’t want treatment. In some cases – such as, for example, in Florida – the law explicitly allows for the involuntary commitment and treatment of people by reference to harm or criminal behavior that hasn’t happened yet. Human rights concerns are thus particularly relevant for drug courts, as these courts blur the line between voluntary and coerced treatment, and compel participants to waive the right to confidentiality. Furthermore, most drug courts operate with regulations that subject medical expertise and advice regarding treatment to prosecutorial oversight and potential veto, raising questions about a person’s ability to access impartial evidencebased care. Even where courts did not actively violate human rights protections of their participants, the regulatory set-up constantly threatened such violations. Neither Justice Nor Treatment There are also other reasons to be skeptical of the criminal justice system as deliverer of treatment for the growing part of the U.S. population that suffers from addiction. Certainly, it is not the most cost-effective way to facilitate access to care, whether the costs of punitive sanctions and supervision are borne by drug court participants or the state. Either way, treatment without jail and parole would be cheaper. Moreover, improving social services (case management) and insurance, while combatting stigma around drug use, would have at least an equally beneficial and certainly more direct effect on people with serious substance use disorders. The criminal justice system’s conflation of drug possession and personal use with clinical need for care has done nothing to ensure treatment for those who truly need it. Ultimately, people with substance use disorders who get treatment through the criminal justice system are still treated as criminals, and the symptoms of their illness punished as if the illness itself were a crime. Until the criminal justice system delinks possession of drugs for personal use from criminal behavior such as larceny, theft, and assault, it will be particularly hard to deliver quality care to the high-need population that drug courts purport to serve. An approach more respectful of human rights and medical ethics demands that the Department of Justice prioritize harm reduction initiatives over criminal justice approaches to drug use. Further, Congress should enact legislation that expands access to voluntary care for people with substance use disorders, and insurance companies and Medicaid should be required to cover all evidence-based care for those who need it. People with substance use disorders who get treatment through the criminal justice system are still treated as criminals, and the symptoms of their illness punished as if the illness itself were a crime. Physicians for Human Rights phr.org 4 Methodology and Limitations Three Physicians for Human Rights (PHR) researchers conducted interviews, both in person and over the phone, with health care professionals, social workers, judges, lawyers, drug court staff, and drug court participants, predominantly in three U.S. states: Florida, New Hampshire, and New York. These three states were chosen to provide an overview of drug courts in states with different health care systems, and with different histories of drug court engagement and funding. Florida has a mature system of drug courts, with the very first drug court in the United States established there in 1989, and operates in a context of limited funding for health care, in particular for people with substance use disorders. As of April 2017, there were 95 drug courts in Florida.1 New York equally has decades of history with drug courts, and has recently passed legislation to ensure access to medication-assisted treatment. There were 141 drug courts in New York State as of January 2017.2 New Hampshire has the newest drug court system, yet is one of the states with the highest overdose rates in the country. As of April 2017, there were seven drug courts in New Hampshire.3 New York and New Hampshire opted to expand Medicaid through the Affordable Care Act, thus theoretically expanding access to voluntary treatment. Florida, however, has not. We anticipated that these diverse contexts would give a good overview of barriers to treatment faced in different parts of the country. PHR observed proceedings of several drug courts, including closed meetings of drug court team evaluations of drug court participants. Researchers also interviewed representatives from national medical associations, associations of people who use drugs, U.S. and international addiction experts, researchers, and others with professional knowledge of drug court history and functioning, addiction medicine, criminal justice diversion programs, and substance use disorders. These interviews were carried out between July 2016 and March 2017. In total, we conducted approximately 170 interviews, including 41 interviews with drug court participants, and observed court proceedings directly in 15 drug courts. Respondents were selected through a convenience sample. We contacted all registered treatment providers working with drug court participants in each state for whom information was available on official websites and listings, and spoke to those who indicated interest. For Florida and New Hampshire, we contacted all drug courts. In New York, the statewide drug court coordinator denied PHR permission to speak directly with drug court staff, so we instead contacted public defenders, police chiefs, prosecutors, and others working directly with drug courts. In all three states, we reached out to harm reduction specialists and drug court evaluators. Neither Justice Nor Treatment The research methodology was designed to surface research questions and concerns that merit further investigation. Given the diversity of drug courts and contexts, the results may not be generalizable or representative of all drug courts. In New Hampshire and Florida, the statewide drug court coordinators encouraged full participation in the study by drug court teams, leading to a higher participation rate than in New York State, where we were not permitted to interview New York state drug court staff. Likewise, New Hampshire and Florida authorities shared data and information with PHR, whereas New York authorities did not respond to several requests for data beyond an initial acknowledgement that the request had been received. For all interviews, PHR researchers obtained informed oral consent following a detailed explanation of PHR, the purpose of the investigation, and the potential benefits and risks of participation. Interviews were conducted using semi-structured interview instruments developed by PHR medical and legal experts and approved by PHR’s Ethics Review Board (ERB), a body established in 1996 to ensure the protection of individual witnesses interviewed during the course of investigations and research. PHR’s ERB regulations are based on Title 45 CRF part 46 provisions, which are used by academic Institutional Review Boards. In addition, PHR researchers reviewed existing research on drug courts, access to treatment for substance use disorders inside and outside the criminal justice system, and peer-reviewed research on treatment for substance use disorders. We reviewed drug court regulations, state evaluations, handbooks, and manuals shared by the drug court coordinators from New Hampshire and Florida, and those materials available to the public online in all three states. This report is about the availability and quality of substance use disorder treatment through drug courts. Some participants PHR studied were diverted into drug courts because of alleged illegal use of legal substances (e.g. driving under the influence of alcohol, or misuse of prescription drugs). Others were alleged to have committed crimes thought to be related to the possession, sale, purchase, or use of substances that are considered “illicit” (e.g. stealing to fund a drug habit). For the purposes of this report, our concern is whether drug courts were able to appropriately diagnose and facilitate treatment for substance use disorders, whatever the substance. While the delivery of health care through the criminal justice system raises human rights concerns, the overall adverse human rights consequences of the criminalization of personal substance use have been covered elsewhere and are not addressed in this report.4 The names of all drug court participants have been changed in the interest of their privacy. Where requested, the names of treatment providers and other drug court actors have been withheld. PHR is deeply grateful to the many individuals who took the time to share their expertise, concerns, and deliberations with us. Physicians for Human Rights phr.org 5 Background Drug Policy in the United States History of U.S. Drug Courts Since the 1980s, U.S. drug policy has sought to reduce drug supply and consumption primarily through law enforcement,5 resulting in strict and strictly enforced criminal laws punishing the possession of even small amounts of illegal drugs. An overview of the criminal law provisions covering personal drug possession published in October 2016 noted that “all US states and the federal government criminalize possession of illicit drugs for personal use” and that “in 42 states, possession of small amounts of most illicit drugs other than marijuana is either always or sometimes a felony offense.”6 Drug courts (sometimes called treatment courts) are specialized courts within the criminal justice system, set up to provide an alternative to incarceration for people arrested for offenses where problematic drug use is considered an underlying cause of the crime. The first drug court was established in Miami, Florida in 1989 in an effort to reduce overflowing dockets and jails.13 The narrative in support of criminalizing personal drug use assumes that abstinence from illegal drugs is imperative for the health of the individual and for society as a whole.7 Law enforcement strategies in the United States have integrated this assumption, most notably with the rise of theories like “broken windows policing,” which have led to policing practices that target low-level crimes deemed to be “anti-social,” including drug possession for personal use, especially marijuana.8 The push for abstinence has not been particularly successful. Studies show that “abstinence” as a policy option requires a substantial investment in treatment and social services to effect a reduction in drug use.9 From a public health perspective, some people cannot or will not choose to stop using drugs, and forcing them to do so may put them at risk of more harm, including overdose if they resume using after detoxing. Moreover, many addiction specialists note that the majority of people who use drugs do not develop a drug dependency or addiction.10 Over the past five to 10 years, some jurisdictions – including the federal government – have started to invest in harm-reduction interventions,11 which are not focused on reducing drug use but rather on reducing the harm of problematic drug use on individuals and society.12 In addition, some jurisdictions have increasingly invested in treatment through court-supervised treatment options, thereby blurring the lines between law enforcement and treatment and giving rise to the proliferation of drug courts. Neither Justice Nor Treatment Most drug court programs loosely resemble community-based probation programs but include intensive court supervision (usually presided over by a judge), drug testing, and a mandated “treatment” program. Under the drug court model, judges and other court personnel monitor a participant’s treatment and program compliance, and judges can impose immediate sanctions if participants fail to comply with the program’s requirements.14 There are several types of specialized drug courts, including adult, juvenile, family dependency, felony, misdemeanor, and pre-plea or post-plea. In many cases, participants must plead guilty to the crime they are charged with in order to be diverted to the drug court, with the understanding that charges will be reduced or dismissed if they successfully complete all conditions of the court program. As of mid-2015, there were 3,133 drug courts operating in the United States, the majority of which target adults.15 Drug courts vary substantially across a number of areas: eligibility criteria, target population, treatment options, sanctions and incentives schedule, success criteria, and funding. However, most share the stated dual objective of reducing incarceration and facilitating access to treatment for people whose drug use is an underlying cause of criminal behavior. The National Association of Drug Court Professionals (NADCP), a not-for-profit organization that has advocated for the drug court model since 1994, adds an implied financial objective in its evaluation of why it believes the drug court model works: “By keeping drug-addicted offenders out of jail and in treatment Drug Courts have been proven to reduce drug abuse and crime while saving money.”16 Many courts insist that people who have been arrested for drug-related offenses stop using drugs – including legal drugs such as alcohol and prescribed medication – as a condition for the removal of court supervision and probation.17 In fact, the NADCP highlights ensuring abstinence as one of 10 key components of the U.S. drug court model.18 Physicians for Human Rights phr.org 6 Background continued In 2015, the NADCP introduced national standards for best practices in drug courts for the first time. The organization acknowledged that its initial focus had been to grow the model even before it had been deemed successful. In an article published in the Pacific Standard Magazine, then NADCP Director of Standards (now Chief Operating Officer) Terrence Walton was cited as saying: “The aim of the first couple [of] decades of drug courts was to spread drug courts. We said, ‘We want a drug court in reach of every individual in need.’ Well, now that we have almost 3,000 drug courts across the country and in every single state, we want a drug court that works in reach of everyone in need.”19 Now, the drug court model has been one of the most heavilystudied justice mechanisms in the United States.20 Most evaluations have found that drug courts are more cost-effective than conventional incarceration but have not looked at a comparison with community-based probation or indeed at the cost associated with quality evidence-based treatment.21 Further, most studies deal with the question of how well drug courts are implemented based on the evolution of best practices by the NADCP. There is little data on the quality of treatment provided, or on drug courts’ effects on the participants’ long-term recovery from problematic drug use, or social relationships, employment, and general health.22 No drug court evaluation has compared the courts to public health and harm-reduction approaches. The Opioid Crisis: An Impetus for Change The United States has experienced a rise in opioid use and overdose deaths since the mid-2000s,23 which prompted Congress to pass the Comprehensive Addiction and Recovery Act (Public Law No. 114-198) in 2016.24 The law provided for expanded access to naloxone (used to prevent opioid overdose),25 encouraged awareness-raising around the misuse of opioid-based pain medication, and directed the Department of Justice to fund state and local initiatives that expand treatment alternatives to incarceration and support collaboration between criminal justice and treatment providers, including drug courts.26 The law also directed the White House Office of National Drug Control Policy to expand grants to allow states and local governments to address a spike in opioid and methamphetamine usage and overdose.27 This office has been targeted for elimination by the Trump administration.28 Some states were prompted by the rise in overdose deaths to change their approach to drug use, including through increased funding for drug courts,29 and – less frequently – pre-booking or pre-arrest diversion initiatives such as the Law Enforcement Assisted Diversion programs in King County, Washington; Santa Fe, New Mexico; and Albany, New York;30 and the “angel” program in Gloucester, Massachusetts.31 At the same time, many states and counties remain resistant to diversion and alternative sentencing programs, fearing that public safety may be compromised. This is the climate in which drug courts are being promoted as fulfilling both the public safety objective of the criminal justice system and the urgent need for treatment highlighted by the increase in opioid use and overdoses. In this report, we evaluate the treatment element of that equation. “Now that we have almost 3,000 drug courts across the country and in every single state, we want a drug court that works in reach of everyone in need.” A police officer holds a bag of confiscated heroin in Gloucester, MA, in 2016, where the so-called “Angel Program” diverts people with problematic drug use away from the criminal justice system without arrest or threat of prison. Photo: John Moore/Getty Images Neither Justice Nor Treatment Terrence Walton, Chief Operating Officer, National Association of Drug Court Professionals Physicians for Human Rights phr.org 7 Research Findings Participants in the drug courts visited by Physicians for Human Rights (PHR) faced multiple barriers to accessing quality, evidence-based diagnosis and care. Barriers varied considerably between states, and even between counties, and ranged from appropriate diagnosis and care being completely unavailable, to care being insufficient, financially inaccessible, inadequately supported by evidence, or uncovered by insurance, including, at times, Medicaid. Some of the interventions that have proven most effective in setting people with substance use disorders on the road to recovery – such as adequate case management, support for stable housing, and steady employment, as well as medicationassisted treatment (MAT) where appropriate – were either not available at all, or were not available in sufficient quantity. The very population meant to benefit from the treatment provided through the drug courts – people with a high level of addiction at escalated risk of re-offending – face additional barriers in even participating in these courts in some jurisdictions because of funding constraints as well as prosecutorial wariness of allowing “high-risk, high-need” individuals to participate in treatment.32 PHR’s research also documented a number of systemic issues that directly undermined the effectiveness of drug courts as currently set up. A central drug court premise – people who commit crimes to sustain problematic drug use should be treated as sick, not criminal – did not always permeate the court proceedings. In one assessment of drug courts, a key conclusion was that “the particular treatment methodology used in drug courts [did] not attempt to separate punishment from treatment but rather conflate[d] the two,” and that courts would not be effective until this tension was resolved.33 Barriers to High Quality Evidence-Based Diagnosis and Care The treatment offered in drug courts has taken various shapes over time and across jurisdictions. In the courts visited and observed by PHR, it did not always include access to medicallyassisted treatment, psychosocial therapy or counseling, or a level of treatment appropriate to the severity of the addiction manifested in each drug court participant – all approaches known to be effective. This discrepancy between evidence-based treatment for substance use disorders and the treatment provided to drug court participants had various roots: inadequate or unfunded treatment options (also outside of the courts); inappropriate plans mandated by courts without reference to medical science and evidence; inappropriate surveillance or probation responsibilities for treatment providers; lack of ancillary services like housing and employment; deficient insurance coverage; and treatment centers providing treatment without reference to evidencebased practices. People who use drugs who are considered high-need and high-risk – ostensibly the population drug courts are primarily set up to serve – encounter particular problems in accessing appropriate treatment through drug courts, facing both regulatory and financial obstacles. Each of these elements are explored below. In PHR’s research, drug court participants who tested positive for the use of drugs were generally either kept from advancing to the next phase of the program – extending their time under strict court supervision sometimes to longer than they would have served in jail for the crime they were charged with – or punished with jail time, essay writing, or additional court time or supervision. This converted relapse to drug use into a moral failure subject to criminal sanction, as opposed to a common part of the recovery process, as defined by the American Society of Addiction Medicine (ASAM).34 We also documented lack of appropriate support for housing, education, job search, and other essential case management, which, in drug court evaluations, has been shown to be critical to long-term recovery. In many of the situations documented by PHR, the drug court participants’ rights to privacy, physical integrity, and health were at risk. Where treatment compliance was enforced by threat of severe punitive action, or coerced by law, both medical ethics and human rights protections were directly violated. Neither Justice Nor Treatment This woman, showing her kit of clean needles, mixing cap, and tourniquet, says she has tried to get treatment for her heroin addiction, but was unable to secure a bed in a treatment facility or to meet the drug test requirements of the treatment provider. Homeless, she lives under a bridge in Philadelphia, which is in the midst of an opioid epidemic. Photo: Dominick Reuter/AFP/Getty Images Physicians for Human Rights phr.org 8 Research Findings continued What is evidence-based treatment? Availability and Funding of Treatment Options The underlying premise for drug courts is that they provide treatment for people whose substance use and criminal behavior are caused by a chronic brain disease: substance use disorder.35 Substance use disorder was included in the Diagnostic and Statistical Manual for Mental Disorders (DSM-5), the manual published by the American Psychiatric Association which classifies currently acknowledged mental disorders and their components, with a list of 11 criteria used to determine the existence and severity of the disorder.36 A first and underlying obstacle to quality care for drug court participants was the paucity of quality care options in the communities served by the courts. Most interviewees pointed to a significant treatment gap, especially for low-income people with substance use disorders. All residential, inpatient, and detox treatment facilities in communities visited by PHR had waiting lists. In fact, for people seeking treatment voluntarily without a court mandate, waiting lists could be months. Outpatient services, if available, often had shorter waiting lists, but provided a lower level of care. The net result was a dearth of available care option for people with substance use disorders who wanted treatment. There is general clinical and scientific consensus regarding the continuum of care that is most appropriate to treat addiction,37 including the notion that the evidence base is stronger for the treatment of opioids than for marijuana, methamphetamine, cocaine, and other stimulants. For opioid disorders, specifically, the Food and Drug Administration has approved three medications to be used in combination with psychosocial treatment, namely methadone, buprenorphine, and naltrexone (oral and injectable).38 Vivitrol, an extended-release injectable form of naltrexone, is a newer form of medicationassisted treatment, which has gained popularity in some drug courts without the same evidence base as methadone and buprenorphine. The World Health Organization notes in its List of Essential Medicines that both methadone and buprenorphine “should only be used within an established support programme.”39 Neither Justice Nor Treatment This fact is echoed in available data. In 2013, 2014, and 2015, the federal Substance Abuse and Mental Health Administration referred to a treatment and service gap in its annual announcement of discretionary grants. In New Hampshire, specifically, a 2014 assessment found that all treatment providers in the state, including methadone clinics, operated with waiting lists.40 The assessment surveyed all treatment providers in the state and also found a universal desire to expand capacity, but a wariness to do so without assurance of adequate funding, either through adequate insurance reimbursements or increased funding from the state.41 Many interviewees cited particular difficulties in accessing MAT, especially methadone. In New Hampshire, there were just eight methadone clinics operating in the state, all of them located in the southern half of the state.42 According to public information, there were 36 methadone clinics in Florida, but several counties where drug courts were operating lacked methadone clinics.43 In New York, methadone treatment was particularly scarce upstate, with one journalistic assessment noting in 2016 that in Syracuse, for example, it was easier to access heroin than treatment.44 In New York, methadone treatment was particularly scarce upstate, with one journalistic assessment noting in 2016 that in Syracuse, for example, it was easier to access heroin than treatment Physicians for Human Rights phr.org 9 Research Findings continued In efforts to meet the increasing need for substance abuse treatment for opioid users, in 2016 the Department of Health and Human Services raised the number of patients that licensed buprenorphine providers were able to treat at one time from 100 patients to 275.45 Dr. Laura Martin, in Syracuse, said the rule had eased long waiting lists for people seeking buprenorphine, but because of onerous licensing procedures and stigma, doctors in upstate New York were wary about becoming licensed to prescribe buprenorphine and treat people with substance use disorders. “The truth is many providers have misperceptions about the type of people who need treatment for addiction. If you’re a regular family doctor, you fear homeless people sleeping in your waiting room, or drug deals happening in your office. In reality, it’s not like that. I would like to see other doctors understand that a little more,” Dr. Martin said.46 Access to legally prescribed buprenorphine has remained low over the past 10 years in the three states covered in this report, as measured by the percentage of the population that certified prescribers of buprenorphine are able to cover.47 In Florida and New York, certified prescribers could reach less than 0.1 percent of the population in 2015. Only in New Hampshire did the number of certified prescribers grow, doubling their reach to 0.3 percent of the population in 2016 from 0.16 percent in 2015. The dearth of certified providers meant that not all providers had time to supplement the prescription of buprenorphine or methadone with counseling, as recommended by the World Health Organization (WHO). In fact, PHR found that some providers ostensibly delivering MAT wrote prescriptions but had very little other time for the patients at all. Alex Casale, state drug court coordinator in New Hampshire, noted: “Many [clinics] are private and still don’t provide counseling. There is … a Suboxone48 clinic, they don’t take insurance, and they don’t give therapy. They charge 70 dollars a week, and give someone drugs. That is not MAT: that is just giving someone drugs.”49 refused care on the basis of how many “failures” (i.e. relapses) the patient had during various levels of care: outpatient, inpatient, and residential. “First they didn’t take her because she didn’t have enough failure in outpatient, then because she didn’t have enough failures in inpatient, then there was a million people ahead of her, then Medicaid wasn’t the right kind and didn’t cover.”50 Health providers PHR spoke to confirmed that patients usually would have to “fail” less intensive care options before higher levels of care were authorized, even if the health care providers recommended the more intensive option. Generally, interviewees in New York and New Hampshire pointed to Medicaid expansion as helping to defray the costs of care for some drug court participants. In Florida, it was another story. Florida was one of 19 states that chose not to expand Medicaid through the Affordable Care Act (ACA), so most drug court participants were not eligible for Medicaid and few had private insurance. As a result, treatment provided through drug courts in Florida was either funded by the counties, or relied on state funds through the Department of Children and Families. MAT, in particular, was prohibitively costly unless covered by insurance. For example, Vivitrol, an injectable form of naltrexone, cost up to $1,000 for a monthly shot.51 In 2014, the Florida state legislature dedicated $1 million of additional funding every year to provide Vivitrol to treat alcohol and opioid-addicted people under criminal justice supervision, either through drug courts or probation. However, David Adan, the clinical supervisor at Banyan Health Systems in Miami, which provides care for courtmandated clients in Miami-Dade County, Florida, said the funds allocated to his clinic were enough for just six clients, and that his funding would run out in May 2017.52 Drug court participants, team members, and treatment providers all highlighted lack of funding for treatment of substance use disorders as a massive hurdle to much-needed care both inside and outside drug courts. Several drug court participants told PHR they had sought care outside of the criminal justice system, but had been unable to pay the cost. Richard, a 37-yearold drug court participant in upstate New York, told PHR of his unsuccessful efforts to secure methadone treatment for his wife, who had become addicted to prescription opioids after a shoulder operation. He described a typical sequence of being Court-mandated tests were also costly to drug court participants. Shayanne, a 23-year-old drug court participant in New Hampshire whose partner was also in court-mandated treatment, told PHR: “I have private insurance, but my partner has Medicaid, which covers 100 percent of the drug tests and screenings. I have a copayment for mine since I have private insurance, I just got a bill for $108 for each test.”53 Jim, a 32-year-old man in court-mandated residential treatment in New York, told PHR the payment demands could be onerous and unpredictable: “A lot of people have problems when it comes to testing day, we have to pay for it, $40-$120. Some days it goes to your treatment facility, then your insurance covers it. But sometimes they want you to go to the county.... They tell you to keep a money order on you in case your number comes up [i.e. you are randomly selected for testing].”54 Neither Justice Nor Treatment Physicians for Human Rights phr.org 10 Research Findings continued Failure to Adhere to Evidence-Based Treatment In some drug courts PHR visited, the same treatment plan was mandated for most participants, regardless of the severity of their addiction level, while in others, non-medical staff recommended treatment plans later deemed unhelpful by the medical providers asked to implement them. Richard, a 37-year-old man in courtmandated long-term residential treatment in New York for marijuana possession, told PHR his court-mandated treatment plan was dismissed as inappropriate by his doctor. Richard said: “It was just the drug court coordinator [who diagnosed me] who has no degree or anything, and then when I came to see the actual doctor [at the treatment center] who is a professional, he says, you have no [addiction] problem.”55 The medical director at the treatment facility Richard was assigned to by the court confirmed to PHR that the treatment plan drawn up for Richard by the drug court was inappropriate.56 City, said that she and colleagues at times suggested treatment options for expediency rather than therapeutic reasons: “Did we consult a medical professional? No. It’s more of a legal determination. Really, what we are looking for is anything that can help [the client’s] legal objectives…. No one is really making a determination [about treatment] that’s medical.”57 “Did we consult a medical professional? No. It’s more of a legal determination. Really, what we are looking for is anything that can help [the client’s] legal objectives…. No one is really making a determination [about treatment] that’s medical.” In fact, as drug courts are part of the criminal justice system, treatment plans were negotiables between defense lawyers and prosecutors. Emma Ketteringham, a defense attorney in New York Emma Ketteringham, New York City defense attorney Detoxing in Jail Where drug court participants are required to detoxify before they can enter treatment, many were forced to go through withdrawal in jail and without medical supervision. The Office of Alcoholism and Substance Abuse Services in New York sets out clear guidelines for detoxification, including mandatory medical supervision, to avoid health complications or even death.58 Joshua, a white male in his early 30s, had been using heroin for about seven years before being arrested in Gainesville, Florida. One of the case managers at the Alachua County drug court, who are tasked with making treatment recommendations, assessed Joshua to be a high-need participant and recommended him for long-term residential treatment. With only one detox facility in Gainesville, and a waiting list of several weeks for Metamorphosis, the residential treatment center, the drug court team decided to Neither Justice Nor Treatment keep Joshua in custody while he waited for a bed – for his own safety, they said. Joshua stood before the presiding drug court judge, ready to plead guilty in order to access the drug court’s program. But when he heard he would have to detox in jail – which can be a grueling process – he began to beg, “I really don’t want to detox in jail, please … I want to wait for my spot in detox and then go into Meta[morphosis]. I’ve been wanting to get help. I’ve detoxed in jail before … they don’t care if I die.” Judge Walter M. Green cut him off, saying, “You need to make a decision right now … if you’re thinking you want to go home and use one more time … I can tell you the consequences of not going into treatment today, right now … [You will overdose] … you’re lucky to be alive, given your IV use.” Facing prosecution for heroin possession, a felony, and grand theft, Joshua chose to be taken into custody and detox in jail. In Hillsborough County, New Hampshire, 23 year-old Shayanne was poised to graduate from drug court after more than a year in the program. “My son’s first birthday is the day before I graduate, so it will be a great time,” she said. Her son, she said, is the reason she decided to cooperate with drug court treatment and quit heroin, a drug she had been addicted to since she was 17 years old. Pregnant at the time of her arrest, Shayanne knew the Department of Children and Families could take her baby away as soon as he was born if she didn’t stop using drugs. She detoxed in jail, a harrowing experience. “I detoxed without methadone because I didn’t want my son to have to detox when he was born. I chose not to take methadone, but the jail staff gave me no help either … one time, I was bleeding in my cell, and I was afraid I was having a miscarriage. All they told me to do was put my jumpsuit in a biohazard bag so they could weigh how much blood I had lost.” Physicians for Human Rights phr.org 11 Research Findings continued Drug courts came up particularly short when it came to participants who use marijuana, in part because there are no known effective, evidence-based treatments for marijuana dependence.59 In New York, many individuals landed in drug court programs because of marijuana possession charges, and even more were kept from graduating from drug courts because of marijuana use. A substantial number of these participants did not present indications of marijuana dependence. In fact, several New York-based treatment providers told PHR they were frustrated that people in court-mandated “treatment” for marijuana use took up seats in programs they could not benefit from, while people with opioid dependence were “literally dying” because they couldn’t access treatment.60 Despite buprenorphine’s proven record in curbing opioid cravings, PHR found that some drug courts refused to include medication-assisted treatment, including buprenorphine, in the treatment options available to drug court participants. Photo: Joe Raedle/Getty Images Neither Justice Nor Treatment Specific Barriers Related to Medication-Assisted Treatment The lack of reference to best practices in treatment of substance dependence in the drug courts was particularly pronounced with regard to access to MAT, notably methadone and orally administered buprenorphine. This is despite the fact that methadone and buprenorphine have a strong evidence base for successfully preventing relapse for opioid dependence, and have been placed on the WHO model list of essential medicines.61 A 2013 national survey of the availability of, barriers to, and need for MAT for opioid addiction in drug courts (especially methadone and buprenorphine) concluded that while almost all drug courts had participants diagnosed with opioid use disorders, only 47 percent of courts offered agonist medication (notably methadone), with a slightly higher percentage (56 percent) offering MAT of some kind.62 Similarly, a 2013 study of drug courts in New York concluded: “Drug court practices in some jurisdictions are a barrier to access to MMT [methadone maintenance treatment] and may constitute discrimination against people in need of MMT. These practices should be changed, and drug courts should give high priority to ensuring that treatment decisions are made by or in close consultation with qualified health professionals.”63 Aversion to MAT in drug courts was so pronounced that, in early 2015, the U.S. federal government issued new guidance to deny funding for drug courts who forced participants already on methadone or other substitution therapy to phase out medication as a condition for dismissal from drug courts.64 The new grant rules also allowed, but did not require, drug courts funded by federal grants to use up to 20 percent of these grants on MAT.65 Similarly, in September 2015, the governor of New York signed a law to create uniform access to MAT in the state’s judicial diversion program.66 The law amended New York’s Criminal Procedure Law to explicitly state that participation in “medically prescribed drug treatments” cannot be the basis for finding that a participant in a drug court has violated release conditions.67 Even so, many drug court judges remained skeptical of the need for and usefulness of MAT. In February 2017, for example, Yavapai County drug court in Arizona continued to implement a blanket denial of MAT, including to drug court participants who had failed non-medication-assisted treatment before, and where medication had been indicated as necessary for relapse prevention by trained medical professionals.68 Physicians for Human Rights phr.org 12 Research Findings continued Danielle Gravina, MAT Case Manager from Treatment Alternatives for Safe Communities in Queens, a not-for-profit organization contracted by some drug courts in New York City to manage intake, evaluations, and drug testing, told PHR that in the courts she worked with “you are not allowed to be on prescribed medicine to start the [drug court] program, you have to start clean.”69 This applied to both opioid substitution therapy as well as medication prescribed for anxiety, attention deficit disorder, and other co-occurring conditions. It is worth noting that rapid detoxification without medical supervision can have grave, even fatal, consequences.70 In some instances, advocacy for evidence-based treatment and practice came from the drug court staff themselves. In Miami, Florida, treatment providers told PHR the drug court judge, Jeri B. Cohen, forced them to update their treatment methods to include evidence-based options such as MAT.71 This advocacy from drug court judges was not the norm, however. Joanna Caldwell, the risk and compliance manager at South Florida Behavioral Health Network (SFBHN), ran SFBHN’s quality assurance arm, which took complaints filed by third parties against treatment providers. “Judge Cohen is our primary complainant.... I’m not sure if I’d have a job if she wasn’t around,” she said.72 Over the years, organizations like the NADCP and Center for Court Innovation have increased trainings for drug court staff, leading to increasing awareness of evidence-based practice for treating people with substance use disorders, in particular opioid use disorders. However, access to training was still contingent on funding, and for drug courts without funding or dependent on county funding, training and educational seminars on the latest developments in addiction medicine and evidence-based practice were out of reach. Dr. Thomas Robinson, a psychologist and director of mental health at Jackson Hospital in Miami, Florida, pointed to the lack of consistency and scientific grounding in training to treat people with substance use and mental health disorders. “Everyone has a modicum of training, but no one stays up-to-date on new research. You obviously can’t have a psychologist or psychiatrist treating everyone, but you can give more people better training,” he said.73 Inadequate Insurance Reimbursements Treatment providers and drug court team members often cited insurance coverage as an operational consideration in their determination of what type of treatment should be mandated for each drug court participant. While international human rights law does not mandate any specific health system set-up, the right to nondiscrimination in accessing available health care option would require equitable access for all, including people in conflict with the law or those without resources. For many drug court participants, the tension between a criminal justice imperative and their lack of insurance coverage resulted in an additional debt burden or inability to access needed care. Keith Brown, the director of the Law Enforcement Assisted Diversion (LEAD) program in Albany, New York, summarized it succinctly: “The criminal justice [system] tells you: we’ve assessed you and we say you need this care. The insurance company says, that’s fine, but we don’t pay for it.”74 The uncertainty with regard to where payment for treatment would come from created limited options for both drug court teams and treatment providers, who told PHR they at times were compelled to recommend inappropriate treatment plans for participants whose insurance would not cover the option indicated by best practice. Notably, many insurance providers covered only 28 days of inpatient or residential treatment, or less.75 This length of treatment is thought to have its basis in the “Minnesota Model” developed for treating alcoholics in the 1950s,76 but which hasn’t been validated thoroughly since. Dr. Joshua Lee, associate professor of population health and medicine at New York University, told PHR: “There is not a whole lot of evidence that residential treatment for drug dependence needs to be of a particular length.” Dr. Lee also noted that, in his experience as attending physician at Bellevue hospital in New York City, insurance companies regularly refused to pay for the length or type of treatment recommended by the attending physician: “It happens all the time: they deny inpatient treatment, so then we have to send people elsewhere.”77 In PHR’s research, lack of consistency within the treatment community led to the criminal justice system overriding or undermining the credibility of competent treatment providers. It also provided openings for staff without clinical training to implement punitive practices without therapeutic purpose. Medicaid coverage for substance use disorder treatment was considered preferable to private insurance by the treatment providers interviewed by PHR, in large part because the coverage was predictable, and the process to ensure payment likewise known. Drug court coordinators, case managers, and defense lawyers, in particular from New York and New Hampshire, told PHR that one of the very first steps in the drug court intake process was to ensure that the participant was signed up for Medicaid, or had private insurance. An assistant district attorney Neither Justice Nor Treatment Physicians for Human Rights phr.org 13 Research Findings continued in New York County who was an early participant in Manhattan’s first felony drug court told PHR: “A real problem is, ironically, the more affluent defendants. Medicaid pays for everything. But private insurance doesn’t. They won’t reimburse for medicationbased treatment, or have limits to number of visits.”78 Dr. Lee concurred: “Medicaid is easier than commercial insurance.”79 The ACA facilitated the expansion of Medicaid, which extended health insurance benefits to an estimated 1.6 million previously uninsured people with substance use disorders, in states that opted in.80 The ACA also required states that adopted the Medicaid expansion to cover substance use disorder treatment as part of essential health benefits.81 However, outside of essential health benefits, addiction treatment services are not mandated at the federal level, leaving states significant flexibility in how they provide coverage for addiction-related treatment services.82 Research published in 2015 with data from 2011-2013 showed that only 13 state Medicaid programs included all medications approved for alcohol and opioid dependence on their preferred drug lists, with the most commonly excluded drug being methadone. Several state programs required pre-authorization for combined buprenorphine-naloxone treatment and a handful placed lifetime treatment limits of one to three years for MAT.83 Medical research confirms that some people with opioid dependence need to continue on MAT for an extended period of time, even over a lifetime, to avoid relapse and an escalated risk of overdose.84 Further, in states that did not opt for Medicaid expansion through the ACA, such as Florida, a significant proportion of adult drug court participants had incomes that were too low to qualify for subsidies available on the federal exchange, yet they continued to be ineligible for Medicaid and had no employer health insurance.85 For the states covered by this research, New York was the only one that covers all four treatment levels mentioned in ASAM guidelines in its expanded state Medicaid coverage. New Hampshire’s state Medicaid expansion did not cover intensive outpatient and residential outpatient services, and Florida did not opt into Medicaid expansion. All three states, in theory, covered access to methadone, buprenorphine, and naltrexone through Medicaid, though needs assessments and the experience of clinical staff trying to get patients into methadone programs showed considerable unmet needs.86 Neither Justice Nor Treatment Ed Fox, the director of Project SafePoint in Albany, a harm reduction program that did not work directly with drug courts, spoke to the daunting nature of dealing with insurance: “The realities around insurance are complex [for people with substance use disorders]: finding out what insurance they have, calling around, what programs are around that will take their insurance, that can keep people away.… We are holding a person’s hand if necessary – it’s daunting. It’s traumatic enough to be addicted.”87 Barriers Specific to High-Risk, High-Need Participants The NADCP noted in its Best Practice Standards that drug courts should target high-risk and high-need participants, or, if unable to do so, develop alternative tracks with services that meet the risk and need levels of its participants.88 In this context, “high-need” means individuals with a significant need for treatment for a substance use disorder, and “high-risk” means individuals who are very likely to reoffend. In reality, however, this very population faces significant barriers to participation in drug courts, some of which PHR documented during the course of this research. A key barrier to participation in drug court programs for highneed, high-risk people was the very process by which eligibility was determined. While every drug court visited by PHR had a slightly different process, most gave the prosecutor or county attorney the power to decide whether or not a person was offered the option to plead into the court program rather than face criminal charges, and the judge had the final power to veto. David Betancourt, a public defender in Strafford County in New Hampshire, told PHR: “A fifth of people who want drug court are kept out of it, because … the county attorney won’t let them in. That’s the most frustrating, when you have a client who needs drug court and the prosecutor is set on a more punitive sentence.”89 On the other hand, a prosecutor from New York County said that, in her opinion, judges could go in either direction: “Some judges focus very carefully on who really should go into the diversion programs, but some judges will send anyone in.”90 Alex Parsons, the managing defense attorney for Cheshire County in New Hampshire, told PHR: “We had a case in my office where there was a sheriff’s deputy who made a case for this individual that he believed … was in a place where he was ready for treatment and rehab, and this individual was desperate. The prosecutor was of the mindset that he needed to be punished, and that he needed a prison sentence … and the participant became suicidal.”91 Physicians for Human Rights phr.org 14 Research Findings continued Federal and state grants, and, in the case of Florida, a state statute, often exclude specific types of charges from diversion into drug courts. Those charged with offenses considered violent, and repeat felony offenders, are excluded by federal grants, and by the Florida state statute. Some jurisdictions at the county level will impose their own exclusion criteria, such as people charged with the sale of drugs rather than simple possession. A person who is both high-need and high-risk will likely hit one or several of those exclusion factors: they will have been arrested multiple times, they will sell drugs to fund their use, and they may have displayed violent behavior as a result of their addiction. In some places, available treatment centers would not take court-mandated clients charged with violence offenses. Dana Patterson, the case manager from Alachua County felony drug court in Florida, told PHR the restrictions of the closest residential rehabilitation center proved difficult for the intake process, because some patients whose drug dependency level was such that inpatient care would be deemed more likely to be successful would not be considered eligible for residential treatment because of the nature of their alleged crime. “If we were to start taking violent offenders, there would be an issue internally in terms of care, because their criminal history might make them ineligible for [inpatient treatment], which means that we are setting them up for failure by taking them into the program at an outpatient level,”92 Patterson said. A key criticism launched at drug courts has been that they cherrypick their participants.93 It may very well be that they do not cherry-pick so much as have their participants picked for them through these funding restrictions, which skew participants towards lower need and lower risk. A New York prosecutor told PHR that it was a waste of resources to send people to drug court who do not really have a serious drug problem, as there are a lot of people who could benefit, and there is a waiting list for treatment in New York City unless you are mandated by a court.94 Chief Justice Tina Nadeau, of the New Hampshire Supreme Court, told PHR the acceptance of low-need individuals in drug courts meant recidivism rates for the courts should not be read as a measure of effectiveness, but rather as a proxy measure for whether participants had needed treatment in the first place: “If you have really low recidivism rates [in drug court participants] then it’s not really a good measure for how well you’re doing because you’re not taking the people who need it most.”95 She said this element was hard to communicate to legislators who determine funding, because they look to recidivism rates rather than long-term recovery as proof the drug court model works. Neither Justice Nor Treatment Broken Promises: Involuntary and Punitive Treatment in Drug Courts Drug courts promise voluntary treatment, not punishment, for people with substance use disorders, including appropriate support for recovery. In PHR’s research, much of this promise remains unfulfilled. Many treatment providers felt their expertise was overridden by other drug court team members, like the prosecutor, probation officer, or judge, who preferred to impose punishment for behavioral or treatment infractions such as breaking a curfew or failing to comply with other drug court rules. Several providers told PHR that they often had to defend their therapeutic choices in court, and that they decided on a case-bycase basis whether it was worth the fight.96 Many interviewees pointed out the tension between the courts’ mandate to balance public safety with the needs of drug court participants, which in some cases led to drug courts weakening due process. Particularly in New Hampshire, where more courts were admitting higher-risk cases, including people charged with violence offenses, prosecutors and probation officers cited the need to keep participants under close surveillance, a practice that undermined the therapeutic approach. “A fifth of people who want drug court are kept out of it, because … the county attorney won’t let them in. That’s the most frustrating, when you have a client who needs drug court and the prosecutor is set on a more punitive sentence.” David Betancourt, public defender, Strafford County, New Hampshire Physicians for Human Rights phr.org 15 Research Findings continued Drug Tests, Abstinence, and Patient-Provider Confidentiality Most drug courts PHR visited compelled participants to waive doctor-patient confidentiality and to submit to regular drug tests which – it was understood – would be discussed openly in court. This element is, in fact, key to most drug courts across the United States: a participant’s abstinence from all drug use other than (in some cases only) MAT – often measured in terms of drug test results – was a condition for their graduation to the next level of the program. The NADCP Best Practice Standards, published in 2015, state that a person suffering a relapse or testing positive for drug use should never be punished, but should instead receive a “therapeutic adjustment.”97 However, PHR found that testing positive for drug use still resulted in punishment in many drug courts. Several courts in Florida imposed jail sentences of up to a month for positive or missed drug screenings.98 In Putnam County, New Hampshire, the first positive drug screen automatically leads to seven days in the county jail, with any subsequent positive drug screen leading to a minimum of 48 hours in jail.99 Judge James Carroll, of the Belknap County drug court in New Hampshire, summarized this situation aptly: “If it’s a cancer patient, we bake brownies and throw fundraisers for them. We need to have more of that mentality for those with addiction.”100 Lack of confidentiality at times led to a breakdown of the therapeutic relationship between health care provider and patient. Stacey Lanza, a treatment provider who worked with court-mandated patients at Phoenix House in New Hampshire for two years, noted: “It was very difficult to do true treatment and therapy with [drug court] clients because there was this sense that we were going to tell the team and judge, and they would be punished.”101 Likewise, Asa Scott, an addiction care administrator at Addiction Care Interventions in New York, expressed discomfort with the role of being a court “snitch” and worried that patients might not see clinicians as advocates because the “stick of the punishment from court is greater than the carrot of therapy.”102 She reported that one patient told her “I have three hands around my neck” – meaning, the court, the therapist, and his own. Neither Justice Nor Treatment Abstinence measured through drug tests was often used as a proxy for court compliance, even to the exclusion of other measures. In one drug court session in New York City observed by two PHR researchers in June 2016, a participant who had tested negative for drug use graduated to the next phase of the program despite having used abusive language against a treatment provider, while another who had tested positive was held back despite reportedly engaging constructively in the court-mandated treatment program. Moreover, both drug court participants had their drug use and treatment information discussed in open court.103 The National Association of Drug Court Professionals highlights the need for both abstinence and regular drug tests as a key component of the model they promote.104 Some addiction specialists told PHR that drug testing may have a therapeutic purpose in addiction therapy, though PHR was not able to find research to support this claim. Treatment providers linked this therapeutic purpose to the establishment of trust between patient and therapist. Notably, this trust would be undermined by punishing positive drug tests with jail time or delay in graduation from the drug court program. David Lucas, treatment coordinator at Toronto drug court, said he had asked his clients about the usefulness of drug tests: “They said it made things simple for them: I can’t lie about it, so I’ll just have to be honest. Maybe they can’t be honest yet about abuse or trauma, but they have to be honest about the drug use.”105 Lucas added, however, that no participant gets punished for a positive drug screen at Toronto drug court: “We don’t give them any static about use – if we did that, we’d be little more than glorified parole officers.”106 To be sure, carrying out targeted exams and tests to measure the impact of any kind of treatment is part of the responsible practice of medicine. In fact, drug dependence and substance use disorders are health conditions, the normal patterns of which include relapses of drug use,107 which can be measured in toxicology reports. Further, in the context of MAT, toxicology reports for use in private medical consultations are necessary to check and adjust dosage levels and cross-refer with other patient indicators. However, when this information is shared in public court hearings or used to administer punishment, the individual’s human rights to privacy and health are violated. Physicians for Human Rights phr.org 16 Research Findings continued Inadequate Case Management Drug courts in the United States provide varying levels of support for participants in terms of facilitating access to housing, transport, education, and health care unrelated to problem drug use. This type of support – often referred to as “case management” – has proven paramount to participants successfully completing drug court programs. In an evaluation of New York drug courts published in 2011, higher levels of case management, in combination with a judge’s consistent praise and engagement, was highlighted as key to lowering the incidence of drug use and criminal behavior in participants.108 In fact, many of the treatment providers, lawyers, and judges PHR spoke with noted that case management not only was key to a person’s ability to graduate from drug court, but also to long-term recovery. Treatment providers and coordinators, in particular, often placed it above judicial supervision, and certainly above sanctions. The mental health counselor at a residential treatment center in upstate New York, which accommodates courtmandated patients from across the state, told PHR that a stronger focus on the patients’ needs and motivation, rather than on abstinence, would support successful treatment outcomes and long-term recovery: “Maybe if [drug courts] focused less on scare tactics, if they were more supportive… if they were to examine more closely a client’s own motivation: do they want to get clean, to not reoffend, or to take care of their family, and then go with that… we’d be more successful.”109 PHR’s interviewees mentioned lack of housing in particular as a serious issue that could determine whether or not a participant was able to successfully complete a court-mandated treatment plan. Robert Gasser, a retired prosecutor and former coordinator of Grafton county drug court in New Hampshire, told PHR that housing turned out to be central to success, as many drug court participants are homeless, in nonpermanent housing, or need to leave their home situation to get away from family members who use drugs: “When I started the drug court in Grafton, people told me I’d have two problems. One was transport: people can’t get to court, can’t get to treatment, can’t meet their obligations. This was not a problem. People bonded together, they would get a van, or help each other get to where they needed to get to. The second problem was housing. And, boy, that is absolutely our number one problem.”110 Other counties in New Hampshire cited similar problems, and noted that transportation could be of critical concern because it affected a person’s ability to make court and clinic appointments.111 Most drug courts PHR visited did not have the funding or regulatory support to offer case management services like transportation and housing. “It’s predictable that [the Neither Justice Nor Treatment participants] won’t succeed if they don’t have these things,” said Alex Casale, state drug court coordinator in New Hampshire. “We have an obligation to provide what our participants need. They need housing, they need various levels of treatment for their substance abuse and mental health problems – which run the gamut – and they need counseling and education [referring to the fact that some drug court participants did not finish schooling].”112 Many participants and drug court team members we spoke with were not able to speak with personal experience to the difference such services would have made, given that the services were not available to them. Instead, the main experiential knowledge came from harm reduction activists, who witnessed the impact firsthand in terms of a reduction in criminal recidivism. Keith Brown, the director of Albany’s LEAD program, a pre-arrest diversion program that is based on harm reduction principles, told PHR that LEAD was all case management with no punitive sanctions. Because of it, LEAD was successful at keeping people out of the criminal justice system: “For example, if you are a homeless injector, and you keep getting arrested because you inject in a MacDonald’s – even if we can’t get you treatment, if we get you an apartment, that’s going to lower your engagement with criminal justice, because you now have a safe place to use. Is it the be-all end-all? Of course not. But does it keep you out of the criminal justice system? Yes, it does.”113 For contrast, PHR also reached out to David Lucas, the treatment coordinator at Toronto drug court, in Canada, where support services were readily available. He confirmed: “If you asked the clients, ‘How do you measure success and how do you get [to recovery]?,’ not a single one would mention urine screens. They would talk about community, connection, housing, support – that’s what really works and what brings the lasting change.”114 “Maybe if [drug courts] focused less on scare tactics, if they were more supportive… if they were to examine more closely a client’s own motivation - do they want to get clean, to not reoffend, or to take care of their family, and then go with that… we’d be more successful.” Mental health counselor, residential treatment center, New York Physicians for Human Rights phr.org 17 Research Findings continued Involuntary Treatment Drug court participants signed over their rights to autonomy and confidentiality in treatment when entering court-supervised programs. The justification given for this limitation on rights was usually that no one is forced to participate – that participants voluntarily choose treatment over jail or probation. Critics of drug courts have noted that the voluntary nature of court-mandated treatment has been compromised by limited alternatives, and by the severity of the prison sentence the participant would otherwise serve.115 Apart from the potential prison sentence and probation, there are also long-term legal consequences to being convicted for a drugrelated offense, which might compel a person to plead into drug court regardless of whether they are ready for or in need of the treatment program provided through the court. Federal and state regulations permit (in some cases require) the exclusion of those convicted of drug-related offenses from public benefits. For example, the Welfare Reform Act of 1996 makes anyone with a federal or state felony drug conviction ineligible for welfare benefits for life.116 Conviction for drug-related offenses also leads to a time-bound ban on federal student aid, and people with three convictions are subject to a life-long ban.117 Federal and state housing regulations allow substantial discretion on exclusion of people who use drugs from public housing – no conviction or arrest necessary.118 Most states – with the notable exception of Vermont and Maine – impose some restrictions on voting rights for convicted or imprisoned felons, including those convicted of drug-related offenses.119 Florida imposes a lifetime voting ban on all people convicted of a felony. Fourteen states, including Florida and New York, automatically suspend drivers’ licenses for at least six months for drug possession. Florida requires a mandatory suspension of one year.120 In fact, many of the drug court team members PHR interviewed noted that drug court programs and plans only really work where the threat of a prison sentence or other traditional criminal justice responses is strong enough.121 Some testified that some drug court participants were charged with the maximum amount of crimes in order to create a “big enough stick,” meaning an incentive for them to “volunteer” for drug court.122 Ironically, drug court participants often had to plead guilty to these unproven charges in order to access drug court and would receive conventional criminal justice sentencing for those charges if they failed to graduate from drug court. Neither Justice Nor Treatment In Florida, people with substance use disorders did not have to be charged with a crime to be subjected to involuntary treatment. The Substance Abuse Impairment Act (known as the Hal S. Marchman Alcohol and Other Drug Services Act or Marchman Act) allows for the involuntary commitment and treatment of people “if there is good faith reason to believe that the person is substance abuse impaired or has a co-occurring mental health disorder.”123 The admission criteria was loosely established through the law as a situation where someone who uses drugs “without care or treatment is likely to suffer from neglect or refuse to care for himself or herself; that such neglect or refusal poses a real and present threat of substantial harm to his or her well-being; and that it is not apparent that such harm may be avoided through the help of willing family members or friends or the provision of other services, or there is substantial likelihood that the person has inflicted, or threatened to or attempted to inflict, or, unless admitted, is likely to inflict, physical harm on himself, herself, or another.”124 In other words, a person could be involuntarily committed – by reference to harm or criminal behavior that hasn’t happened yet – on the basis of the subjective judgement of drug court staff and facilitating agencies without medical or substance abuse treatment training. While Marchman Act admissions in principle were separate from criminal procedures, warrants issued under that law were implemented with the full coercive force of the police, with severe consequences. Brian, a 32-year-old man in Tampa, told PHR: “It really doesn’t help when they pick you up for those [Marchman Act] warrants, they come with three or four cop cars, picking you up in the middle of the night, freaking out my family. I have three little girls. And then there is the constant going over to my neighbor’s house and stating that I’m not a fugitive … that I’m not a criminal, even though I am being treated like one. That [my case] is a mental health case.”125 Brian estimated he had spent more than 145 days in custody for refusing to comply with treatment or test orders, and waiting for a bed in residential treatment. He faced no criminal charges at all. Some treatment providers interviewed in all three states said court-enforced compliance with treatment requirements made their jobs easier. They pointed to better compliance with treatment for participants under court supervision. “It doesn’t matter how you get into treatment, whether it’s mandatory or voluntary. I think consequences are part of the recovery process. If you had that same approach in the public health department, you’d get a lot more people doing well,” said Debra Thomas, a clinical liaison with DACCO, a treatment provider receiving courtmandated clients from the Hillsborough Drug Court in Tampa, FL.126 Physicians for Human Rights phr.org 18 Research Findings continued Régent Champigny, a mental health counselor with the Greater Nashua Mental Health Center in Nashua, New Hampshire, agreed. Mr. Champigny was contracted by the Nashua drug court to treat its clients. “They are a unique bunch coming from the criminal justice system. It’s the nudge from the judge that is very effective. If my clients were not in drug court, they wouldn’t meet their appointments and better themselves,” he said.127 From a medical perspective, there is little evidence to support enhanced effectiveness of involuntary treatment for substance use disorders. A systematic analysis of the scientific evidence on the effectiveness of compulsory drug treatment published in 2016 concluded that the limited literature on this subject did not, on the whole, suggest improved outcomes from compulsory treatment, with some studies suggesting potential harms.128 From a human rights perspective, as well, the voluntary nature of the treatment is paramount, as the rights to health and physical autonomy require informed and meaningful consent to treatment.129 Moreover, even treatment providers who referred to mandated treatment as “overall a good thing” clarified that a person’s motivation to enter treatment was what determined a successful treatment outcome. Dr. Todd Patton, medical director at El Rio treatment center in the Bronx, New York City, told PHR: “For people who are really ready for [treatment], [mandated care] can be a life changer, and we’ve had people really turn their lives around. … But there are some people who are not ready, and you have to want to get better [for treatment to work].”130 A woman stands in the hallway of a drug treatment clinic in Burlington, Vermont. Photo: Jordan Silverman/Getty Images Even treatment providers who referred to mandated treatment as “overall a good thing” clarified that a person’s motivation to enter treatment was what determined a successful treatment outcome. Neither Justice Nor Treatment Physicians for Human Rights phr.org 19 Human Rights, Health Care, and Criminal Justice Confidentiality Consent to Treatment The right to privacy is protected under international law, including in the International Covenant on Civil and Political Rights (ICCPR).131 The UN Human Rights Committee, which is authorized by states to monitor the implementation of the ICCPR and offer authoritative interpretations of its provisions, has noted that any state interference with the right to privacy, “even interference provided for by law [,] should be in accordance with the provisions, aims and objectives of the Covenant and should be, in any event, reasonable in the particular circumstances.”132 The right to bodily integrity, and with it the right to refuse medical treatment and to be free from non-consensual treatment, is an integral part of the human rights to health,140 security of person,141 and to freedom from torture and other cruel, inhuman, and degrading treatment.142 The Declaration of Lisbon establishes a patient right to self-determination, including the right “to make free decisions regarding himself/herself,” “the right to give or withhold consent to any diagnostic procedure or therapy,” and “the right to the information necessary to make his/her decisions.”143 The right to confidentiality in health care is implicit in the right to the highest attainable standard of health, contained in the International Covenant on Economic, Social and Cultural Rights (ICESCR).133 The Committee on Economic, Social and Cultural Rights, the authoritative oversight body for the ICESCR, refers specifically to the “right to have personal health data treated with confidentiality.”134 The World Medical Association’s Declaration of Lisbon on the Rights of the Patient (Declaration of Lisbon) establishes a right to confidentiality, noting that “all identifiable information about a patient’s health status, medical condition, diagnosis, prognosis and treatment and all other information of a personal kind must be kept confidential, even after death.”135 All 50 U.S. states have legislation that requires some level of informed consent for treatment.144 The doctrine of informed consent also includes the right to refuse medical treatment, and is clear that patients must be given the information to understand the health consequences of both treatment and refusal of treatment.145 These elements are routinely flouted in drug courts, where treatment elements and options often are part of an incentives and sanctions schedule, and where consent is compelled through threats of incarceration. In an effort to encourage people to seek treatment, U.S. federal law specifically protects the confidentiality of drug and alcohol abuse treatment and prevention records.136 The regulations are meant to limit the use and disclosure of substance abuse patient records and identifying information in federally assisted substance abuse treatment programs.137 The protections are broad, but the exceptions to them equally so. Notably, in the case of drug court proceedings, while treatment providers usually are covered by federal confidentiality regulations, the other members of the drug court team are exempt and often refer to treatment information in open court.138 Moreover, the law sets out exceptions to the consent requirement, including when disclosure is in response to a court order, and when patients provide written consent to disclosure.139 All of the drug courts Physicians for Human Rights (PHR) visited required participants to waive the right to confidentiality of their treatment information as a condition for participation in the drug court program. Dual Loyalty The primary loyalty of every health care professional must be to their patient. This concept is central to medical ethics, and is captured in the very first principle of the Declaration of Lisbon: “Every patient has the right to be cared for by a physician whom he/she knows to be free to make clinical and ethical judgements without any outside interference.”146 Dual loyalty occurs when a doctor’s primary concern for their patient is replaced, in part or in whole, by “simultaneous obligations, express or implied … to a third party, often the state.”147 Where the interests of the patient and the state are the same, dual loyalty poses little risk. However, where they are not aligned, the result could be that doctors are compelled to set aside the interests of their patients for the benefit of the state. The International Dual Loyalty Working Group, convened by PHR in 1993, provided examples of contexts that may give rise to dual loyalty conflicts, including health practice in closed institutions such as prisons and with socially stigmatized patients.148 The Working Group also gave concrete examples of the dimensions of the problem: –– Health professionals subordinating independent judgment, whether in therapeutic or evaluative settings, to support conclusions favoring the state or other third party; and –– Health providers limiting or denying medical treatment or information related to treatment of an individual to effectuate the policy or practice of the state or other third party.149 These elements are certainly borne out in the context of some drug courts in the United States, as documented in this report. Neither Justice Nor Treatment Physicians for Human Rights phr.org 20 Conclusion and Recommendations While some drug courts have benefitted people who would otherwise not have gotten treatment, other drug courts have fallen woefully short of achieving the objectives set almost three decades ago to substitute treatment for jail for people suffering from substance use disorders. This is largely due to a conflation of substance use with addiction, a serious unmet treatment need, and a reluctance to trust the growing evidence base on what constitutes quality treatment and what are appropriate clinical guidelines for care. The drug courts we examined varied widely in whether they were able to provide participants with access to quality evidence-based treatment, their acceptance of medication-assisted treatment, and their attitudes towards diversion of people who engaged in criminal behavior due to problematic drug use away from the criminal justice system altogether. It is questionable if drug courts will ever be able to deliver on their promise, rooted as they are in a punitive criminal justice logic that undermines their stated objective to treat participants as ill rather than deviant. By implementing the following recommendations, the courts may, however, bridge some of the gap. To the White House • Ensure that the White House Office of National Drug Control Policy (NADCP), or equivalent entity, provides adequate grants for state and local initiatives to address problem drug use through comprehensive, community-based strategies involving appropriate case management, access to stable housing, and evidence-based treatment, in particular those provided for in Public Law 114–198, section 103. To the Department of Justice • Provide increased funding for state and local pre-booking diversion initiatives (Law Enforcement Assisted Diversion programs). These initiatives have been shown to dramatically decrease recidivism and avoid re-arrest of people with addiction-related criminal behavior. • Remove restrictions attached to current Bureau of Justice Assistance and Substance Abuse and Mental Health Services Administration grants (and any other federal grants for drug courts) requiring that only non-violent offenders be diverted to treatment courts, thereby allowing courts to take ‘highrisk, high-need’ people based on medical best practice and diagnosis, not legal criteria. • Issue federal guidelines for drug court regulations, based on NADCP best practices, including, at a minimum, the following guarantees: –– Access to evidence-based treatment for substance use disorders, including access to medication-assisted treatment (MAT) where appropriate according to clinical best practices; –– No punitive actions taken for positive drug tests or other symptoms of substance use disorders; Neither Justice Nor Treatment –– Assessment for substance use disorder based on American Society of Addiction Medicine or other evidence-based criteria; –– A certified MAT provider as well as a trained health professional on all drug court teams; –– Sufficient funding to ensure case management support in all drug courts, including, specifically, facilitating access to housing and public transport; –– Continued legal representation for all drug court participants throughout drug court proceedings; and –– Public funding for all court-mandated treatment and tests. To Congress • Decriminalize drug possession for personal use as a direct way to facilitate access to voluntary treatment by removing fear of arrest. • Ensure Medicaid coverage for people with substance use disorders living below the poverty line. • Appropriate adequate funding for grant initiatives and programs announced in Public Law 114-198, as well as other initiatives geared at diverting people charged with addictionfueled criminal behavior away from the criminal justice system. • Remove restrictions on public benefits for people convicted of drug-related offenses, including restrictions on federal student aid. To State Governments • Issue state guidelines for drug court regulations, based on NADCP best practices and follow any federal guidelines based on best practices, as recommended for federal guidelines above. • Ensure that state Medicaid covers treatment for substance use disorders according to best clinical practices and guidelines. • Immediately defund drug courts that disallow MAT. • Decriminalize drug possession for personal use as a direct way to facilitate access to voluntary treatment by removing fear of arrest. To County Commissioners • Immediately defund drug courts or treatment providers receiving court-mandated clients that disallow MAT. • Require drug courts receiving county funding to follow federal and state guidelines on best practices and evidence-based treatment. • Provide additional funding for training and capacity building for drug court staff, including treatment providers in the community receiving funding for drug court referrals. To Health Insurance Companies • Cover evidence-based treatment for substance use disorders, including access to MAT, as prescribed by a patient’s or drug court participant’s treating physician. Physicians for Human Rights phr.org 21 Endnotes 1. Florida Courts, “Drug Courts,” accessed May 8, 2017, http://www.flcourts.org/resources-and-services/courtimprovement/problem-solving-courts/drug-courts/. 2. New York State Unified Court System, “Drug treatment courts,” accessed May 8, 2017, http://www.nycourts. gov/courts/problem_solving/drugcourts/index.shtml. 3. New Hampshire Judicial Branch, “Drug and Mental Health Courts,” accessed May 8, 2017, https://www. courts.state.nh.us/drugcourts/locations.htm. 4. See Human Rights Watch and the American Civil Liberties Union, “Every 25 Seconds: The Human Toll of Criminalizing Drug Use in the United States,” October 2016, accessed on April 11, 2017, https://www.hrw. org/report/2016/10/12/every-25-seconds/human-tollcriminalizing-drug-use-united-states. 5. See David Boyum, Peter Reuter, “An Analytic Assessment of U.S. Drug Control Policy,” American Enterprise Institute Press, Washington, DC, 2005, pp. 2-3; and Beau Kilmer, Gregory Midgette, and Clinton Saloga, “Back in the National Spotlight: An Assessment of Recent Changes in Drug Use and Drug Policies in the United States,” Brookings Institute, July 2016, accessed February 17, 2017, https://www.brookings.edu/wpcontent/uploads/2016/07/Kilmer-United-States-final-2. pdf. 6. See Human Rights Watch and the American Civil Liberties Union, “Every 25 Seconds: The Human Toll of Criminalizing Drug Use in the United States,” October 2016. 7. Ronald Reagan, “Radio Address to the Nation on Federal Drug Policy,” October 2, 1982, accessed March 7, 2017, http://www.presidency.ucsb.edu/ws/?pid=43085; Tess Owen, “’Just Say No’: How Nancy Reagan Helped America Lose the War on Drugs,” Vice, March 6, 2016, accessed March 7, 2017, https://news.vice.com/article/ just-say-no-how-nancy-reagan-helped-america-losethe-war-on-drugs. 8. New York City Police Department, “Broken Windows and Quality of Life Policing in New York City,” William J. Bratton, Police Commissioner, 2015, accessed March 9, 2017, http://www.nyc.gov/html/nypd/downloads/ pdf/analysis_and_planning/qol.pdf; George L. Kelling and James Q. Wilson, “Broken Windows: The police and neighborhood safety,” The Atlantic, March 1982, accessed March 9, https://www.theatlantic.com/ magazine/archive/1982/03/broken-windows/304465/; John Del Signore, “Broken Windows Theory Broken: Most People Arrested for Pot Possession Aren’t Dangerous Criminals,” The Gothamist, November 23, 2012, accessed March 9, 2017, http://gothamist.com/2012/11/23/ broken_windows_theory_broken_most_p.php; Human Rights Watch, “A Red Herring: Marijuana Arrestees Do Not Become Violent Felons,” 2012, accessed March 9, 2017, https://www.hrw.org/report/2012/11/23/ red-herring/marijuana-arrestees-do-not-become-violentfelons. Both the relative dangers of “illicit” versus legal drugs as well as the effectiveness of abstinence as key to avoiding drug addiction have implicitly been validated through “broken windows” policies, without reference to historical fact or evidence. In fact, drugs predominantly used by marginalized populations have often been subject to restrictions, whereas the drugs of choice for more privileged groups have not. See e.g. Tessie Castillo, “Why Are Heroin, Cocaine and Other Drugs Really Illegal? We Must Never Forget the Answers,” The Influence, April 4, 2016, accessed March 7, 2017, http:// theinfluence.org/why-are-heroin-cocaine-and-otherdrugs-really-illegal-we-must-never-forget-the-answers/ (discussing the history of criminalization of drugs in the United States). When restrictions are imposed, the Neither Justice Nor Treatment 9. 10. 11. 12. 13. 14. harm of the restricted drug is often cited as justification. However, a landmark study published in 2007 – focused on the United Kingdom, which has similar drug classifications to the United States – showed virtually no correlation between legal classification of harm and actual harmfulness of any particular drug. Notably, the study showed that the actual physical, mental, and social harms of both marijuana and ecstasy were lesser than those of alcohol and nicotine, even though the former were criminalized and the latter were not. David Nutt et al, “Development of a rational scale to assess the harm of drugs of potential misuse,” The Lancet, Vol. 369, No. 9566, pp 1047-1053 (assessing the potential harm of various legal and illegal drugs of potential misuse, and showing virtually no correlation between legal classification of harm and actual harmfulness of a drug). Scott O. Lilienfeld and Hal Arkowitz, “Why ‘Just Say No’ Doesn’t Work,” Scientific American, January 1, 2014, accessed March 7, 2017, https://news.vice.com/article/ just-say-no-how-nancy-reagan-helped-america-losethe-war-on-drugs. Paul Hayes, “Many people use drugs – but here’s why most don’t become addicts,” The Conversation, January 6, 2015, accessed on March 7, 2017, http:// theconversation.com/many-people-use-drugs-butheres-why-most-dont-become-addicts-35504. See also National Institute on Drug Abuse, “Principles of Drug Addiction Treatment: A Research-Based Guide,” last updated December 2012, accessed March 7, 2017, https://www.drugabuse.gov/publications/principlesdrug-addiction-treatment-research-based-guide-thirdedition/frequently-asked-questions/there-differencebetween-physical-dependence (arguing that there is a difference between drug dependence and addiction, and that some people who use drugs develop one, both, or neither). Arian Campo-Flores and Jeanne Whalen, “Needle Exchanges Gain Currency,” The Wall Street Journal, March 29, 2015, accessed February 17, 2017, https:// www.wsj.com/articles/needle-exchanges-gain-currencyamid-hiv-hepatitis-infections-in-drug-users-1427673026; Drug Policy Alliance, “Law Enforcement Assisted Diversion: Reducing the Role of Law Enforcement in Local Drug Control,” February 2016, accessed February 17, 2017, http://www.drugpolicy.org/sites/default/files/ DPA%20Fact%20sheet_Law%20Enforcement%20 Assisted%20Diversion%20%28LEAD%29%20 _%28Feb.%202016%29.pdf. On December 18, 2015, President Obama signed the 2016 Consolidated Appropriations Act, allowing federal funds to be used for some aspects of syringe exchange programs. See Human Rights Watch and the American Civil Liberties Union, “Every 25 Seconds: The Human Toll of Criminalizing Drug Use in the United States,” October 2016, at footnote 28. See Mark A.R. Kleiman, Legal Commercial Cannabis Sales in Colorado and Washington: What Can We Learn? (Washington D.C.: Brookings Institute, 2015); and John Ingold, “Lawmakers in 11 States Approve Low-THC Medical Marijuana Bills,” Denver Post, June 30, 2014, accessed March 15, 2017, http://www.denverpost.com/ marijuana/. Miami-Dade County Drug Court, accessed February 22, 2017, http://www.miamidrugcourt.com/. Graduated sanctions can include more frequent drug testing, inpatient detoxification and treatment, additional court appearances, and short periods of incarceration that may increase as an offender’s infractions accumulate. To encourage participants’ continued compliance, drug courts also provide incentives, such as fewer drug tests, fewer court appearances, and possibly the dismissal of criminal charges or reduced or set-aside sentences if the program is successfully completed. U.S. DOJ, BJA, OJP, “Defining Drug Courts: The Key Components,” January 1997, reprinted 2004, pp. 14-15; Douglas B. Marlowe, “Integrating Substance Abuse Treatment and Criminal Justice Supervision,” Science and Practice Perspectives, National Institute on Drug Abuse of the National Institutes of Health, August 2003, p. 7; U.S. DOJ, BJA, OJP, “BJA Drug Court Discretionary Grant Program: FY 2010 Requirements Resource Guide,” p. 2; and NCJRS, In the Spotlight: Drug Courts; Douglas B. Marlowe, “Integrating Substance Abuse Treatment and Criminal Justice Supervision,” Science and Practice Perspectives, National Institute on Drug Abuse of the National Institutes of Health, August 2003, p. 7. 15. National Drug Court Resource Center, “How Many Drug Courts Are There?” accessed February 17, 2017, http:// www.ndcrc.org/content/how-many-drug-courts-arethere. 16. National Association of Drug Court Professionals, “Drug Courts Work,” accessed February 17, 2017, http://www. nadcp.org/learn/facts-and-figures. 17. Graduation requirements vary from drug court to drug court. However, a core requirement for most courts examined by PHR was a certain time frame during which all drug tests for the participants are negative, including alcohol testing and tests for prescribed medication. This is not the case in some non U.S. drug courts. 18. See National Association of Drug Court Professionals, “Defining Drug Courts: The Key Components” (Washington, DC: U.S. Department of Justice, 1997), accessed on March 31, 2017, http://www.ndci.org/sites/ default/files/nadcp/KeyComponents.pdf. 19. Lauren Kirchner, “Drug Courts Grow Up,” Pacific Standard Magazine, July 27, 2015, accessed on February 17, 2017, https://psmag.com/drug-courts-grow-up276ed4bbd5f8#.8mv8crs3z, emphasis in original. 20. NADCP, “Research Update on Adult Drug Courts,” Marlowe, Douglas B. JD, PhD, December 2010, accessed on April 11, 2017, http://www.nadcp.org/sites/default/ files/nadcp/Research%20Update%20on%20Adult%20 Drug%20Courts%20-%20NADCP_1.pdf. 21. Shelli B. Rossman, Michael Rempel, John K. Roman et al., “The Multi-Site Adult Drug Court Evaluation: Study Overview and Design. Final Report: Volume 4” (Washington: The Urban Institute, 2011), accessed March 31, 2017, http://www.urban.org/uploadedpdf/412354MADCE-Study-Overview-and-Design.pdf. 22. See Ciska Wittouck et al, “The Impact of Drug Treatment Courts on Recovery: A Systematic Review,” The Scientific World Journal, Volume 2013, accessed March 31, 2017, https://www.hindawi.com/journals/tswj/2013/493679/. 23. According to a report released by the United Nations Office on Drugs and Crime, heroin use in the United States increased by 145 percent between 2007 and end 2015. The U.S. Centers for Disease Control and Prevention estimates that the number of overdose deaths including opioids quadrupled from 1999 to 2015. See Susan Scutti, “Worldwide drug use steady, but heroin on rise in U.S., U.N. report says,” CNN, June 23, 2016, accessed March 9, 2017, http://www.cnn. com/2016/06/23/health/un-world-drug-report/; Centers for Disease Control and Prevention, “Understanding the Epidemic, Drug overdose deaths in the United States continue to increase in 2015,” last updated December 16, 2016, accessed <arcj 15, 2017, https://www.cdc.gov/ drugoverdose/epidemic/. 24. Comprehensive Addiction and Recovery Act of 2016, P.L. 114-198, July 22, 2016. Physicians for Human Rights phr.org 22 Endnotes continued 25. Naloxone is an opioid antagonist used to counter the effects of opioid overdose. “Understanding Naloxone,” Harm Reduction Coalition, accessed March 15, 2017, http://harmreduction.org/issues/overdose-prevention/ overview/overdose-basics/understanding-naloxone/. 26. P.L. 114-198, Sec. 201. 27. P.L. 114-198, Sec. 103. 28. Sharon LaFraniere and Alan Rappeport, “Popular Domestic Programs Face Ax Under First Trump Budget,” New York Times, February 17, 2017, accessed March 15, 2017, https://www.nytimes.com/2017/02/17/us/politics/ trump-program-eliminations-white-house-budget-office. html. 29. For example, in 2016, New Hampshire’s governor, Maggie Hassan (now a U.S. Senator), signed legislation establishing a statewide drug court program as part of the state’s efforts to expand treatment and recovery programs and address criminal recidivism related to the opioid crisis. Maggie Hassan, “Combatting the Heroin and Opioid Crisis: Federal Support for Those on the Front Lines,” 2016, p. 12, accessed on March 15, 2017, http://maggiehassan.com/wp-content/uploads/2016/09/ CombatingtheHeroinandOpioidCrisis.pdf. 30. Addiction Policy Forum, “Innovation Enforcement Assisted Diversion (LEAD),” February 2017, accessed March 15, 2017, http://media.wix.com/ugd/ bfe1ed_561f2ede90fe4c8f8250972ac015550a.pdf. 31. Shafaq Hasan, “Boston Considers Adopting Gloucester’s “Angel” Program for Drug Offenders,” Nonprofit Quarterly, June 17, 2015, accessed March 15, 2017, https://nonprofitquarterly.org/2015/06/17/bostonconsiders-adopting-gloucesters-angel-program-fordrug-offenders/. 32. PHR interview with Melissa Guldrandsen, county attorney in Belknap County, New Hampshire in December, 2016: “I look for people who have mediumrange criminal records, with more drug and property cases, we don’t have a hard rule that we don’t take violent offenders, but I don’t want a hard and fast bad guy in the group. It’s probably rather intuitive, I look at the criminal history and their crimes and circumstances. If someone is entrenched in criminal thinking over time, I don’t want their victim of a new crime coming back to me to say to me ‘why are you putting this person into this program?’” “High-risk, high-need” participants have been designated by the NADCP Adult Drug Court Best Practice Standards manual as individuals who are both diagnosed with an addiction disorder and at high risk for criminal recidivism. In New Hampshire, several counties have interpreted “high-risk” to also include people charged with violent offenses. 33. Eric J. Miller, “Embracing Addiction: Drug Courts and the False Promise of Judicial Interventionism,” Ohio State Law Journal Vol. 65, 2004 pp. 1479-1576. 34. See American Society of Addiction Medicine, “Definition of Addiction,” accessed May 9, 2017, http://www.asam. org/quality-practice/definition-of-addiction. 35. Addiction has been defined as a chronic brain disease by the American Society of Addiction Medicine, as well as by the National Institute on Drug Abuse (NIDA) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA): “Addiction is a chronic, often relapsing brain disease … similar to other chronic, relapsing diseases, such as diabetes, asthma, or heart disease….” See National Institute on Drug Abuse, “Understanding Drug Use and Addiction,” updated August 2016, accessed February 22, 2017, https://www. drugabuse.gov/publications/drugfacts/understandingdrug-use-addiction. See also McLellan AT, Lewis DC, O’Brien CP, Kieber HD. Drug dependence, a chronic Neither Justice Nor Treatment medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284 (13), pp. 1689–1695. There has been considerable debate among health care providers and medical researchers about the usefulness of the “chronic disease concept” to explain substance dependence or compulsive behavior of any kind. For conflicting views see, e.g., Maia Szalavitz, “Why the New Definition of Addiction, as ‘Brain Disease,’ Falls Short,” TIME Magazine, August 16, 2011, accessed February 22, 2017, http://healthland.time.com/2011/08/16/ why-the-new-definition-of-addiction-as-brain-diseasefalls-short/, (arguing that labeling people who use drugs with a chronic brain disease is harmful, stigmatizing, and unsupported by science, which shows a majority of people labeled with addiction as improving on their own; and that, nevertheless, there is ample scientific evidence to support the benefits of scheduled medical treatment rather than a criminal justice response for those who need it); and Gene Heyman, A Disorder of Choice (Harvard University Press: Cambridge, 2010) (arguing that addiction should not be treated as a result of involuntary behavior, but that, rather, treating addiction as a result of voluntary behavior (choice) that results in poor long-term health outcomes provides a viable approach to the prevention and treatment of drug addiction). 36. BupPractice, “DSM 5 Criteria for Substance Use Disorder,” accessed March 30, 2017, http://www. buppractice.com/node/12351. 37. The American Association of Addiction Medicine (ASAM) has developed criteria to match the severity levels of substance use disorders with appropriate level of care. These criteria have been validated by medical researchers Marianne Stallvik and David R. Gastfriend, “Predictive and convergent validity of the ASAM criteria in Norway,” in Addict Res Theory, 2014; 22(6), pp. 515-23. 38. Antoine B Bouaihy, Thomas M. Kelly, and Carl Sullivan, “Medications for Substance Use Disorders,” Soc Work Public Health, 2013; 28(0) pp. 264-278, accessed April 12, 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC3767185/. 39. World Health Organization, “WHO Model List of Essential Medicines, April 2015 (amended November 2015),” (World Health Organization: Geneva, 2015), accessed on March 24, 2017, http://www.who.int/ medicines/publications/essentialmedicines/EML_2015_ FINAL_amended_NOV2015.pdf. 40. New Hampshire Center for Excellence, “Substance Use Disorder Treatment and Other Service Capacity in New Hampshire,” 2014. 41. New Hampshire Center for Excellence, “Substance Use Disorder Treatment and Other Service Capacity in New Hampshire,” 2014, pp. 28-30. 42. Bureau of Drug and Alcohol Services (BDAS), New Hampshire Center for Excellence, “2015-2016 Guidance Document on Best Practices: Key Components for Delivering Community-Based Medication-Assisted Treatment Services for Opioid Use Disorders in New Hampshire,” pp. 40. 43. PHR interviews with three drug court participants in Palatka, Putnam County, FL, on February 7, 2017. See also Opiate Addiction and Treatment Resource, “Methadone Clinics – Florida,” last updated October 2013, accessed April 10, 2017, http://www. opiateaddictionresource.com/treatment/methadone_ clinic_directory/fl_clinics. 44. James Mulder, “In Syracuse it’s easier for addicts to get heroin than medical treatment,” Syracuse.com, February 14, 2016, accessed April 12, 2017, http://www.syracuse. com/health/index.ssf/2016/02/heroin_main.html. 45. Substance Abuse and Mental Health Services Administration, “Apply to Increase Patient Limits,” last updated February 9, 2017, accessed April 14, 2017, https://www.samhsa.gov/medication-assistedtreatment/buprenorphine-waiver-management/increasepatient-limits. 46. PHR interview with Dr. Laura Martin, My Care Syracuse, Syracuse, NY, November 22, 2016. 47. PHR comparison of data. Certified prescriber data via Substance Abuse and Mental Health Services Administration, “Number of DATA-certified physicians,” accessed May 8, 2017, https://www.samhsa.gov/ medication-assisted-treatment/physician-program-data/ certified-physicians; population data via Statistica. com, accessed May 8, 2017; and drug use data via SAMHSA, Center for Behavioral Health Statistics and Quality, “Results from the 2015 National Survey on Drug Use and Health: Detailed Tables,” accessed March 7, 2017, https://www.samhsa.gov/data/sites/default/files/ NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUHDetTabs-2015.pdf. 48. A prescription medicine that contains buprenorphine and naloxone. 49. PHR interview with Alex Casale, state court coordinator, New Hampshire, December 6, 2016. 50. PHR interview with Richard, New York, August 25, 2016. 51. Cara Tabachnick, “Breaking Good: Vivitrol, a new drug given as a monthly shot, is helping addicts stay clean,” Washington Post, March 13, 2015, accessed on April 12, 2017, https://www.washingtonpost.com/lifestyle/ magazine/his-last-shot-will-a-monthly-jab-of-a-newdrug-keep-this-addict-out-of-jail/2015/03/05/7f0543547a4c-11e4-84d4-7c896b90abdc_story.html?utm_term=. c8ef46060ac3. 52. PHR interview with David Adan, clinical supervisor, Banyan Health Systems, Miami, February 17, 2017. 53. PHR interview with Shayanne, participant, Nashua drug court, Hillsborough County, New Hampshire, December 2, 2016. 54. PHR interview with Jim, residential treatment center, New York, August 25, 2016. 55. PHR interview with Richard, New York, August 25, 2016. 56. PHR interview with [name withheld], clinical director, [name withheld], New York, August 24, 2016. 57. PHR phone interview with Emma Ketteringham, Bronx Defenders, July 19, 2016. 58. OASAS, “Guidelines for Detoxification Triage,” at https:// www.oasas.ny.gov/admin/hcf/documents/detoxguide. pdf (accessed on May 23, 2017). 59. Benjamin R. Nordstrom and Frances R Levin, “Treatment of Cannabis Use Disorders: A Review of the Literature,” American Journal on Addictions, Volume 16, 2007, issue 5, accessed March 31, 2017, http://www.tandfonline. com/doi/figure/10.1080/10550490701525665. 60. PHR phone interview with Dr. Benjamin Nordstrom, Phoenix House, New York City, August 5, 2016; and with [name withheld], [clinic name withheld], New York, August 5, 2016. 61. World Health Organization, “WHO Model List of Essential Medicines, April 2015 (amended November 2015),” (World Health Organization: Geneva, 2015), accessed March 24, 2017, http://www.who.int/ medicines/publications/essentialmedicines/EML_2015_ FINAL_amended_NOV2015.pdf. Physicians for Human Rights phr.org 23 Endnotes continued 62. Harlan Matusow et al, “Medication assisted treatment in US drug courts: Results from a nationwide survey of availability, barriers, and attitudes,” in Journal of Substance Abuse Treatment, May-June 2013, Vol 44, issue 5, pp. 473-480. 63. Joanne Csete and Holly Catania (2013). “Methadone treatment providers’ views of drug court policy and practice: a case study of New York State,” Harm Reduction Journal 10:35, accessed February 24, 2017, http://www.harmreductionjournal.com/content/10/1/35. 64. Alison Knopf, “SAMHSA bans drug court grantees from ordering participants off MAT,” Alcoholism and Drug Abuse Weekly, February 16, 2015, accessed March 7, 2017, http://www.alcoholismdrugabuseweekly.com/ Article-Detail/samhsa-bans-drug-court-grantees-fromordering-participants-off-mat.aspx. 65. Alison Knopf, “SAMHSA bans drug court grantees from ordering participants off MAT,” Alcoholism and Drug Abuse Weekly, February 16, 2015, accessed March 7, 2017, http://www.alcoholismdrugabuseweekly.com/ Article-Detail/samhsa-bans-drug-court-grantees-fromordering-participants-off-mat.aspx. 66. Memorandum in support of bill S4239B, available at http://www.nysenate.gov/legislation/bills/2015/S4239B. 67. NY Crim. Proc. Law §§ 216.05(5) and (9)(a). 68. PHR letter to Judge Cele Hancock, dated February 7, 2017, on file with PHR. Only drug courts receiving federal funding are required to allow MAT, some statefunded grants are beginning to introduce new rules to require allowance of MAT in order to receive funding. 69. PHR interview with Danielle Gravina, MAT Case Manager, Queens Felony Treatment Court Enhanced Program, Queens Treatment Alternatives for Safe Communities, July 14, 2016. 70. Shannon Gwin Mitchell et al, “Incarceration and opioid withdrawal: The experiences of methadone patients and out-of-treatment heroin users,” Journal of Psychoactive Drugs, June 2009, Vol. 41(2), pp. 145-152, accessed March 31, 2017, https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC2838492/. 71. PHR interview with Hanif Rashid, court liaison with the Diversion and Treatment Program (DATP), Miami, FL, February 16, 2017. 72. PHR interview with Joanna Caldwell, risk and compliance manager, South Florida Behavioral Health Network, Miami, FL, February 17, 2017. 73. PHR interview with Dr. Thomas Robinson, psychologist, Jackson Hospital, Miami, FL, February 16, 2017. 74. PHR phone interview with Keith Brown, director, Law Enforcement Assisted Diversion, Albany, NY, July 15, 2016. 75. National Center for Addiction and Substance Abuse at Columbia University (CASA), “Addiction Medicine: Closing the Gap Between Science and Practice,” June 2012, pp. 172: “A survey of private health plans found that while only 16 percent of private insurance offering imposed lifetime limits on addiction treatment, 94 percent had annual limits on addiction treatment, and 89 percent had annual limits for inpatient services.” 76. Ben Allen, “How We Got Here: Treatment Addiction in 28 Days,” NPR Weekend Edition, October 1, 2016, accessed March 20, 2017, http://www.npr.org/sections/ health-shots/2016/10/01/495031077/how-we-got-heretreating-addiction-in-28-days. 77. PHR phone interview with Dr. Joshua D. Lee, assistant professor, NYU, attending physician, Bellevue hospital, New York City, March 30, 2017. Neither Justice Nor Treatment 78. PHR interview with [name withheld], assistant district attorney’s office, New York County, November 21, 2016. Note that Medicaid does not cover all treatment options for substance dependence, and that coverage varies by state. 79. PHR phone interview with Dr. Joshua D. Lee, assistant professor, NYU, attending physician, Bellevue hospital, New York City, March 30, 2017. 80. Colleen L. Barry and Haiden A. Huskamp, “Moving beyond parity—mental health and addiction care under the ACA,” New England Journal of Medicine 2011; 365(11), pp. 973-5; and Keith Humphreys and Richard G. Frank, “The Affordable Care Act will revolutionize care for substance use disorders in the United States,” in Addiction, 2014. 109 (12), pp. 1957-8. 81. HealthCare.gov, “Mental Health and Substance Abuse Coverage,” accessed April 10, 2017, https://www. healthcare.gov/coverage/mental-health-substanceabuse-coverage/. 82. National Center on Addiction and Substance Abuse at Columbia University, “Addiction Medicine: Closing the Gap Between Science and Practice,” June 2012, pg. 170, “Treatment for Addiction, Medicaid” ; Kaiser Family Foundation, “Medicaid Pocket Primer,” accessed on April 10, 2017, http://kff.org/medicaid/fact-sheet/medicaidpocket-primer/; Kristen Beronio, Rosa Po, Laura Skopec, and Sherry Glied, “Affordable Care Act Expands Mental Health and Substance Use Disorder Benefits and Federal Parity Protections for 62 Million Americans,” February 20, 2013, accessed February 24, 2017, https://aspe.hhs. gov/report/affordable-care-act-expands-mental-healthand-substance-use-disorder-benefits-and-federal-parityprotections-62-million-americans. 83. Tami Mark et al, “Medicaid coverage of medications to treat alcohol and opioid dependence,” Journal of Substance Abuse Treatment 2015 Aug, pp. 1-5. 84. Alison M. Diaper, Fergus D. Law, and Jan K. Melichar, “Pharmacological strategies for detoxification,” British Journal of Clinical Pharmacology, Feb 2014, Vol 77(2), pp. 302-314, accessed March 31, 2017, https://www. ncbi.nlm.nih.gov/pmc/articles/PMC4014033/; The National Center on Addiction and Substance Abuse, “Addiction Medicine: Closing the Gap between Science and Practice,” June 2012, CASA Columbia National Advisory Commission on Addiction Treatment, p. 107 “Chronic Disease Management,” accessed April 10, 2017, http://www.centeronaddiction.org/addiction-research/ reports/addiction-medicine-closing-gap-betweenscience-and-practice. 85. Kirstin P. Frescoln, “Engaging with the Affordable Care Act: Implications and Recommendations for Adult Drug Court Professionals,” National Association of Drug Court Professionals, May 2014, accessed March 20, 2017, http://www.ndcrc.org/sites/default/files/17673_nadcp_ ntk_aca_v2_2_2.pdf. 86. Kristen Beronio, Rosa Po, Laura Skopec, and Sherry Glied, “Affordable Care Act Expands Mental Health and Substance Use Disorder Benefits and Federal Parity Protections for 62 Million Americans,” February 20, 2013, accessed February 24, 2017, https://aspe.hhs.gov/ report/affordable-care-act-expands-mental-health-andsubstance-use-disorder-benefits-and-federal-parityprotections-62-million-americans. 87. PHR interview with Ed Fox, director, Project SafePoint, Albany, New York, August 26, 2016. 88. National Association of Drug Court Professionals, Best Practices Standards, p.5, accessed February 24, 2017, http://www.nadcp.org/sites/default/files/nadcp/ AdultDrugCourtBestPracticeStandards.pdf. 89. PHR interview with David Betancourt, public defender, Strafford county, New Hampshire, December 1, 2016. 90. PHR interview with [name withheld], prosecutor’s office, New York county, November 21, 2016. 91. PHR interview with Alex Parsons, Managing Defense Attorney, Cheshire County Drug Court, New Hampshire, December 8, 2016. 92. PHR interview with Dana Patterson, Alachua county drug court, Florida, February 9, 2017. 93. Drug Policy Alliance, “Drug Courts Are Not the Answer: Toward a Health-Centered Approach to Drug Use,” 2011, accessed April 10, 2017, https://www.drugpolicy. org/docUploads/Drug_Courts_Are_Not_the_Answer_ Final2.pdf; Justice Policy Institute, “Addicted to Courts: How a Growing Dependence on Drug Courts Impacts People and Communities,” March 2011, accessed April 10, 2017, http://www.justicepolicy.org/uploads/ justicepolicy/documents/addicted_to_courts_final.pdf. 94. PHR interview with [name withheld], prosecutor’s office, New York county, November 21, 2016. 95. PHR phone interview with Judge Tina Nadeau, Chief Justice, New Hampshire Supreme Court, July 26, 2016. 96. PHR phone interview with [name withheld], [clinic name withheld] August 5, 2016. PHR phone interview with Jose Villanueva, clinical manager, Camino Nuevo treatment center, Albany, New York, November 9, 2016. This point was repeated by several public defenders. PHR phone interview with Emma Ketteringham, Bronx Defenders, July 19, 2016; and PHR phone interview with Regina Tebrugge, attorney, Sarasota, June 8, 2016. 97. NADCP Best Practice Standards, “Incentives, Sanctions and Therapeutic Adjustments,” 2015, pp. 27-28. 98. Osceola County Participant Handbook, copy provided to PHR by Osceola County, FL on February 3, 2017; Orange County Participant Handbook, copy provided to PHR by Orange County, Florida, on February 6, 2017. 99. Putnam County Participant Handbook, last updated October 2016, accessed April 7, 2017, http://www. circuit7.org/Program%20and%20Services/Drug_Court_ Putnam_handbook.pdf. PHR observed the Putnam County drug court on February 7, 2017, but drug court staff declined to be interviewed for this report. 100. PHR interview with Judge James Carroll, Belknap county drug court, New Hampshire, December 6, 2016. 101. PHR interview with Stacey Lanza, former treatment provider, Phoenix House, Cheshire County, New Hampshire, December 8, 2016. 102. PHR interview with Asa Scott, senior clinical director and administrator of program development, Addiction Care Interventions, November 17, 2016. 103. All drug court participants waive doctor-patient confidentiality as a condition for participation in the drug court program. While legal under U.S. law, this does not take away from the seriousness of the privacy interference, nor does it follow that any discussion of personal drug use in open court contributes to relapse prevention or recovery. 104. See National Association of Drug Court Professionals, “Defining Drug Courts: The Key Components” (Washington, DC: U.S. Department of Justice, 1997), accessed March 31, 2017, http://www.ndci.org/sites/ default/files/nadcp/KeyComponents.pdf. 105. PHR phone interview with David Lucas, treatment coordinator, Toronto drug court, Canada, November 18, 2016. 106. PHR phone interview with David Lucas, treatment coordinator, Toronto drug court, Canada, November 18, 2016. Physicians for Human Rights phr.org 24 Endnotes continued 107. National Institute on Drug Abuse, “Drugs, Brains, and Behavior: The Science of Addiction,” July 2014, accessed July 25, 2016, https://www.drugabuse.gov/publications/ drugs-brains-behavior-science-addiction/treatmentrecovery (“The chronic nature of the disease means that relapsing to drug abuse at some point is not only possible, but likely.”); Jeanne L. Obert et al., “Client’s Handbook: Matrix Intensive Outpatient Treatment for People With Stimulant Use Disorders,” US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, 2006, accessed July 26, 2016, http://www.ct.gov/dmhas/lib/dmhas/pgs/ PGIntegratedMatrixClientHandbook.pdf. 108. Shelli B. Rossman, John K. Roman et al, “The Multi-Site Adult Drug Court Evaluation: The Impact of Drug Courts (Volume 4),” Urban Institute, Justice Policy Center, 2011, accessed March 14, 2017, http://www.courtinnovation. org/sites/default/files/documents/MADCE_4.pdf. 109. PHR interview with [name withheld], mental health coordinator and counselor at [name withheld], August 25, 2016. 110. PHR phone interview with Robert Gasser, former Grafton county drug court coordinator, July 18, 2016. 111. PHR interview with Connie Flagg, case manager, Cheshire county drug court, December 8, 2016. 112. PHR interview with Alex Casale, state drug court coordinator, New Hampshire, December 9, 2016. 113. PHR phone interview with Keith Brown, director, Albany Law Enforcement Assisted Diversion, July 15, 2016. 114. PHR phone interview with David Lucas, treatment coordinator, Toronto drug court, Canada, November 18, 2016. 115. For a thorough analysis of sentencing for drug-related offenses, including possession of minimal amounts of illicit drugs, see Human Rights Watch and the American Civil Liberties Union, “Every 25 Seconds: The Human Toll of Criminalizing Drug Use in the United States,” October 2016. 116. States have the possibility of modifying or opting out of this ban. Of the three states studied in this report, New York and New Hampshire have opted out of a lifetime ban on food stamps and cash assistance, and Florida imposes a modified ban. Eli Hager, “Six States Where Felons Can’t Get Food Stamps,” The Marshall Project, February 4, 2016, accessed March 10, 2017, https:// www.themarshallproject.org/2016/02/04/six-stateswhere-felonscan-t-get-food-stamps#.6zkAJf4qq. 117. See Federal Student Aid, “Students With Criminal Convictions,” (undated), accessed March 10, 2017, https://studentaid.ed.gov/sa/eligibility/criminalconvictions#drug-convictions. 118. Rebecca Vallas and Sharon Dietrich, “One Strike and You’re Out: How We Can Eliminate Barriers to Economic Security and Mobility for People with Criminal Records,” Center for American Progress, December 2014, accessed March 10, 2017, https://cdn. americanprogress.org/wpcontent/uploads/2014/12/ VallasCriminalRecordsReport.pdf. 119. American Civil Liberties Union, “State Criminal Reenfranchisement Laws (Map),” 2016, accessed March 10, 2017, https://www.aclu.org/map/state-criminal-reenfranchisement-lawsmap. 120. The Clemency Report, “Reefer sanity: States abandon driver’s license suspensions for drug offenses,” September 14, 2014, accessed March 10, 2017, http:// clemencyreport.org/drivers-license-suspensions-drugoffenses-state-state-list. Neither Justice Nor Treatment 121. PHR phone interview with Emma Ketteringham, Bronx Defenders, New York City, July 19, 2016. The point was reiterated by prosecutors and drug court coordinators in New Hampshire and Florida. Public defenders also preferred to refer prison-bound clients, rather than those with lesser sentences, to drug court because of the intensive, and sometimes invasive, nature of the drug court program. Public defenders said they often advised clients to serve jail sentences of less than a year in many cases, rather than sign up for drug court. 122. PHR phone interview with Emma Ketteringham, Bronx Defenders, New York City, July 19, 2016. 123. Fl. Stat. Title XXIX, Chapter 397, § 397.675. Similar laws exist in Kentucky, Ohio, and Indiana. 124. Fl. Stat. Title XXIX, Chapter 397, § 397.675. 125. PHR interview with Brian, Tampa, February 13, 2017. 126. PHR interview with Debra Thomas, clinical liaison, DACCO, Tampa, Florida, February 14, 2017. 127. PHR interview with Régent (Reggie) Champigny, mental health counselor, Greater Nashua Mental Health Center, Nashua, New Hampshire, December 2, 2016. 128. Dan Werb et al, “The effectiveness of compulsory drug treatment,” International Journal of Drug Policy 28 (2016), pp. 1-9. 129. See section below on human rights obligations and U.S. legal protections. 130. PHR interview with Dr. Todd Patton, medical director, El Rio, Osborne Association, New York City, October 25, 2016. 131. International Covenant on Civil and Political Rights (ICCPR), article 17. The ICCPR was ratified by the United States in 1992. The United States has not taken out any reservations or issued any declarations with regard to its understanding of the right to privacy under the Covenant. 132. Human Rights Committee, “General Comment No. 16: Article 17 “The Right To Privacy,” 1998, U.N. Doc. INT/ CCPR/CEC/662.E para. 4. 133. International Covenant on Economic Social and Cultural Rights (ICESCR), article 12. The ICESCR was signed by the United States in 1977. While signature to a treaty does not imply the same obligation of implementation as ratification or accession, it indicates a willingness to avoid violating the basic principles of the treaty. According to the Vienna Convention on the on Law of Treaties, article 18: “[a] State is obliged to refrain from acts which would defeat the object and purpose of a treaty when: (a) it has signed the treaty. …” 134. Committee on Economic Social and Cultural Rights, “General Comment 14, “The right to the highest attainable standard of health,” U.N. Doc E/C.12/2000/4 (2000), para. 12(b). 135. World Medical Association, Declaration of Lisbon on the Rights of the Patient, as revised in 2005 and reaffirmed in 2015, para. 8. 136. 42 CFR Part 2. 137. The confidentiality regulations set forth in 42 CFR Part 2 are not applicable to fully privatized substance use treatment centers. The majority of treatment centers that drug courts refer to are covered by these regulations. 138. The National Association of Drug Court Professionals appears keen to publicize this point in its guidance to drug court professionals. See, e.g., Bill Meyer, “Being a Legal Eagle: Confidentiality, Ethical, and Constitutional Requirements,” National Association of Drug Court Professionals, 2011, accessed March 17, 2017, http:// www.nadcp.org/sites/default/files/2014/CG-11.pdf. 139. 42 CFR Part 2, 2) Part 2 Restrictions, a. Disclosure; see also 45 CFR 164.512 (a), (e). 140. ICESCR, article 12 (the right to the highest attainable standard of health). Committee on Economic Social and Cultural Rights, “General Comment 14, The right to the highest attainable standard of health,” U.N. Doc E/C.12/2000/4 (2000), para. 8 (specifying the right to be free from non-consensual medical treatment). 141. ICCPR, article 9(1) (the right to liberty and security of person). 142. ICCPR, article 7 (the right not to be subjected to torture or to cruel, inhuman or degrading treatment or punishment, including, in particular, the right not to be subjected without their free consent to medical or scientific experimentation). 143. World Medical Association, Declaration of Lisbon on the Rights of the Patient, as revised in 2005 and reaffirmed in 2015, para. 3. 144. T. Pape, “Legal and ethical considerations of informed consent” Journal of the Association of perioperative Nurses 1997;65, pp. 1122-1127. 145. See e.g. In re Brown, 478 So.2d 1033, 1040 (Miss. 1985); and Cruzan v. Harmon, 760 S.W.2d 408, 417 (Mo. 1988). 146. World Medical Association, Declaration of Lisbon on the Rights of the Patient, as revised in 2005 and reaffirmed in 2015, para. 1(c). 147. International Working Group, “Dual loyalty and human rights in health professional practice: Proposed guidelines and institutional mechanisms,” PHR, 2002, at introduction. 148. International Working Group, “Dual loyalty and human rights in health professional practice: Proposed guidelines and institutional mechanisms,” PHR, 2002, p.12. 149. International Working Group, “Dual loyalty and human rights in health professional practice: Proposed guidelines and institutional mechanisms,” PHR, 2002, part II. Physicians for Human Rights phr.org Physicians for Human Rights phr.org For more than 30 years, Physicians for Human Rights (PHR) has used science and the uniquely credible voices of medical professionals to document and call attention to severe human rights violations around the world. A Nobel Peace Prize co-laureate, PHR employs its investigations and expertise to advocate for persecuted health workers and facilities under attack, prevent torture, document mass atrocities, and hold those who violate human rights accountable. Through evidence, change is possible. Nobel Peace Prize Co-laureate